| Case Report | ||
Open Vet J. 2023; 13(12): 1776-1782 Open Veterinary Journal, (2023), Vol. 13(12): 1776–1782 Case Report Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case reportKang Yong1†, Zhengzhong Luo2†, Qingwen Yang1, Yunning Li3, Qian Lv1, Xixi Dai1, Liangpeng Zhong4, Yixin Huang2 and Suizhong Cao2*1 College of Animal Science and Technology, Chongqing Three Gorges Vocational College, Chongqing, China 2The Key Laboratory of Animal Disease and Human Health of Sichuan Province, College of Veterinary Medicine, Sichuan Agricultural University, Chengdu, China 3Balin Zuoqi Benda Animal Husbandry Service Co., Ltd., Chifeng, China 4Guangxi Aigele Agriculture and Animal Husbandry Technology Co., Ltd., Guigang, China †These authors have contributed equally to this work *Corresponding Author: Suizhong Cao. The Key Laboratory of Animal Disease and Human Health of Sichuan Province, College of Veterinary Medicine, Sichuan Agricultural University, Chengdu, China. Email: suizhongcao [at] 126.com Submitted: 25/10/2023 Accepted: 30/11/2023 Published: 31/12/2023 © 2023 Open Veterinary Journal
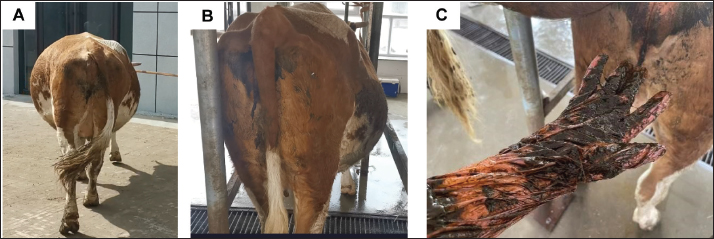
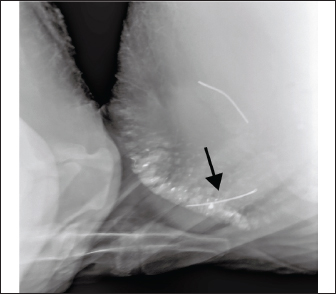
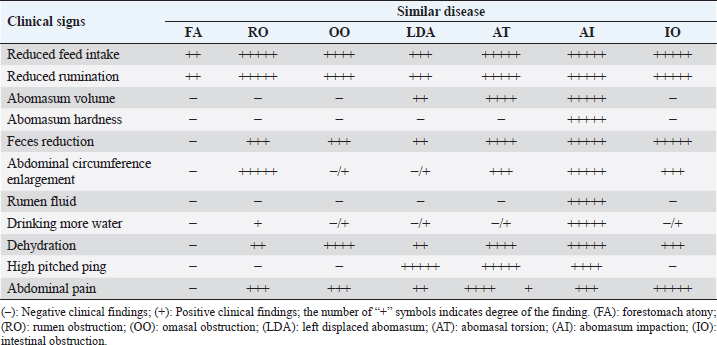
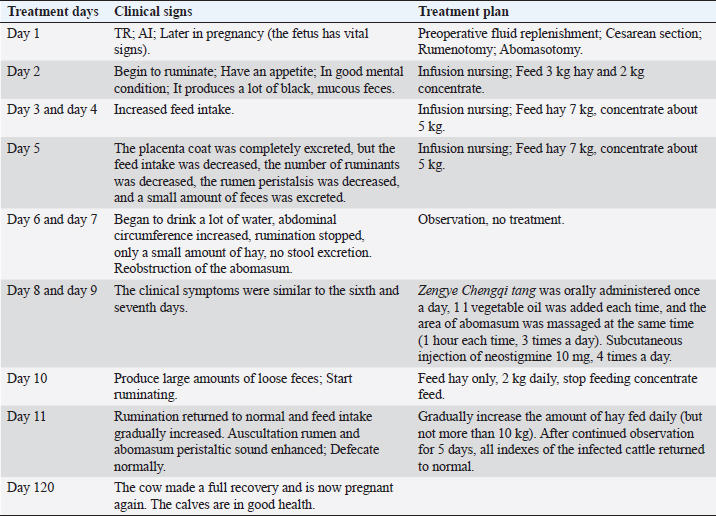
AbstractBackground: Traumatic reticulitis (TR) and abomasal obstruction are common digestive diseases in beef cattle. In clinical practice, these two conditions are often detected alone and rarely occur at the same time. Surgical therapy is an effective approach to treat both of these diseases. However, there are no reports on the treatment of abomasal obstruction in cattle induced by TR. Case Description: We here report a rare case of the diagnosis and treatment of TR associated with abomasal obstruction in a beef cow during late pregnancy. The affected cattle had an iron wire that was piercing the wall of the reticulum, but did not penetrate the wall; the abomasum was blocked and appeared solid; and the fetus survived well in utero (268 days gestation). To save the lives of the cow and fetus on the same day, a cesarean section was first performed, followed by rumenotomy, the foreign body (wire) was removed, and abomasotomy was finally performed. The fetus removed by cesarean section grew well, and the beef cow recovered and successfully became pregnant again. Conclusion: This case thus offers guidance for the timely diagnosis, effective treatment, and postoperative management of these digestive diseases in cattle to prevent progression and further complications. Keywords: Beef cattle, Abomasal obstruction, Traumatic reticulitis, Cesarean section, Late pregnancy. IntroductionTraumatic reticulitis (TR) in cattle is caused by ingested nails, pieces of wire, and nonmetallic materials that injure the reticular wall (Braun et al., 2018). Foreign bodies may penetrate the diaphragm into the chest (causing pleurisy and lung abscess in some cases) and the pericardium (causing pericarditis and subsequent