| Case Report | ||
Open Vet J. 2023; 13(12): 1744-1751 Open Veterinary Journal, (2023), Vol. 13(12): 1744–1751 Case Report Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogsJon Andre Berg1,2* and Bente Kristin Sævik21Department of Preclinical Sciences and Pathology, Faculty of Veterinary Medicine, Norwegian University of Life Sciences, Ås, Norway 2AniCura Jeløy Dyresykehus, Moss, Norway *Corresponding Author: Jon Andre Berg. Department of Preclinical Sciences and Pathology, Faculty of Veterinary Medicine, Norwegian University of Life Sciences, Ås, Norway. Email: jon.andre.berg [at] nmbu.no Submitted: 18/07/2023 Accepted: 06/11/2023 Published: 31/12/2023 © 2023 Open Veterinary Journal
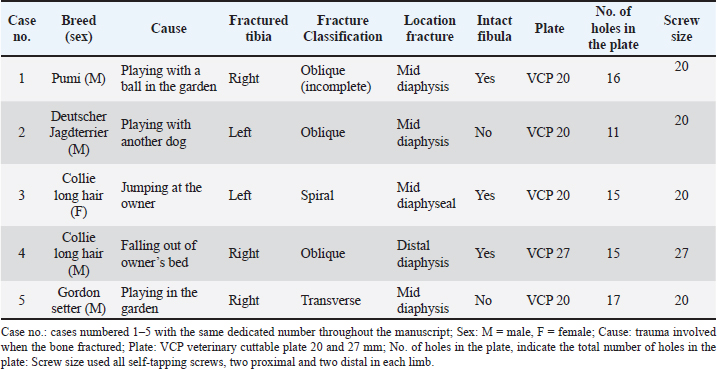
AbstractBackground: Pediatric fractures are relatively common in dogs, and several treatment options exist, particularly for fractures in the distal extremities. Regardless of the choice of treatment, the overall goal is rapid restoration and excellent long-term functional recovery, with minimal discomfort and morbidity during healing. This case series aims to report the long-term outcome after minimally invasive percutaneous elastic plate osteosynthesis (MIPEPO) in the treatment of pediatric tibial fractures in dogs and compare this to other treatment options, where all techniques emphasize biological osteosynthesis. We especially accentuate surgery time, patient comfort level during osteosynthesis, time to clinical union, and complications, including long-term follow-up. Case Description: Medical records of five skeletally immature (juvenile) dogs <6 months old with an isolated tibial diaphyseal fracture or a combination of tibial and fibular diaphyseal fractures, treated with MIPEPO aided by fluoroscopy. All dogs experienced excellent levels of comfort and limb functionality and exhibited preserved muscle mass throughout the healing process. The mean duration until plate removal was 27.6 days, with a standard deviation [(SD) ± 9.61; range of 15–36 days] following the operation. Subsequently, four dogs underwent a follow-up examination approximately 1.5 years after plate removal, during which bilateral orthogonal radiographs of the tibia were obtained. These radiographs revealed minimal discrepancies in terms of limb length, frontal plane alignment, and rotational alignment. Furthermore, the owners expressed complete satisfaction with their dogs’ recovery and restoration of intended function. Conclusion: MIPEPO is quick to perform and well tolerated, with rapid fracture healing in juvenile dogs and excellent long-term outcomes. It can be considered along with external fixators and external coaptation when dealing with juvenile diaphyseal fractures. Keywords: Dogs, Fluoroscopy, Fractures, Juvenile, Minimally invasive percutaneous elastic plate osteosynthesis. IntroductionPediatric fractures of the long bones in dogs are relatively common, where 20% of all long bone fractures in the immature skeleton are related to the tibia. Seventy-two percent of these fractures are diaphyseal (Boone et al., 1986; Unger et al., 1990). In addition, of all the fractures of the immature skeleton in dogs, 70% were in juvenile dogs less than 6 months of age (Kumar et al., 2007). The treatment of fractures in young dogs presents specific difficulties and necessitates additional factors for the veterinarian to consider. Juvenile dogs are inherently energetic, playful, and difficult to keep calm. Furthermore, they tend to chew on and gnaw at bandages, casts, and external fixators. The immature skeletal structure of juvenile dogs possesses unique qualities when compared to adult bones, both in terms of structure and function. The juvenile skeleton exhibits an active state of aerobic biologic condition, characterized by a high rate of cellular turnover and excellent blood supply (Carmichael, 1998; Piermattei et al., 2006), making these dogs potentially “healing machines.” Compared to an adult skeleton, the juvenile tibial cortex is thin, with low stiffness and strength, but highly ductile. The juvenile cortex is enveloped by a pliable, highly vascularized periosteal membrane, supporting the cortex as an external splint (Torzilli et al., 1981, 1982). However, this thin juvenile cortex has a low holding capacity for implants (Carmichael, 1998; Piermattei et al., 2006). For minimally displaced diaphyseal fractures in young individuals, the conventional approach involves using external coaptation, particularly for fractures in the lower limbs. However, an alternative technique called elastic plate osteosynthesis has been found to be effective in treating both femoral and tibial diaphyseal fractures. This method addresses the limited implant fixation capabilities of the immature skeleton (Cabassu, 2001; Sarrau et al., 2006). Other reported treatment options are external fixators, interlocking nails, hybrid variations of interlocking nails, and intramedullary pins in addition to external fixators (Shani and Shahar, 2002; Duhautois, 2003; Gemmill et al., 2004; Nanai and Basinger, 2005; Aronsohn and Burk, 2009). The purpose of this case series is to contribute to the limited existing literature on the management of juvenile diaphyseal tibial fractures in dogs. The focus is on discussing the minimally invasive percutaneous elastic plate osteosynthesis (MIPEPO) technique and comparing it to other treatment options for these fractures, with an emphasis on approaches that prioritize biological osteosynthesis as highlighted by Palmer (1999). Specifically, factors such as the duration of surgery, the level of patient comfort during the bone healing process, the time required for the clinical bone union to occur, any complications that may arise, and the long-term follow-up of the patients. In this context, a clinical bone union is defined as the presence of a bridging callus or a callus of 50% of the diameter of the tibia at the fracture site in three of four cortices on two orthogonal views (Guiot and Dejardin, 2010), and the point at which the fracture has sufficiently healed, for the implants to be safely removed. Case DetailsThe inclusion criteria for this study were complete medical records of dogs under 6 months old (juvenile) with a tibial diaphyseal fracture independently or combined with a diaphyseal fibular fracture (n =5), seen from April 2020 to July 2021 at AniCura Jeløy Dyresykehus in Norway. All dogs were client-owned, and the owners signed consent forms for the treatment; there was no need for additional ethical approval. All surgeries were implemented by the first author. Fractures were classified descriptively (Piermattei et al., 2006), and the fracture localization within the tibia diaphysis was approximated to the proximal, middle, and distal third. In addition, all cases were managed with fluoroscopically aided MIPEPO. The complete medical record was studied, including radiographic confirmation of bone union. Long-term follow-up (>12 months) (Cook et al., 2010) includes orthogonal bilateral radiographs of the tibia. The tibial lengths were measured bilaterally and compared according to Radasch et al. (2008). Alignment in the frontal plane was assessed by calculating the mechanical medial proximal tibial angle (mMPTA) and mechanical medial distal tibial angle (mMDTA) (Dismukes et al., 2007). The tibial varus-valgus angle (TVA) was calculated, where TVA=[mMPTA + mMDTA] − 180 (Guiot and Déjardin, 2011). Rotational alignment was subjectively described according to Guiot and Déjardin (2011), and complications were recorded according to Cook et al. (2010). All dogs were ASA score I and pre-medicated with methadone (Semfortan: Dechra Veterinary Products AS) 0.3 mg/kg intramuscularly (IM) in combination with acepromazine (Plegicil Vet: Pharmaxim AB) 0.01 mg/kg IM. One dog received fentanyl (Fentadon vet: Dechra Veterinary Products AS) 3 µg/kg/hour continuous rate infusion (CRI) in combination with acepromazine (Plegicil Vet: Pharmaxim AB) 0.01 mg/kg IM. In addition, all dogs received maropitant (Cerenia: Zoetis Animal Health AS) 1 mg/kg subcutaneous (SC) pre-operatively and meloxicam (Metacam vet: Boehringer Ingelheim Animal Health Nordics AS) 0.2 mg/kg SC. After induction with propofol (PropoVet Multidose: Zoetis Animal Health AS) 4 mg/kg intravenously (IV) anesthesia was maintained with sevoflurane (SevoFlo: Zoetis Animal Health AS) in 100% oxygen. The affected limb was clipped and aseptically prepared with 4% chlorhexidine gluconate (Hibiscrub; Regent Medical Limited, 40 mg/ml) and chlorhexidine spirit (Fresenius Kabi Norge, 5 mg/ml). The dogs were placed in dorsal recumbency with the affected limb hanging from a drip stand. Proximal and distal stab incisions were made medially on the skin, and the percutaneous plate (Cuttable Plates 1.5/2.0 or 2.0/2.7 mm: DePuy Synthes) (Table 1) was placed epiperiostealy from proximal to distal, in a previously bluntly dissected epiperiosteal soft tissue tunnel. The epiperiosteal tunnel was developed under the skin, by blunt dissection with a straight hemostatic forceps or a periosteal elevator, carefully sparing the medial saphenous artery and vein. The tunnel was extended from distal to proximal. Proximally the tendons of insertion of the sartorius, gracilis, and semitendinosus muscles were preserved (Hedequist and Sink, 2005; Beale and McCally, 2020). Precautions were taken to prevent interference with the proximal and distal physis (growth plates). To secure the plate, one self-tapping screw (DePuy Synthes) was used proximally, followed by manually reducing the fracture and performing spatial reconstruction, as described by Aron et al. (1995). The most distal self-tapping screw was then applied. The two screws were tightened, and the remaining self-tapping screws were placed in a similar manner, all done under the guidance of fluoroscopy. The screw holes were drilled with a battery-driven drill (Colibri II: DePuy Synthes). Screw sizes are given in Table 1. The stab incisions were closed with a simple cross stitch of 1.5 poliglecaprone 25 (Monocryl: Ethicon). Postoperative orthogonal radiographs confirmed satisfactory reduction and plate placement before the dogs were taken to the intensive care unit, where they were monitored during recovery from anesthesia. In addition, pain, temperature, and blood glucose were monitored until discharged. The following in-hospital postoperative medications were used for this purpose: meloxicam (Metacam vet: Boehringer Ingelheim Animal Health Nordics AS), 0.1 mg/kg orally once a day, methadone (Semfortan: Dechra Veterinary Products AS) 0.1–0.3 mg/kg (IM) or buprenorphine hydrochloride (Vetergesic vet: Orion Pharma Animal Health) 10 µg/kg (IM) or fentanyl (Fentadon vet: Dechra Veterinary Products AS) CRI 3 µg/kg/hour IV. The dogs were fed as soon as awake to prevent hypoglycemia. Table 1. Details regarding the dogs` breed, sex, cause of fracture, fracture side, classification and location, and whether the fibula was intact are given. The implants used are also outlined.
