| Case Report | ||
Open Vet J. 2023; 13(10): 1379-1384 Open Veterinary Journal, (2023), Vol. 13(10): 1379–1384 Case Report Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case reportAndrea Kashani-Carver1*, Gemma Turner1, Gisela Escalada Cáliz1, Amna Salih1, Casey Jordan2, Prado Cebrian1 and Robert Lowe11Optivet Referrals, 3 Downley Road, Havant, PO9 2NJ, UK 2Melbourne Eye Vet, 9-11 Miles Street, Mulgrave 3170, Australia *Corresponding Author: Andrea Kashani-Carver. Optivet Referrals, Havant, UK. Email: Andrea [at] Optivet.com Submitted: 04/08/2023 Accepted: 27/09/2023 Published: 31/10/2023 © 2023 Open Veterinary Journal
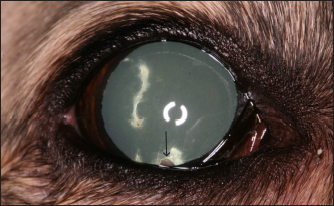
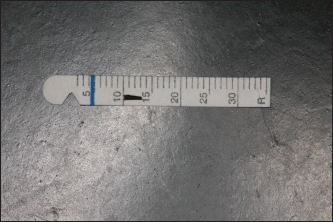
AbstractBackground: Intra-lenticular foreign bodies are rare in veterinary medicine and uncommon in human medicine. Approximately 50% of perforating ocular injuries in canines have lenticular involvement. Treatment choices include conservative management and surgical options. Retained intra-lenticular foreign body with delayed removal has not been reported in animals. Case Description: A 3-year-old male neutered Lurcher presented with right-sided ocular discomfort and a sealed full-thickness corneal perforation. The full ophthalmic examination could not be performed at the initial presentation due to miosis. Recrudescence of anterior uveitis was seen post-drug cessation. Re-evaluation of the eye with a mydriatic pupil revealed an intra-lenticular foreign body. Surgical removal via phacoemulsification was performed 8 weeks after the initial perforating injury. The eye remains visual, comfortable, and normotensive 50 months post-operatively. Conclusion: This is the first report of an encapsulated, retained intra-lenticular foreign body with delayed removal in a dog. Mydriasis and repeat examinations are of crucial importance when evaluating eyes post-perforation. Keywords: Intraocular foreign body, Intralenticular foreign body, Phacoclastic uveitis, Cataract. IntroductionSuspected corneal foreign body trauma is a common presentation to referral veterinary ophthalmologists, with 45% of cases involving the lens (Tetas Pont et al., 2016). Management options for intraocular foreign bodies vary due to the variety of clinical presentations, including the type of foreign material, location in the eye, the time frame between presentation and initial injury, damage caused along the path of penetration, and whether successful removal of the foreign body is possible (Grahn et al., 1995). Treatment options range from conservative medical therapies to surgery for foreign body removal and surgical repair or enucleation if irreversible damage or complications have occurred. Intraocular foreign bodies with lenticular involvement can be managed medically or surgically. Treatment depends on the case presentation, size of the lens capsule tear, presence of extrusion of cortical material, or the possibility of septic implantation syndrome (Gelatt, 1974; Bell et al., 2013). Phacoemulsification has been previously recommended when an anterior lens capsular tear exceeds 1.5 mm (Davidson et al., 1991); however, more recent literature has shown that medical management achieves similar outcomes (Paulsen and Kass, 2012). Intraocular foreign bodies with severe lens involvement have a poorer prognosis compared to those within the cornea or anterior chamber (Tetas Pont et al., 2016). Common complications that contribute to treatment failure include cataract development, phacoclastic uveitis, panophthalmitis, and secondary glaucoma (Bussanich and Rootman, 1981; Grahn et al., 1995; Bell et al., 2013; Tetas Pont et al., 2016). Retention of intralenticular foreign bodies has been reported to increase the likelihood of treatment failure in humans (Lee and Briner, 1996). The risk for complications increases with duration of retention, severity of capsule tear, presence of infection, and degree of damage caused to other ocular structures (Lee and Briner, 1996). To the best of our knowledge, no reports exist of the successful removal of a chronic lenticular foreign body in a dog. This case report describes the clinical presentation, diagnosis, management, and successful long-term outcome after the surgical removal of a retained intralenticular foreign body in a dog. Case DetailsHistoryA 3-year-old male neutered Lurcher presented for investigation of ongoing ocular discomfort following a full-thickness corneal perforating injury to the right eye 10 days prior. Ophthalmic examinationA complete ophthalmic examination was performed by an ECVO resident and ECVO board-certified diplomate. On distant examination, blepharospasm and