myocarditis). Occasionally, the foreign body may impinge on the liver or spleen, causing an infection that could progress to sepsis (Kahn and Line, 2010). At present, TR is mainly treated conservatively by administering magnets or using antibiotics, anti-inflammatory drugs, intravenous fluids, and re moval of the reticular foreign body via rumenotomy (Braun et al., 2020). Both of these methods can increase the cure rate of the disease from approximately 60% when left untreated to 80%–90% (Kahn and Line, 2010). Studies have shown that surgical treatment is more effective than conservative treatment (Braun et al., 2020). TR can lead to dysregulation of the vagus nerve and to the development of anterior gastric diseases such as atony of the forestomach, ruminal tympany, vagal indigestion, and impaction of the omasum (Kahn and Line, 2010; Braun et al., 2018). How ever, there are no reports of an abomasal obstruction induced by TR. Abo masum impaction (AI) is a disorder in which the organ becomes enlarged due to the accumulation of solid, dry matter (El-Ashker et al., 2018; Yong et al., 2021). In general, AI is considered to be a rare condition; however, the incidence varies geographically and is related to feeding patterns, pregnancy, and complications with other diseases (Kahn and Line, 2010; Yasaswini et al., 2022). Yasaswini et al. (2022) confirmed that buffalo in third-trimester pregnancy with concurrent disorders and those fed paddy straw alone were more likely to be diagnosed with AI. In addition, AI can cause dehydration, disturbance of electrolyte balance, alkalosis, and progressive weight loss. According to the nature of the obstruction, AI is divided into food obstruction and foreign body obstruction (El-Ashker et al., 2018; Yong et al., 2021). Food obstruction is mainly caused by eating too much digestible protein and low-energy feed such as distiller grains (Kahn and Line, 2010; Yong et al., 2021). The foreign bodies causing AI mainly include phytobezoars, gravel, wool balls, placenta, plastic, string, almond husk, and pineapple pulp. According to our previous retrospective study (Yong et al., 2021), a nonsurgical approach is the preferred treatment for AI, with a cure rate of 61%, especially for mild to moderate cases. However, when nonoperative treatment is not effective, surgical treatment is a suitable option. Clinically, the cure rate is low for the middle and late stages of AI. The cure rate may be lower if accompanied by other diseases, especially late in pregnancy. Unfortunately, no cases have been reported in this regard. We here report the diagnosis and treatment of TR accompanied by AI in a beef cow during late pregnancy. This case can provide a useful reference for effective prevention and treatment of the disease. Case DetailsBasic informationOn July 24, 2022, a 4-year-old pregnant Simmental beef cow (approximately 600 kg, 268 days gestation) stopped eating and had not drunk water for 8 days. The cow was not producing any feces despite being given 