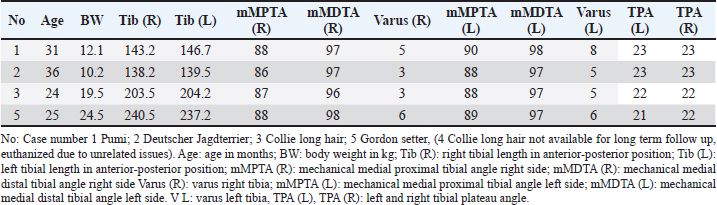
All dogs were ambulatory on the operated limb when discharged from the hospital, with a meloxicam prescription (Metacam vet: Boehringer Ingelheim Animal Health Nordics AS) 0.1 mg/kg once a day orally for 3–5 days. The owners were provided with specific, written instructions for strict postoperative restrictions, including keeping the dog on short leash walks and avoiding any play or jumping activities. A scheduled postoperative progress evaluation was planned, during which the clinical progress and radiographs would be assessed to determine if the plate removal was safe. Furthermore, the owners were advised to contact the clinic if they observed a lack of progress, deformity, or any pain related to the surgery. All dogs were re-examined approximately 4 weeks postoperatively, evaluating limb usage, pain, muscle mass, and joint alignment. In addition, the dogs were examined radiographically for bone healing progress and to confirm clinical bone union before plate removal. Lameness was graded at the walk on a scale of 0–4 (0: no lameness; 1: subtle weight-bearing lameness; 2: obvious weight-bearing lameness; 3: intermittent non-weight-bearing lameness; 4: consistent non-weight-bearing lameness). Long-term follow-up was available for four dogs, including clinic examination as well as bilateral orthogonal radiographs of the tibia. Moreover, the owners provided their subjective experience and evaluation of the overall outcome of the treatment. They categorized the outcome as excellent, indicating normal limb function; good, indicating slight lameness only after extensive exercise; fair, indicating slight-to-moderate lameness but consistent weight-bearing; or poor, indicating consistent non-weight-bearing lameness. Four males and one female of various breeds were included with a mean age of 15 weeks (SD ± 3.32 weeks; range 12–20 weeks) and a mean weight of 8.53, (SD ± 4.36 kg; range 4.6–15.6 kg). Fracture causes were all minor traumas (Table 1). Notably, all fractures were closed; details of fracture configurations can be seen in Table 1. Proximal and distal physis were open and considered within normal limits radiographically in all dogs, including the apophysis of the tibial tuberosity. The mean surgical time was 25.4 minutes (SD ± 6.69; range 15–33 minutes), while the mean hospital stay was 16.8 hours (SD ± 6.10; range 8–24 hours). Implant sizes are given in Table 1. At the initial re-examination, 15–36 days after the surgery, there were no signs of residual lameness, muscle atrophy, or any restrictions in the proximal and distal joints. In all five dogs, the tibial growth plates (physis) were still open at the time when bone healing was confirmed, and the implants were removed. The mean duration for implant removal was thus 27.6 days (SD ± 9.61; range 15–36 days). Four dogs were available for long-term follow-up (>12 months post plate removal) with a mean of 24.5 months (SD ± 11.70; range 15–40 months). Both clinical examination and owners’ assessment of the dog showed that there were no abnormalities. Assessment on the bilateral tibial length and frontal plane TVA were of minimal disparity, and there was no unacceptable tibial rotational malalignment (Table 2). In one case, case no. 4, a minor complication arose. There was a suspicion of post plate removal infection at the proximal stab incision. However, the bacteriological examination yielded negative results, and the clinical signs resolved after a 3-day treatment with local chlorhexidine swabs (Fresenius Kabi Norge, 1 mg/ml), used twice a day. DiscussionPublished studies on juvenile tibial diaphyseal fractures have reported a wide range of weights, varying from 3.53 to 17.55 kg (Gemmill et al., 2004; Sarrau et al., 2006; Aronsohn and Burk, 2009; Guiot and Déjardin, 2011) where the cases reported here fall into the same weight range of 4.6–15.6 kg. While male dogs, as reported here, seem to be overrepresented (Libardoni et al., 2016), breeds represented will mainly depend on the composition of the canine population in the local area of the clinic in question. Juvenile fractures, as reported in this study, frequently result from low-energy trauma (Zaal and Hazewinkel, 1997; Carmichael, 1998; Sarrau et al., 2006; Aronsohn and Burk, 2009; Deahl et al., 2017). The fractures reported herein were closed isolated tibial diaphyseal fractures (three cases) or combined with a fibular diaphyseal fracture (two cases) (Table 1). Fracture forces need consideration when the repair technique is assessed, while the