epiphora were noted in the right eye. Neurophthalmic examination revealed intact palpebral reflex, menace response, and dazzle reflex bilaterally. The right pupil was miotic compared to the left. Slit-lamp biomicroscopy was performed (Kowa SL-17, Kowa Optimed Europe Ltd, Berkshire, UK) and revealed a re-epithelialised 9 mm linear, full-thickness corneal lesion in the latero-paraxial cornea of the right eye. Iris rests were seen on the corneal endothelium behind the lesion. No foreign bodies were noted in the cornea nor in the anterior chamber. There was a mild, cellular, aqueous flare. The intraocular pressure (IOP) was measured using rebound tonometry (iCare Tonovet, iCare, Vantaa, Finland) and was 5 and 17 mmHg in the right and left eye, respectively. The pupil did not fully dilate in response to multiple applications of the mydriatic agent tropicamide (Minims tropicamide 1%, Bausch and Lomb, UK), and as such, peripheral examination of the lens could not be performed. Of the lens that was examinable, there were no abnormalities seen. Anterior exudative uveitis was diagnosed secondary to a previous full-thickness corneal perforation. The left eye had a normal ophthalmic examination. Medical managementTopical treatment was instigated with chloramphenicol (Clorogen, 0.5%, FDC International Ltd, UK) every 6 hours, dexamethasone phosphate (Maxidex 0.1%, Novartis, UK) every 12 hours, and a topical cycloplegic, atropine sulfate (Minims atropine sulfate 1%, Bausch and Lomb, UK) every 24 hours for 5 days. Systemic anti-inflammatories were started concurrently: meloxicam (Loxicom, Norbrook, UK) 0.1 mg/kg per os q24 hours until review. Clinical remission of the uveitis, as evidenced by normalization of IOP and absence of aqueous flare, was achieved within a week, and medications were tapered down and stopped over the subsequent 2 weeks. Six weeks following the initial trauma and 3 weeks after cessation of medication, the patient was re-presented with a red and painful right eye. Ophthalmic examination revealed an incipient anterior and posterior capsular and subcapsular cataract in the right eye. Anterior non-exudative uveitis was present. The IOP was 8 and 20 mmHg in the right and left eye, respectively. Gonioscopy was performed in the right eye using an 18 mm Koeppe goniolens (Goniolens, Eickemeyer, Surrey, UK), which did not reveal additional abnormalities. Medical management was re-started with topical anti-inflammatories: prednisolone acetate eye drops (Pred Forte 1%, Allergan, Marlow, UK) to the right eye q8 hours and oral anti-inflammatories: meloxicam (Loxicom, Norbrook, UK) 0.1 mg/kg per os q24 hours until review. On re-examination 2 weeks later, the right eye presented with blepharospasm, increased blink frequency, and reflex lacrimation. Complete mydriasis was achieved during the consultation with tropicamide (Minims tropicamide 1%, Bausch and Lomb, UK), facilitating full examination of the lens periphery, revealing an intralenticular foreign body associated with a progressive incipient cortical cataract at the 6 o’clock position (Fig. 1). An ocular ultrasound (M9 portable ultrasound machine, Mindray, Huntingdon, UK), using the linear array probe in B-mode was performed prior to surgery, which confirmed the presence of the intralenticular foreign body and cataract. Surgical managementPhacoemulsification was performed in the right eye by an RCVS specialist in ophthalmology with a two-handed approach in a routine manner with no complications. The foreign body was successfully removed via the main port, and an artificial intra-ocular lens was inserted (Univers 41D 4 mm flexible IOL, Dioptrix, Toulouse, France). The foreign body grossly appeared to be a 3.5 mm piece of organic plant material (Fig. 2). Culture of the cataractous material revealed no aerobic bacterial or fungal growth; however, there was a light growth of anaerobic Gram-positive rods (further speciation was not performed by the laboratory). The anaerobic Gram-positive rods were found to be sensitive to metronidazole, amoxicillin-clavulanate, chloramphenicol, clindamycin, and cephalosporins. Post-operative management comprised of: cephalexin (Cephacare, Animalcare, York, UK) 15 mg/kg per os q12 hours, meloxicam (Loxicom, Norbrook, UK) 0.1 mg/kg per os q24 hours, chloramphenicol eye drops (Clorogen 0.5%, FDC International, Fareham, UK) to the right eye q6 hours, brinzolamide eye drops (Azopt 1%, Alcon, Birmingham, UK) to the right eye q8 hours, prednisolone acetate eye drops (Pred forte 1%, Allergan, Marlow, UK) to the right eye q4 hours and sodium hyaluronate eye drops (Clinitas 0.4%, Altacor, Berkshire, UK) to both eyes q6 hours.