1 kg of sodium sulfate and 8 l of vegetable oil twice. DiagnosisPrimary symptoms The affected cow had an increased abdominal circumference (Fig. 1A), was dehydrated (as evident by the recession of the eyes in the orbits and skin tent duration >2 seconds), and transabdominal palpation revealed a large accumulation of fluid in the rumen. The cow had a body temperature of 39.4°C, respiration rate of 42 breaths/minute, and heart rate of 74 beats/minute. The left 1–3 ribs had high-pitched “pinging” based on auscult ation and percussion. The right abomasum area was enlarged (Fig. 1B), which was hard and clearly defined on palpation. On rectal examination, the intestine was found to be empty, the intestinal wall was dry, and a small amount of black sticky feces was attached to the rectum (Fig. 1C). The fetus was confirmed to be alive by the rectal touch of the uterus. Laboratory examination Blood routine examination showed an elevated white blood cell count of 18.4 × 109/l (reference range: 4.9–12.0 × 109/l) and neutrophil count of 9.6 × 109/l (reference range: 1.8–6.3 × 109/l). There were also marked increases in the number of red blood cells (10.8 × 1012/l; reference range: 5.1–7.6 × 1012/l), hemoglobin content (154 g/l; reference range: 85–122 g/l), and hematocrit (0.75 l/l; reference range: 0.22–0.33 l/l). Biochemical results showed reduced potassium ions (3.2 mmol/l; reference range: 3.9–5.8 mmol/l), chloride ions (88 mmol/l; reference range: 95–110 mmol/l), and calcium ions (2.0 mmol/l; reference range: 2.43–3.10 mmol/l), with elevated creatinine (384.46 μmol/l; reference range: 88–175 μmol/l), urea nitrogen (28.2 mmol/l; reference range: 2.0–9.6 mmol/l), total bilirubin (19.23 μmol/l; reference range: 0.17–8.55 μmol/l), and γ-glutamyltransferase (29.7 U/l; reference range: 6.1–17.4 U/l). X-ray examination revealed a metallic foreign body in the reticulum (Fig. 2). The rumen fluid pH was approximately 8.5. Based on the above results, the cow was diagnosed with TR and AI. Based on previous reports (Braun et al., 2020), the diagnosis of TR can be confirmed by foreign body tests and X-ray examination. However, the differential diagnoses include forestomach atony (FA), rumen obstruction (RO), omasal obstruction (OO), left displaced abomasum (LDA), abomasal torsion (AT), and intestinal obstruction (IO) (Table 1). TreatmentTreatment plan Both TR and AI were treated surgically. To save the fetus, a cesarean section was performed on the cow before the two operations were carried out. Medication was administered 3 hours before surgery to correct the dehydration, electrolyte disturbances (hypokalemia, hypocalcemia, and hypochloremia), and acid-base disturbances (metabolic alkalosis). Table 2 describes the specific treatment plan in the present case.
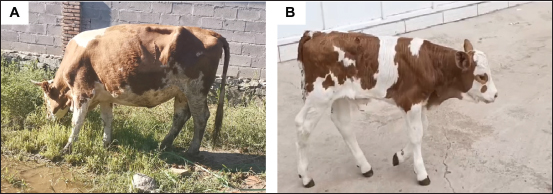
Fig. 1. Main clinical symptoms of AI. (A) Enlargement of the abdominal circumference; (B) enlargement of the abomasal area; (C) small amount of black sticky feces in the rectum.