intact fibula is reported to aid in torsional stability by acting as an internal splint (Galbraith et al., 2016). Considering other treatment options for juvenile tibial diaphyseal fractures, based on the philosophy of closed reduction and biological osteosynthesis, external coaptation is frequently mentioned. The advantages of external coaptation, such as casts or splints, are no implant-related infection or need for specialized equipment (Leighton, 1991; Oakley, 1999; Weinstein and Ralphs, 2004). Regarding cost, it will usually end up equal to the surgery cost if there are no complications. However, external coaptation can cause serious complications that will not only prolong the healing time and morbidity for the patient but also increase the cost of the treatment significantly (Tomlinson, 1991; Weinstein and Ralphs, 2004; Meeson et al., 2011). In addition, external coaptation needs to span the proximal and distal joints, with the possibility of atrophy of the articular cartilage and temporary joint stiffness (Leighton, 1991; Oakley, 1999). In addition, the use of external coaptation can hinder the dog’s ability to have a “normal” gait during the healing period. Moreover, juvenile dogs tend to chew or bite on external coaptations, which can compromise their effectiveness. Successful use of external coaptation requires a high level of owner compliance. In addition, the suitability of external coaptation may vary in different geographical areas due to local climates and environmental factors. External fixators type 1a have been used successfully to treat juvenile independent tibial diaphyseal fractures (Aronsohn and Burk, 2009). Gemmill et al. (2004) encountered loose pins in two dogs utilizing a 2b frame. The authors did not provide clarification regarding whether the fracture involved only the tibia or if it was a combination fracture involving the fibula. However, they did conclude that the stiffness of the frame, influenced by the weight of the dog, led to increased shear stress at the interface between the bone and pins when weight was applied. This resulted in elevated strain and premature loosening of the pins. External fixators have been associated with a high occurrence of complications and potential for adverse effects (Johnson et al., 1989; Gemmill et al., 2004). Some of the problems with the earlier designs have improved in terms of complication but not in time-to-frame removal (Johnson and Schaeffer, 2008). Another drawback with an external fixator is that it makes the dog walk with broader stans. Moreover, the external fixators can cause harm to the dog, owners and furniture. Table 2. Information about the age and weight of the dogs. Data on bilateral tibial length, mMPTA varus, mMDTA tibial angles, and the tibial plateau angle.
There have been reports on various treatment approaches for juvenile diaphyseal fractures in dogs, including the use of intramedullary devices in combination with external fixators, interlocking nails, and hybrids (Shani and Shahar, 2002; Duhautois, 2003; Nanai and Basinger, 2005). However, the use of intramedullary devices carries potential risks, such as damage to the cranial part of the proximal physis, which can lead to early closure and the development of abnormal tibial plateau angles. Currently, based on available information, it is advisable to avoid the use of intramedullary devices in the management of juvenile tibial diaphyseal fractures (Bjerkreim and Langård, 1983). Retrieving the device later in life may be challenging, and it appears to be an excessive amount of hardware for achieving the ultimate goal of rapid fracture healing, minimal discomfort for the animal, and excellent long-term functional outcomes. The surgery time reported in this study, with a mean of 25.4 minutes, is consistent with the reported times for type 1a external fixators (Aronsohn and Burk, 2009). Surgery time is crucial as it reduces the risk of infections, particularly when combined with a low ASA score (Nicholson et al., 2002; Eugster et al., 2004). In addition, it decreases the patient’s anesthesia time and overall cost (Nicholson et al., 2002). All the cases reported in this study had an ASA score of 1, and antibiotics were not used in these cases. There were no postoperative complications requiring antibiotics, except for a suspicious infection after plate removal, which was managed with local chlorhexidine swabs, and no aerobe bacterial growth was identified on bacteriological examination. The use of intraoperative and postoperative antibiotics in the treatment