Fig. 1. A photograph of the right eye showing a linear, full-thickness, sealed perforation in the latero-paraxial cornea. An incipient cataract and associated intralenticular foreign body are present at the 6 o’clock position (arrow).
Fig. 2. Foreign body removed from inside the lens capsule. Post-operative outcomesAt 50 months following surgery, the eye remained visual and comfortable with normal IOP and no evidence of uveitis. DiscussionThis case report highlights the importance of further investigation in cases with protracted uveitis, incomplete mydriasis on examination, and a known history of full-thickness corneal perforation. Identification of an intralenticular foreign body is of vital importance due to the potential sequelae if it remains in the eye; phacoclastic uveitis, secondary glaucoma, and septic implantation syndrome (Gelatt, 1974; Tetas Pont et al., 2016). A complete ophthalmic examination, including pupillary dilation and gonioscopy to assess the ICA for possible retained foreign material, is warranted. A complete ophthalmic examination can only be performed after complete mydriasis is achieved. Incomplete mydriasis can lead to areas of the posterior segment (peripheral lens and peripheral retina) not being fully examined. Miosis can preclude full examination of the eye. Miosis is a known consequence of anterior uveitis and can be caused by direct damage to the cells of the uvea by biological, chemical, or physical insults (Håkanson and Forrester, 1990; van der Woerdt, 2001). Once the cell has been damaged, arachidonic acid is released from phospholipids present in cell membranes via the enzyme phospholipase A2. The arachidonic acid enters the cyclooxygenase pathway and is converted into thromboxane and prostacyclin (potent prostaglandins). Direct action of these prostaglandins on the iris sphincter and ciliary body causes miosis and ciliary body spasm, respectively (Håkanson and Forrester, 1990; van der Woerdt, 2001). This direct action by prostaglandins on the iris sphincter can be difficult to overcome with topical mydriatics and can prevent full mydriasis from being achieved when acute active anterior uveitis is present. Re-examination, once full mydriasis has been achieved, is of vital importance due to the ability of a mid-dilated pupil to obscure visualization of the periphery of the lens and retina. Topical atropine can be used two to four times daily until full pupillary dilation is achieved (van der Woerdt, 2001). Atropine has effects on both pupil dilation (via its effect on the ciliary body causing cycloplegia and relieving ciliary spasm) and on the stabilization of the blood-aqueous barrier; however, care must be taken in animals with tear film deficiencies due to the decrease seen in tear production of animals receiving topical atropine (Ludders and Heavner, 1979; Margadant et al., 2003). IOP must also be closely monitored due to the potential for exacerbating increases in IOP and potential precipitation of glaucoma (Kovalcuka et al., 2015). On application, it can cause salivation due to the bitter taste, and care should be taken as systemic absorption of the drug can lead to an increase in heart rate (Greenberg et al., 2015). Cases of corneal perforation with suspicion of a retained foreign body that is not responding well despite appropriate medical management should be re-evaluated. In this case, the recurrence of uveitis upon cessation of topical anti-inflammatories indicated potential phacoclastic uveitis (Wilcock and Peiffer Jr, 1987), and that further examination was warranted. Gonioscopy is of importance for two reasons: first, to help predict the likelihood of the development of secondary glaucoma, and second, to identify small foreign bodies that may become trapped within the ICA (Tetas Pont et al., 2016). This is highlighted