Fig. 2. X-ray showing a metal foreign body inserted into the fundus of the reticulum. Preoperative treatmentAntibiotics and anti-inflammatory agents were administered in the following preoperative injections: (i) 500 ml Ringer’s solution, 5 mg vitamin C, and 50 ml of 10% potassium chloride; (ii) 100 ml of 10% glucose and 500 ml of 10% calcium gluconate; and (iii) 500 ml of 5% glucose and 5 g ampicillin, each as a one-time intravenous injection; and (iv) 0.3 g meloxicam as a one-time intramuscular injection. Surgical steps in cesarean and treatment of TRBefore surgery, the accumulated fluid in the rumen was extracted by inserting a gastric tube via the oral cavity, further relieving the abdominal pressure. After local-infiltration anesthesia with a 0.5% procaine solution, an incision was made in the middle of the paralumbar fossa in the lef t flank to open the abdominal cavity. Intraperitoneal exploration rev ealed that the wall of the reticulum had adhered to the diaphragm, although no inflammatory purulent exudate from the abdomen. The omasum was found to be approximately 0.5 times larger than normal and located in a more ventral position than normal. The volume of the abomasum was approximately 5–7 times normal and was very firm on palpation. The bowel was empty and the fetu s was active. The cesarean section was then performed. Part of the uterus was pulled out at the incision, the uterus was cut open, and the fetus was removed. The uterus was then sutured. Subsequently, the rumen was cut open and the wire attached to the wall of the reticulum was removed. The rumen was then sutured. Surgical steps in abomasal evacuationThe abomasum was cut open to eva cuate its contents. Xylazine hydrochloride (60 mg) w as injected intramuscularly to sedate the cow while lying down on the left side. After administering local-infilt ration anesthesia using a 0.5% procaine solution around the right lower abdominal wall in the abomasum region, the surgical incision was sele cted at the location where the AI was the hardest and made contact with the body surface. The feed material was removed a nd the abomasum was sutured. It is worth noting that we apply a slightly different approach for suturing the rumen, abomasum, and uterus from the traditional method. In particular, continuous spiral sutures were made on the mucosa of the uterus, and on the mucosa and submucosa of the rumen and abomasum with thinner polyglycolic acid (PGA) sutures (USP: 2–0), followed by continuous spiral sutures throughout the layer with thicker PGA sutures (USP: 0). Finally, cushing sutures were made with the same thicker PGA suture. Table 1. Differential diagnosis of abomasal obstruction and other similar diseases.
Table 2. Treatment logs.
Postoperative treatmentPostoperative treatment was provided for 5 days, including (i) 2 l Ringer’s solution, 5 g vitamin C, and 50 ml 10% potassium chloride; (ii) 1 l 10% glucose and 300 ml 10% calcium gluconate; (iii) 500 ml 10% concentrated sodium chloride; (iv) 500 ml 5% glucose and 5 g ampicillin; (v) 500 ml normal saline and 600 mg ranitidine, each as a single intravenous injection once per day; (vi) 20 mg neostigmine methylsulfate as a single subcutaneous injection twice a day; (vii) 20 ml compound vitamin B as a single intramuscular injection twice a day; and (viii) 100 IU of oxytocin as a single intramuscular injection once a day. Recovery and follow-upOn the seco nd day after the surgery, the cow began to ruminate, had an appetite, was in good spirits, and passed a large amount of black mucous feces. The cow fed on 3 kg hay and 2 kg concentrate. On the third and fourth days after surgery, feed intake increased, with 7 kg hay and approximately 5 kg concentrate consumed. On the fifth day, the fetal coat was completely excreted, but the feed intake decreased, the number of ruminations was reduced, the rumen peristalsis was weakened, and only a small amount of feces was excreted. On the sixth day after surgery, the cow began to drink a substantial amount of water, the abdominal circumference increased, rumination stopped, only a small amount of hay was eaten, and no excrement was observed. With rumen effusion, the high-pitched “pinging” could be heard by auscultation of the left side of ribs 1–3 with percussion, and palpation of the genuine stomach area was slightly hard. Therefore, we suspected that the abomasum had become obstructed again. Routine blood examination showed an elevated white blood cell count of 14.5 × 109 and neutrophil count of 7.2 × 109/l, whereas no obvious abnormalities were found in biochemical parameters. On the eighth and ninth days after the operation, Zeng Ye Cheng Qi Tang (a traditional Chinese medicine powder consisting of 300 g rhubarb, 600 g mirabilite, 60 g Magnolia officinalis, 80 g Fructus aurantii immaturus, 120 g Scrophularia ningpoensis, 120 g