of juvenile dog fractures is not consistently reported in the literature (Cabassu, 2001; Peirone et al., 2002; Sarrau et al., 2006), while other publications do mention their use (Aronsohn and Burk, 2009; Cabassu, 2019). Considering the short surgery time, low ASA score, minimal surgical approach, relatively high oxygen tension at the fracture site, short hospital stay, and the global increase in antibacterial resistance, antibiotics may be unnecessary in these cases (Jian et al., 2021; Sjoberg et al., 2023). The use of fluoroscopy during MIPEPO offers several advantages. It provides illumination of the growth plate, facilitating the avoidance of spanning the physis during implant placement. Fluoroscopy also allows visualization of the fracture, plate, and their relationship, aiding in the spatial alignment of the bone (Hudson et al., 2009). However, it is important to note that fluoroscopy carries potential health hazards to the surgical team due to ionizing radiation, and measures should be taken to minimize exposure (FDA, 2020; Ojodu et al., 2018). It is worth mentioning that fluoroscopy is not mandatory for performing MIPEPO specifically related to the tibia (Cabassu, 2019). In this case series we defined bone clinical union according to Guiot and Déjardin (2011), which correspond to the time to implant removal, with a mean duration of 27.6 days. This is comparable to the results reported for the use of type 1a external fixators (Aronsohn and Burk, 2009), but shorter than the durations reported in other publications (Basinger and Suber, 2004; Gemmill et al., 2004; Sarrau et al., 2006; Guiot and Déjardin, 2011). It is important to recognize that clinical union precedes radiographic union, and the time to implant removal is based on individual veterinary surgeons’ interpretation of radiographic and clinical information (Gemmill et al., 2004). Two of the cases in this report were scheduled during the summer holiday period, and as a result, their plate removal surgeries were postponed by 1 week due to the owners and dogs being on vacation. It can be speculated that if these cases were not affected by the holiday, the time to implant removal could potentially have been reduced. However, it is important to note that in other publications reporting clinical bone union, the timing may be influenced by owners returning their dogs for follow-up evaluations. It is worth considering that the quicker the recovery, the sooner the dog can return to regular activity. The removal of implants is recommended in juvenile patients due to the potential for long-term morbidity when the implants become difficult to remove due to bone ingrowth (Abdelgawad et al., 2013; Piermattei et al., 2006). Regardless of the specific techniques used for reduction and fixation, achieving adequate length and alignment in all planes is crucial for functional recovery. In the cases presented in this study, long-term postoperative radiographs were taken to evaluate tibial length and alignment in both the frontal and sagittal planes. These radiographs showed only minor disparities between the left and right sides, well within the acceptable range for successful outcomes (Dismukes et al., 2007, 2008). The use of minimally invasive osteosynthesis (MIO) in fracture treatment has gained popularity in small animal surgery, with reported advantages including reduced surgical time, decreased infection rate, faster healing, and fewer complications (Schmökel et al., 2003, 2007; Hudson et al., 2009; Guiot and Déjardin, 2011; Mahbubur Rahman et al., 2017). However, direct comparisons between MIO and open surgical techniques are scarce in the field of small animal surgery (Dudley et al., 1997; Boero Baroncelli et al., 2012; Pozzi et al., 2013; Xu et al., 2015). Nevertheless, one study reported faster bone healing with MIO compared to open reduction and internal fixation (Pozzi et al., 2012). In this retrospective case series, excellent outcomes were achieved by employing MIPEPO for the management of independent tibial diaphyseal fractures or fractures combined with fibular diaphyseal fractures in five juvenile dogs. The dogs were able to bear weight on the operated limb within 24 hours after surgery, which is consistent with findings from a previous publication (Aronsohn and Burk, 2009). None of the dogs exhibited lameness at the first postoperative examination, and the range of motion in the joints proximal and distal to the fracture was comparable to the contralateral limb, with symmetrical muscle mass. The use of MIPEPO facilitated rapid