in a previous large retrospective study of corneal and anterior segment foreign bodies, in which an intraocular thorn was identified in the ICA using gonioscopy 7 months after the initial injury (Tetas Pont et al., 2016). Imaging is of vital importance in eyes with a history of, or presentation with, a foreign body. B-mode ultrasonography using a linear or sector transducer probe and frequencies of 7.5–12.5 MHz can be utilized when full dilation cannot be achieved in order to image the full globe and peri-ocular tissues (Cho, 2021). Depending on the machine and probe, images of varying quality can be acquired, and information pertaining to lenticular involvement and capsular integrity can be gained. It is easy to perform, does not require general anesthesia, and results can be attained rapidly and in real time. Smaller foreign bodies may not be easily identified using a lower frequency probe, and therefore, a foreign body cannot be excluded even after an ultrasound examination of the eye. High-resolution ultrasound (HRUS) or ultrasound biomicroscopy (UBM) can provide higher-quality images of the ICA, ciliary cleft as well as lens periphery that may not be visible on slit lamp biomicroscopy (Bentley et al., 2003). The advantages of HRUS and UBM include their suitability for conscious or lightly sedated patients and their capacity to acquire higher-resolution images compared to B-mode ultrasonography. This enables them to potentially identify smaller abnormalities more effectively (Bentley et al., 2003). Other imaging modalities, such as magnetic resonance imaging (MRI) and computed tomography (CT) can be used; however, there are limitations. An MRI is contraindicated in suspected metallic magnetic foreign body cases, but these are rarely reported in veterinary literature (Tetas Pont et al., 2016). CT would be the safest next step for investigating patients with a high suspicion of an intra-ocular foreign body; however, general anesthesia is often required, and these imaging modalities are less readily available (Saeed et al., 2008). Furthermore, the presence of higher water content in organic foreign bodies, such as wood or plant material, would make the visualization of these difficult on CT scans. In the veterinary literature, there are few reports of intraocular foreign bodies and rare reports of intralenticular foreign bodies. Schmidt et al. (1975) reported two cases of lead bullet intralenticular foreign bodies, of which both developed cataracts; one case developed a mature cataract and was followed for 7 months post-operatively, and the other case was lost to follow-up 3 weeks after initial presentation. Neither case had a comfortable visual eye upon final assessment. Bussanich and Rootman (1981) reported a single case of a migrating grass awn that penetrated the posterior sclera and led to retinal detachment, panophthalmitis, and enucleation. The lens was unaffected in this case; however, the eye could not be saved. Grahn et al. (1995) reported a case that had lens disruption secondary to perforation with a porcupine quill; the dog developed phacoclastic uveitis, secondary glaucoma, and the eye was later enucleated. More recently, Marchegiani et al. (2017) reported a case of a penetrating palpebral grass awn in a dog, which was removed surgically; in this case, the globe was unaffected. In the human literature, ocular foreign bodies are most commonly metallic and found in young-to-middle-aged male industrial workers (Greven et al., 2000; Dhawahir-Scala and Kamal, 2005; Peate, 2007; Luo and Gardiner, 2010). Due to the scarcity of published cases in veterinary medicine, a predilection has yet to be elucidated; however, a recent study identified a predisposition towards young working dogs, with English Springer Spaniels and Labrador Retrievers being six times