Ophiopogon japonicus, 120 g Rehmannia glutinosa, 150 g areca nut, 60 g Aucklandia, and 200 g Raphanus seed) was administered, which is often used to treat ruminal impaction and IO, along with 1 l of vegetable oil. The abomasum area was massaged at the same time as the administration of the formulation (1 hour each time, three times/day). Furthermore, a subcutaneous injection of 10 mg neostigmine was administered four times/day. The cow was fed hay only (2 kg a day) and concentrate feed was stopped. As of the 11th day, the ruminant returned to normal, feed intake gradually increased, the rumen and abomasum peristaltic sound was enhanced as detected by auscultation, and normal defecation was observed. The amount of hay fed daily was gradually increased (but not more than 10 kg). After continued observation for 5 days, all indices of the diseased cow returned to normal (Fig. 3A). After 120 days, the cow made a full recovery and became pregnant again. The calf born by cesarean section is in good health (Fig. 3B). Ethical approvalThe animal study was reviewed and approved by the College of Animal Science and Technology, Chongqing Three Gorges Vocational College. Written informed consent was obtained from the owners for the participation of their animals in this study. DiscussionEtiology of TR and AIThe cause of TR is well-elucidated and is mainly related to ingestion of sharp foreign bodies that can pierce the reticulum wall (Kahn and Line, 2010; Braun et al., 2018, 2020). Increased abdominal pressure during late pregnancy may also be a predisposing factor for foreign body penetration of the reticulum (Kahn and Line, 2010). Previous reports have suggested that AI may be related to eating foreign objects or indigestible feed (El-Ashker et al., 2018; Yong et al., 2021). In the present case, after surgical incision, we found that the accumulation in the abomasum comprised exclusively ground hay and no foreign body was evident. We believe that the reason for the obst ruction of the abomasum was likely the iron nails on the wall of the reticulum, leading to the disorder of the vagus nerve, consequently causing a reduction of the contractile force of the abomasum. In addition, the fetal compression on the abomasum, especially the pylorus, in late pregnancy led to the accumulation of grass material in the abomasum and the ultimate obstruction. Diagnosis of TR and AIClinical signs of acute TR may include anorexia, fever, drop in milk production, rumen atony and tympany, abdominal pain, an arched back, a tucked up and “guarded” abdomen, and spontaneous grunting, but symptoms may be obscure or absent in chronic cases (Braun et al., 2018). In this case, the examination of blood routine and biochemistry are used as assistant diagnoses for AI and TR. Increases in the levels of blood neutrophil count and hematocrit indicated bovine suffer from systemic inflammation and dehydration. Increases in the levels of total bilirubin and gamma-glutamyltransferase (GGT) indicated that there was also partial da mage to the liver and the possibility of obstructive jaundice. In addition, the diagnosis can be confirmed by X-ray or B-ultrasound. Braun et al. (2019) suggested that the clinical symptoms of abomasum disease can vary greatly among individuals. Diagnosis of any abomasum disease based on clinical symptoms alone is difficult and requires further auxiliary diagnosis such as measurement of blood biochemical parameters, rumen fluid parameters, and ultrasonography (Braun et al., 2019). A high rumen chlorine concentration, hypochloremia, and hypokalemia are considered to be the best indicators of abomasum disease (Yasaswini et al., 2021). Recent studies have reported that effective clinical indicators for the diagnosis of abomasal obstruction in buffalo are hypochloremia, hypokalemia, neutrophilia, eosinophilia, and lymphocytopenia, as well as elevated rumen fluid precipitation time, rumen chlorine content, and serum phosphocreatine kinase (Yasaswini et al., 2022). In practice, we have found that early diagnosis of AI is difficult, and can be easily confused with FA, RO, OO, LDA, AT, IO, and other diseases. For intermediate- and late-stage cases, abomasal obstruction can be diagnosed only by the following diagnostic points: dehydration, rumen effusion, failure to treat with large amounts of laxatives, and high-pitched “pinging” through auscultation combined with percussion in the left penultimate 1–3 intercostal space. In the present case, the cow had an empty rectum and reduced or no bowel movement. The abomasum area was hard upon palpation. The clinical symptoms combined with the results of biochemical tests (hypochloremia, hypocalcemia, hypokalemia, and metabolic alkalosis) were consistent with our previous report (Yong et al., 2021) and other reports (El-Ashker et al., 2018; Yasaswini et al., 2022) on AI.