clinical bone union while preserving limb function, and long-term follow-up indicated excellent outcomes with no major complications. In conclusion, although this retrospective case series has limitations, such as a small sample size and the absence of a control group, MIPEPO appears to be an effective and efficient technique for achieving rapid clinical bone union in juvenile tibial diaphyseal fractures in dogs. The technique provides benefits such as normal gait during the healing process and minimal maintenance for the owners. In addition, based on the findings of this study, the use of antibiotics in these cases seems unnecessary. Therefore, MIPEPO should be considered a viable option for treating juvenile tibial diaphyseal fractures in dogs. On the other hand, advanced training and purchasing specialized equipment like fluoroscopy are involved. AcknowledgmentCatrine Trangerud, DVM, PhD, for encouragement and evaluating the manuscript and Anicura Jeløy Dyresykehus for the support. Author contributionJon A. Berg: Carried out all pre-operative examinations, surgical interventions and postoperative evaluation of the patient. Contributed to the planning of the study, harvesting of data, analysis and interpretation of data as well as writing the manuscript. Bente K. Sævik: Conceptualized the cases and contributed to the writing process. Conflict of interestThe authors declare that there is no conflict of interest. FundingThis study was kindly supported by AniCura Jeløy Dyresykehus. Data availabilityData are available from the authors upon reasonable request. ReferencesAbdelgawad, A.A., Sieg, R.N., Laughlin, M.D., Shunia, J. and Kanlic, E.M. 2013. Submuscular bridge plating for complex pediatric femur fractures is reliable. Clin Orthop Relat Res. 471(9), 2797–2807. Aron, D.N., Johnson, A.L. and Palmer, R.H. 1995. Biologic strategies and a balanced concept for repair of highly comminuted long bone fractures. Compend. Contin. Edu. Pract. Vet. 17, 35–49. Aronsohn, M.G. and Burk, R.L. 2009. Unilateral uniplanar external skeletal fixation for isolated diaphyseal tibial fractures in skeletally immature dogs. Vet. Surg. 38(5), 654–658. Basinger, R.R. and Suber, J.T. 2004. Two techniques for supplementing interlocking nail repair of fractures of the humerus, femur, and tibia: results in 12 dogs and cats. Vet. Surg. 33(6), 673–680. Beale, B. and McCally, R. 2020. Minimally invasive fracture repair of the tibia and fibula. Vet. Clin. North. Am. Small. Anim. Pract. 50(1), 183–206. Bjerkreim, I. and Langård, Ø. 1983. Effect upon longitudinal growth of femur by intramedullary nailing in rats. Acta. Orthop. Scand. 54(3), 363–365. Boero Baroncelli, A., Peirone, B., Winter, M.D., Reese, D.J. and Pozzi, A. 2012. Retrospective comparison between minimally invasive plate osteosynthesis and open plating for tibial fractures in dogs. Vet. Comp. Orthopaed. Traumatol. 25(5), 410–417. Boone, E.G., Johnson, A.L., Montavon, P. and Hohn, R.B. 1986. Fractures of the tibial diaphysis in dogs and cats. J. Am. Vet. Med. Assoc. 188(1), 41–5. Cabassu, J.P. 2001. Elastic plate osteosynthesis of femoral shaft fractures in young dogs. Vet. Comp. Orthopaed. Traumatol. 14(1), 40–45. Cabassu, J. 2019. Minimally invasive plate osteosynthesis using fracture reduction under the plate without intraoperative fluoroscopy to stabilize diaphyseal fractures of the tibia and femur in dogs and cats. Vet. Comp. Orthopaed. Traumatol. 32(6), 475–482. Carmichael, S. 1998. Fracture in skeletally immature animals. In Manual of small animal fracture repair and managment. Eds., Coughlan, A. and Miller, A. Hampshire, UK: British Small Animal Veterinary Association, pp: 103–111. Cook, J.L., Evans, R., Conzemius, M.G., Lascelles, B.D.X., McIlwraith, C.W., Pozzi, A., Clegg, P., Innes, J., Schulz, K., Houlton, J., Fortier, L., Cross, A.R., Hayashi, K., Kapatkin, A., Brown, D.C. and Stewart, A. 2010. Proposed definitions and criteria for reporting time frame, outcome, and complications for clinical orthopedic studies in veterinary medicine. Vet. Surg. 39(8), 905–908. Deahl, L., Ben-Amotz, R., Caceres, A.V. and Agnello, K.A. 2017. Proximal tibial metaphyseal fractures in immature dogs. Vet. Comp. Orthopaed. Traumatol. 30(4), 237–242. Dismukes, D.I., Tomlinson, J.L., Fox, D.B., Cook, J.L. and Song, K.J.E. 2007. Radiographic measurement of the proximal and distal mechanical joint angles in the canine tibia. Vet. Surg. 36(7), 699–704. Dudley, M., Johnson, A.L., Olmstead, M., Smith, C.W., Schaeffer, D.J. and Abbuehl, U. 1997. Open reduction and bone plate stabilization, compared with closed reduction and external fixation, for treatment of comminuted tibial fractures: 47 cases (1980-1995) in dogs. J. Am. Vet. Med. Assoc. 