and one and a half times more likely, respectively, to have a corneal or anterior chamber foreign body compared to other breeds (Tetas Pont et al., 2016). In humans, the prevalence of intralenticular foreign bodies following full-thickness ocular penetration is around 5%–10% (Coleman et al., 1987; Dhawahir-Scala and Kamal, 2005). In dogs lens, involvement was seen in 45% of cases with perforating foreign body trauma (Tetas Pont et al., 2016). This difference is likely due to species differences in behavior and the use of protective eyewear in humans. In human literature, the current recommendations are conservative management of intralenticular foreign bodies until intraocular inflammation, cataract formation, or siderosis bulbi develop (Lee and Briner, 1996; Dhawahir-Scala and Kamal, 2005). In the veterinary literature, the removal of intra-lenticular foreign bodies is recommended when the anterior lens capsule tear is >1.5 mm with cortical lens extrusion or uveitis, which persists despite treatment (Davidson et al., 1991). However, the majority of cases with lens involvement in the literature were conservatively managed due to the minimal damage to the lens and lack of a retained intra-lenticular foreign body (Paulsen and Kass, 2012; Tetas Pont et al., 2016). In humans, the most common material for ocular foreign bodies is metal (Luo and Gardiner, 2010), with reports of long-term retention seen for up to 60 years (Dhawahir-Scala and Kamal, 2005). In dogs, the most common material for ocular foreign bodies is organic plant material, with no reports of a metallic foreign body in a recent large retrospective study (Tetas Pont et al., 2016). Foreign bodies comprised of organic material, such as wood and plant material, are more likely to cause endophthalmitis when compared to inert, non-reactive, inorganic foreign bodies such as lead or plastic (Lit and Young, 2002; Mester and Kuhn, 2002). Metallic foreign bodies, such as copper and iron, can cause toxic damage to intra-ocular structures via oxidation of the metal, leading to the creation of free oxygen radicals, which can also lead to the initiation of the inflammatory cascade within the eye (Carter and Blevins, 1970; Schmidt et al., 1975). With inert foreign bodies, favorable outcomes can be seen with conservative management only (Marchegiani et al., 2017). The composition of the foreign body material can affect treatment outcomes. Wood structures are porous in nature, leading to an increased risk of harboring bacterial and fungal organisms and catastrophic complications such as endophthalmitis or septic implantation syndrome (Tite et al., 2002). In this case, the patient did not develop endophthalmitis or septic implantation syndrome despite the presence of a high-risk foreign body and culture of anaerobic Gram-positive bacilli. Repeat aqueocentesis sampling for culture was not performed after cessation of topical and oral antibiotics; this would have confirmed clearance of the bacteria cultured from the surgical sample. In this case, earlier identification of the foreign body could have been facilitated through ultrasound at the initial presentation; this would have led to a faster diagnosis. Wood foreign bodies, such as the thorn in this case, would show as a hyperechoic structure with acoustic shadowing (Hartley et al., 2007). To the best of the authors’ knowledge, this is the first reported case of a chronic, encapsulated intralenticular foreign body removed from the eye of a dog with a successful outcome and a visual, normotensive eye 50 months post-operatively. AcknowledgmentsThe authors would like to thank Natalia Escanilla Medina for her assistance and guidance in this case. Conflict of interestThe authors have no conflict of interest to declare. FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Author