Fig. 3. (A) Recovery of the sick cow 20 days after surgery. (B) Calf in good physical condition 32 days after birth. Choice of treatmentFor TR, initial treatment should include oral magnets and injections of antibiotics. When feed intake and rumination do not rapidly return to normal within 3–4 days of conservative treatment, it is best to reassess the cattle using X-rays and reformulate the treatment plan. Surgery is required only if the foreign body penetrates the reticulum or fails to fully adhere to the magnet. Braun et al. (2020) treated 503 cattle with TR, providing conservative treatment to 232 cows with an 82% success rate and surgery to 206 cows with a 90% success rate. Thus, surgical treatment was significantly more successful than conservative treatment. In the present case, an X-ray examination showed that the metal foreign body had penetrated the reticulum; thus, surgical treatment was decisively adopted. According to our previous report (Yong et al., 2021), in the early stage of AI, good therapeutic effects can be achieved by using rehydration, massaging the abomasum, and providing laxatives by gavage, with a cure rate of 61%. However, treatment at the middle and late stages of the disease should involve fluid replenishment at the same time as timely surgical treatment. There are two primary surgical methods that can be adopted. One is to open the rumen, intubate the reticulostoma, dredge the omasum first, and then dredge the abomasum to remove the obstruction. This method is suitable for cattle of a small size and without serious obstruction. The contents should be removed by abomasotomy for cattle of a large size or with a solid obstruction (Wang et al., 2005; Wittek et al., 2005; Cao et al., 2006; Wang, 2013). Due to the large size of the affected cow and the rigidity of the abomasum area, abomasotomy was performed in this case. Because the fetus exhibited vital signs, the decision to perform a cesarean section was clear. Among the many surgical methods for a cesarean section, a left abdominal wall incision while the cow is in a standing position is the most commonly used (Schultz et al., 2008). This procedure not only saves time but also prevents the bowel from spilling out of the wound. There are three surgical paths for paralumbar fossa in the left flank: anterior incision, middle incision, and posterior incision. In general, an anterior or middle incision is used to remove foreign bod ies in the reticulum, whereas a posterior incision is often used in the case of a cesarean section (Schultz et al., 2008). Due to the large size of the cow, a middle incision was selected in this case owi ng to the convenience of removing the foreign body from the reticulum. During the operation, the removal of foreign bodies in the reticulum and the removal of the fetus by cesarean section were relatively smooth. Our suture method of the uterus, rumen, and a bomasum helps to create a more orderly and tighter wound, which not only accelerates wound recovery but also prevents inflammation and perforation. The cow in this case began to ruminate on the second day after surgery and had an increased appetite. Based on the evaluation of fecal and uterine characteristics, the bovine has no significant abomasitis (abomasal ulcer) or metritis that occurred within one week after surgery. The cow showed complete recovery approximately 20 days after the operation and was able to conceive again approximately 120 days after surgery, which may be related to this optimal suture method. Postoperative carePostoperative care is critical to the success of surgery. Abomasitis or abomasal ulcers are important c omplications after abomasotomy and main contributors to the treatment failure of diseased cattle. Cattle are prone to abomasitis or abomasal ulcer after surgery, which may be related to the following factors: first, the surgical suture of the abomasal is not sufficiently tight; second, preoperative and postoperative persistent loss of appetite will cause long-term low pH in