211(8), 1008–1012. Duhautois, B. 2003. Use of veterinary interlocking nails for diaphyseal fractures in dogs and cats: 121 cases. Vet. Surg. 32(1), 8–20. Eugster, S., Schawalder, P., Gaschen, F. Boerlin, P. 2004. A prospective study of postoperative surgical site infections in dogs and cats. Vet. Surg. 33(5), 542–550. FDA. 2020. Fluoroscopy | FDA [WWW Document], 2020. U.S. Food & Drug Administration. Available via URL https://www.fda.gov/radiation-emitting-products/medical-x-ray-imaging/fluoroscopy (Accessed 3 September 2021). Galbraith, J.G., Daly, C.J., Harty, J.A. and Dailey, H.L. 2016. Role of the fibula in the stability of diaphyseal tibial fractures fixed by intramedullary nailing. Clin. Biomech. 38, 42–49. Gemmill, T.J., Cave, T.A., Clements, D.N., Clarke, S.P., Bennett, D. and Carmichael, S. 2004. Treatment of canine and feline diaphyseal radial and tibial fractures with low-stiffness external skeletal fixation. J. Small Anim. Pract. 45(2), 85–91. Guiot, L.P. and Déjardin, L.M. 2011. Prospective evaluation of minimally invasive plate osteosynthesis in 36 nonarticular tibial fractures in dogs and cats. Vet. Surg. 40(2), 171–182. Hedequist, D.J. and Sink, E. 2005. Technical aspects of bridge plating for pediatric femur fractures. J. Orthop. Trauma. 19(4), 276–279. Hudson, C.C., Pozzi, A. and Lewis, D.D. 2009. Minimally invasive plate osteosynthesis: applications and techniques in dogs and cats. Vet. Comp. Orthop. Traumatol. 22(3), 175–182. Jian, Z., Zeng, L., Xu, T., Sun, S., Yan, S., Yang, L., Huang, Y., Jia, J. and Dou, T. 2021. Antibiotic resistance genes in bacteria: occurrence, spread, and control. J. Basic. Microbiol. 61(12), 1049–1070. Johnson, A.L., Kneller, S.K. and Weigel, R.M. 1989. Radial and tibial fracture repair with external skeletal fixation: effects of fracture type, reduction, and complications on healing. Vet. Surg. 18(5), 367–372. Johnson, A.L. and Schaeffer, D.J. 2008. Evolution of the treatment of canine radial and tibial fractures with external fixators. Vet. Comp. Orthopaed. Traumatol. 21(3), 256–261. Kumar, K., Mogha, I. V., Aithal, H.P., Kinjavdekar, P., Amarpal, Singh, G.R., Pawde, A.M. and Kushwaha, R.B. 2007. Occurrence and pattern of long bone fractures in growing dogs with normal and osteopenic bones. J. Vet. Med. A Physiol. Pathol. Clin. Med. 54(9), 484–490. Leighton, R.L. 1991. Principles of conservative fracture management: splints and casts. Semin. Vet. Med. Surg. Small Anim. 6(1), 39–51. Libardoni, R., Serafini, G., Oliveira, C. and Rural, P.S.-C. 2016. Appendicular fractures of traumatic etiology in dogs: 955 cases (2004-2013). Ciênc. Rural. 46, 524–546. Mahbubur Rahman, M., Jeong, I.S. and Kim, N.S. 2017. Application of minimally invasive plate osteosynthesis to tibial shaft fractures in dogs. J. Vet. Clin. 34, 200–203. Meeson, R.L., Davidson, C. and Arthurs, G.I. 2011. Soft-tissue injuries associated with cast application for distal limb orthopaedic conditions: a retrospective study of sixty dogs and cats. Vet. Comp. Orthopaed. Traumatol. 24(2), 126–131. Nanai, B. and Basinger, R.R. 2005. Use of a new investigational interlocking nail supplement in the repair of comminuted diaphyseal tibia fractures in two dogs. J. Am. Anim. Hosp. Assoc. 41, 203–208. Nicholson, M., Beal, M., Shofer, F. and Brown, D.C. 2002. Epidemiologic evaluation of postoperative wound infection in clean-contaminated wounds: a retrospective study of 239 dogs and cats. Vet. Surg. 31, 577–581. Oakley, R.E. 1999. External coaptation. Vet. Clin. North. Am. Small. Anim. Pract. 29(5), 1083–1095. Ojodu, I., Ogunsemoyin, A., Hopp, S., Pohlemann, T., Ige, O. and Akinola, O. 2018. C-arm fluoroscopy in orthopaedic surgical practice. Eur. J. Orthopaed. Surg. Traumatol. 28(8), 1563–1568. Palmer, R.H. 1999. Biological osteosynthesis. Vet. Clin. North Am. Small. Anim. Pract. 29(5), 1175–1185. Peirone, B., Camuzzini, D., Filippi, D. and Valazza, A. 2002. Femoral and humeral fracture treatment with an intramedullary pin/external fixator tie-in configuration in growing dogs and cats. Vet. Comp. Orthopaed. Traumatol. 