contributionsAndrea Kashani-Carver: Main author of the paper. Gemma Turner: Co-author of paper. Gisela Escalada Cáliz: Prepared literature review. Amna Salih: Reviewed manuscript. Casey Jordan: Helped prepare the manuscript and review process. Prado Cebrian: Ophthalmologist on the case, helped review the manuscript. Robert Lowe: Surgeon on the case and supervisor to the main author. Data availabilityThe authors confirm that the data supporting the findings of this study are available within the article. ReferencesBell, C.M., Pot, S.A. and Dubielzig, R.R. 2013. Septic implantation syndrome in dogs and cats: a distinct pattern of endophthalmitis with lenticular abscess. Vet. Ophthalmol. 16(3), 180–185. Bentley, E., Miller, P.E. and Diehl, K.A. 2003. Use of high-resolution ultrasound as a diagnostic tool in veterinary ophthalmology. J. Am. Vet. Med. Assoc. 223(11), 1617–1622, 1599. Bussanich, M. and Rootman, J. 1981. Intraocular foreign body in a dog. Can. Vet. J. 22(7), 207. Carter, J. and Blevins, W. 1970. Intraocular copper retention (chalcosis) in a dog: a case report. J. Small. Anim. Pract. 6, 28–36. Cho, J. 2021. Ocular ultrasound abnormalities and optic nerve sheath diameter in dogs and cats. Vet. Clin. North. Am. Small. Anim. Pract. 51(6), 1295–1314. Coleman, D.J., Lucas, B.C., Rondeau, M.J. and Chang, S. 1987. Management of intraocular foreign bodies. Ophthalmology 94(12), 1647–1653. Davidson, M.G., Nasisse, M.P., Jamieson, V.E., English, R.V. and Olivero, D.K. 1991. Traumatic anterior lens capsule disruption. J. Am. Anim. Hosp. Assoc. 27, 410–414. Dhawahir-Scala, F.E. and Kamal, A. 2005. Intralenticular foreign body: a D-Day reminder. Clin. Exp. Ophthalmol. 33(6), 659–660. Gelatt, K. 1974. Organic corneal foreign bodies in the dog. Vet. Med. Small. Anim. Clin. 69(11), 1423–1428. Grahn, B.H., Szentimrey, D., Pharr, J.W., Farrow, C.S. and Fowler, D. 1995. Ocular and orbital porcupine quills in the dog: a review and case series. Can. Vet. J. 36(8), 488–493. Greenberg, S., Plummer, C., Maisenbacher, H., Friary, J. and Berg, A. 2015. The effect of topical ophthalmic 1% atropine on heart rate and rhythm in normal dogs. Vet. Ophthalmol. 18(2), 105–108. Greven, C.M., Engelbrecht, N.E., Slusher, M.M. and Nagy, S.S. 2000. Intraocular foreign bodies: management, prognostic factors, and visual outcomes. Ophthalmology 107(3), 608–612. Håkanson, N. and Forrester, S.D. 1990. Uveitis in the dog and cat. Vet. Clin. North. Am. Small. Anim. Pract. 20(3), 715–735. Hartley, C., McConnell, J.F. and Doust, R. 2007. Wooden orbital foreign body in a Weimaraner. Vet. Ophthalmol. 10(6), 390–393. Kovalcuka, L., Birgele, E., Bandere, D. and Williams, D.L. 2015. Comparison of the effects of topical and systemic atropine sulfate on intraocular pressure and pupil diameter in the normal canine eye. Vet. Ophthalmol. 18(1), 43–49. Lee, L.R. and Briner, A.M. 1996. Intralenticular metallic foreign body. Aust. N. Z. J. Ophthalmol. 24(4), 361–363. Lit, E.S. and Young, L.H. 2002. Anterior and posterior segment intraocular foreign bodies. Int. Ophthalmol. Clin. 42(3), 107–120. Ludders, J.W. and Heavner, J.E. 1979. Effect of atropine on tear formation in anesthetized dogs. J. Am. Vet. Med. Assoc. 175(6), 585–586. Luo, Z. and Gardiner, M. 2010. The incidence of intraocular foreign bodies and other intraocular findings in patients with corneal metal foreign bodies. Ophthalmology 117(11), 2218–2221. Marchegiani, A., Fruganti, A., Cerquetella, M., Cassarani, M.P., Laus, F. and Spaterna, A. 2017. Penetrating palpebral grass awn in a dog: unusual case of a penetrating grass awn in an eyelid. J. Ultrasound. 20, 81–84. Margadant, D.L., Kirkby, K., Andrew, S.E. and Gelatt, K.N. 2003. Effect of topical tropicamide on tear production as measured by Schirmer’s tear test in normal dogs and cats. Vet. Ophthalmol. 