15, 85–91. Piermattei, D., Flo, G. and DeCamp, C. 2006. Fractures in growing animals. In Handbook of small animal ortopedics and fracture repair. Eds., Piermattei, D., Flo, G. and DeCamp, C. St. Louis, MO: Elsever, Saunders, pp: 728–737. Pozzi, A., Hudson, C.C., Gauthier, C.M. and Lewis, D.D. 2013. Retrospective comparison of minimally invasive plate osteosynthesis and open reduction and internal fixation of radius-ulna fractures in dogs. Vet. Surg. 42, 19–27. Pozzi, A., Risselada, M. and Winter, M.D. 2012. Assessment of fracture healing after minimally invasive plate osteosynthesis or open reduction and internal fixation of coexisting radius and ulna fractures in dogs via ultrasonography and radiography. J. Am. Vet. Med. Assoc. 241, 744–753. Radasch, R.M., Acvs, D., Lewis, D.F., Mcdonald, D.E., Calfee, E.F. and Barstad, R.D. 2008. Pes varus correction in Dachshunds using a hybrid external fixator. Vet. Surg. 37, 71–81. Sarrau, S., Meige, F. and Autefage, A. 2006. Treatment of femoral and tibial fractures in puppies by elastic plate osteosynthesis—a review of 17 cases. Vet. Comp. Orthopaed. Traumatol. 1, 51–58. Schmökel, H.G., Hurter, K. and Schawalder, R. 2003. Percutaneous plating of tibial fractures in two dogs. Vet. Comp. Orthopaed. Traumatol. 16, 191–195. Schmökel, H.G., Stein, S., Radke, H., Hurter, K. and Schawalder, P. 2007. Treatment of tibial fractures with plates using minimally invasive percutaneous osteosynthesis in dogs and cats: Paper. J. Small. Anim. Pract. 48, 157–160. Shani, J. and Shahar, R. 2002. The unilateral of external fixator and acrylic connecting bar, combined with I.M pin, for the treatment of tibial fractures. Vet. Comp. Orthopaed. Traumatol. 15, 104–110. Sjoberg, A.M., Fellman, C.L., DeStefano, I.M., Langfitt, S.M., Stein, M.R., Kwong, M., Beaulac, K. and Doron, S. 2023. One Health interprofessional stewardship to combat antimicrobial resistance. Nat. Med. 29(3), 512–513; doi:10.1038/S41591-022-02173-8 Tomlinson, J. 1991. Complications of fractures repaired with casts and splints. Vet. Clin. North. Am. Small. Anim. Pract. 21(4), 735–744. Torzilli, P.A., Takebe, K., Burstein, A.H. and Heiple, K.G. 1981. Structural properties of immature canine bone. J. Biomech. Eng. 103, 232–238. Torzilli, P.A., Takebe, K., Burstein, A.H., Zika, J.M. and Heiple, K.G. 1982. The material properties of immature bone. J. Biomech. Eng. 104, 12–20. Unger, M., Montavon, P.M. and Heim, U.F.A. 1990. Classification of fractures of long bones in the dog and cat: introduction and clinical application. Vet. Comp. Orthopaed. Traumatol. 03, 41–50. Weinstein, J. and Ralphs, S.C. 2004. External coaptation. Clin. Tech. Small Anim. Pract. 19, 98–104. Xu, H., Xue, Z., Ding, H., Qin, H. and An, Z. 2015. Callus formation and mineralization after fracture with different fixation techniques: minimally invasive plate osteosynthesis versus open reduction internal fixation. PLoS One 10, e0140037. Zaal, M.D. and Hazewinkel, H.A.W. 1997. Treatment of isolated Tibial fractures in cats and dogs. Vet. Quart. 19(4), 191–194. | ||
| How to Cite this Article |
| Pubmed Style Berg JA, Sævik BK. Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs. Open Vet J. 2023; 13(12): 1744-1751. doi:10.5455/OVJ.2023.v13.i12.23 Web Style Berg JA, Sævik BK. Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs. https://www.openveterinaryjournal.com/?mno=161615 [Access: May 13, 2024]. doi:10.5455/OVJ.2023.v13.i12.23 AMA (American Medical Association) Style Berg JA, Sævik BK. Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs. Open Vet J. 2023; 13(12): 1744-1751. doi:10.5455/OVJ.2023.v13.i12.23 Vancouver/ICMJE Style Berg JA, Sævik BK. Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs. Open Vet J. (2023), [cited May 13, 2024]; 13(12): 1744-1751. doi:10.5455/OVJ.2023.v13.i12.23 Harvard Style Berg, J. A. & Sævik, . B. K. (2023) Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs. Open Vet J, 13 (12), 1744-1751. doi:10.5455/OVJ.2023.v13.i12.23 Turabian Style Berg, Jon Andre, and Bente Kristin Sævik. 2023. Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs. Open Veterinary Journal, 13 (12), 1744-1751. doi:10.5455/OVJ.2023.v13.i12.23 Chicago Style Berg, Jon Andre, and Bente Kristin Sævik. "Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs." Open Veterinary Journal 13 (2023), 1744-1751. doi:10.5455/OVJ.2023.v13.i12.23 MLA (The Modern Language Association) Style Berg, Jon Andre, and Bente Kristin Sævik. "Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs." Open Veterinary Journal 13.12 (2023), 1744-1751. Print. doi:10.5455/OVJ.2023.v13.i12.23 APA (American Psychological Association) Style Berg, J. A. & Sævik, . B. K. (2023) Minimally invasive percutaneous elastic plate osteosynthesis as a treatment option for tibial diaphyseal fracture in skeletally immature dogs. Open Veterinary Journal, 13 (12), 1744-1751. doi:10.5455/OVJ.2023.v13.i12.23 |