6(4), 315–320. Mester, V. and Kuhn, F. 2002. Intraocular foreign bodies. Ophthalmol. Clin. North. Am. 15(2), 235–242. Paulsen, M.E. and Kass, P.H. 2012. Traumatic corneal laceration with associated lens capsule disruption: a retrospective study of 77 clinical cases from 1999 to 2009. Vet. Ophthalmol. 15(6), 355–368. Peate, W.F. 2007. Work-related eye injuries and illnesses. Am. Fam. Physician. 75(7), 1017–1022. Saeed, A., Cassidy, L., Malone, D.E. and Beatty, S. 2008. Plain X-ray and computed tomography of the orbit in cases and suspected cases of intraocular foreign body. Eye (Lond) 22(11), 1373–1377. Schmidt, G., Dice, P. and Koch, S. 1975. Intraocular lead foreign bodies in four canine eyes. J. Small. Anim. Pract. 16(1–12), 33–39. Tetas Pont, R., Matas Riera, M., Newton, R. and Donaldson, D. 2016. Corneal and anterior segment foreign body trauma in dogs: a review of 218 cases. Vet. Ophthalmol. 19(5), 386–397. Tite, D.J., Batstone, M.D., Lynham, A.J., Monsour, F.N. and Chapman, P.J. 2002. Penetrating orbital injury with wooden foreign body initially diagnosed as an orbital floor blowout fracture. A. N. Z. J. Surg. 72(7), 529–530. van der Woerdt, A. 2001. Management of intraocular inflammatory disease. Clin. Tech. Small. Anim. Pract. 16(1), 58–61. Wilcock, B. and Peiffer Jr, R. 1987. The pathology of lens-induced uveitis in dogs. Vet. Pathol. 24(6), 549–553. | ||
| How to Cite this Article |
| Pubmed Style Kashani-Carver A, Turner G, Cáliz GE, Salih A, Jordan C, Cebrian P, Lowe R. Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report. Open Vet J. 2023; 13(10): 1379-1384. doi:10.5455/OVJ.2023.v13.i10.18 Web Style Kashani-Carver A, Turner G, Cáliz GE, Salih A, Jordan C, Cebrian P, Lowe R. Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report. https://www.openveterinaryjournal.com/?mno=163725 [Access: October 06, 2024]. doi:10.5455/OVJ.2023.v13.i10.18 AMA (American Medical Association) Style Kashani-Carver A, Turner G, Cáliz GE, Salih A, Jordan C, Cebrian P, Lowe R. Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report. Open Vet J. 2023; 13(10): 1379-1384. doi:10.5455/OVJ.2023.v13.i10.18 Vancouver/ICMJE Style Kashani-Carver A, Turner G, Cáliz GE, Salih A, Jordan C, Cebrian P, Lowe R. Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report. Open Vet J. (2023), [cited October 06, 2024]; 13(10): 1379-1384. doi:10.5455/OVJ.2023.v13.i10.18 Harvard Style Kashani-Carver, A., Turner, . G., Cáliz, . G. E., Salih, . A., Jordan, . C., Cebrian, . P. & Lowe, . R. (2023) Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report. Open Vet J, 13 (10), 1379-1384. doi:10.5455/OVJ.2023.v13.i10.18 Turabian Style Kashani-Carver, Andrea, Gemma Turner, Gisela Escalada Cáliz, Amna Salih, Casey Jordan, Prado Cebrian, and Robert Lowe. 2023. Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report. Open Veterinary Journal, 13 (10), 1379-1384. doi:10.5455/OVJ.2023.v13.i10.18 Chicago Style Kashani-Carver, Andrea, Gemma Turner, Gisela Escalada Cáliz, Amna Salih, Casey Jordan, Prado Cebrian, and Robert Lowe. "Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report." Open Veterinary Journal 13 (2023), 1379-1384. doi:10.5455/OVJ.2023.v13.i10.18 MLA (The Modern Language Association) Style Kashani-Carver, Andrea, Gemma Turner, Gisela Escalada Cáliz, Amna Salih, Casey Jordan, Prado Cebrian, and Robert Lowe. "Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report." Open Veterinary Journal 13.10 (2023), 1379-1384. Print. doi:10.5455/OVJ.2023.v13.i10.18 APA (American Psychological Association) Style Kashani-Carver, A., Turner, . G., Cáliz, . G. E., Salih, . A., Jordan, . C., Cebrian, . P. & Lowe, . R. (2023) Diagnosis, management, and outcome of an intralenticular foreign body in a dog: A case report. Open Veterinary Journal, 13 (10), 1379-1384. doi:10.5455/OVJ.2023.v13.i10.18 |