the abomasum, which has inspired the common expression “no acid, no ulcer” (Kahn and Line, 2010). We added ranitidine (1.5 mg/kg) into the infusion, which effectively controlled the occurrence of abomasitis. After surgery, it can take quite a long time f or the relaxation of the abomasum to recover. Although we used drugs to promote vagus nerve excitation after surgery, such as B complex vitamins and neostigmine, providing too much feed, especially concentrate, led to a second blockage of the abomasum. Fortunately, we administered Zeng Ye Cheng Qi Tang and vegetabl e oil in time, and the abomasum was effectively dredged again. Therefore, after an operation for AI, in addition to antibacterial and anti-inflammatory treatment to prevent abomasitis, it is also recommended to use drugs to promote abomasal drainage, such as continuous administration of 3–4 l vegetable oil for 1–5 days (Wittek et al., 2005), 180–200 g Si XiaoWan (a Chinese medicine preparation to promote gastrointestinal contraction, comprising rhubarb, Fructus gleditsiae, Semen pharbitidis, Cyperus rotundus, areca nut, and Trogopterus dung as the main ingredients), 200 mg metoclopramide, or 500–1,000 ml liquid paraffin (Wang et al., 2013). In addition, feed should be added gradually according to the recovery of the abomasum, controlling the rate and amounts provided. Finally, the type of feed provided postoperatively should be carefully considered. ConclusionThree operations (cesarean section, rumenotomy, and abomasotomy) were performed on one cow with TR and AI in succession on the same day and were all ultimately successful. The experience gained from this case can be summarized as follows. First, accurate diagnosis is the premise of successful treatment of disease. Second, the decisive and timely choice of surgical treatment is crucial. Finally, in postoperative care, it is important to choose the right type of feed and control the feeding amount according to the state of the disease. AcknowledgmentsThe authors would like to thank Cactus Communications Business Information Consulting Co., Ltd (Shanghai, China) for providing English editing services. Conflict of interestThe authors declare no conflicts of interest. Fundi ngThis project was supported by the Natural Science Foundation of Chongqing, China (grant number CSTB2022NSCQ-MSX1602), the Science and Technology Research Program of Chongqing Municipal Education Commission, China (grant number: KJQN202203507), and the Quality and Safety of characteristic Agricultural Products in Three Gorges Reservoir Area (grant number: CXQTP19037). Author contributionsKY and ZL contributed to writing the manuscript and the literature review. KY and ZL contributed to the critical revision of the manuscript as well as interpreting and describing the imaging findings. KY and YL performed the described surgery on the patient. QL, XD, and QY assessed the gross specimens and examined the biochemistry. QY, YL, QL, XD, LZ, YH, and SC contributed to the critical revision of the manuscript, assisted with surgery on the patient, and managed the clinical case. All authors contributed to the final manuscript review. Data availabilityThe original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding author. ReferencesBraun, U., Gerspach, C., Hilbe, M., Devaux, D. and Reif, C. 2019. Clinical and laboratory findings in 60 cows with type-3 abomasal ulcer. Schweiz. Arch. Tierheilkd. 161(9), 523–531. Braun, U., Gerspach, C., Ohlerth, S., Warislohner, S. and Nuss, K. 2020. Aetiology, diagnosis, treatment and outcome of traumatic reticulitis in cattle. Vet. J. 255, 105424–105434. Braun, U., Warislohner, S., Gerspach, C., Ohlerth, S. and Nuss, K. 2018. Treatment of 503 cattle with traumatic reticulitis. Acta. Vet. Scand. 60(1), 55–62. Cao, J., Qi, C.M. and Wang, C.A. 2006. Diagnosis and surgical treatment of cow’s abomasal impactions. Anim. Hus. Vet. 1, 40–41. El-Ashker, M.R., Salama, M.F., El-Boshy, M.E. and Abo El-Fadle, E.A. 2018. Significance of clinical observations and biochemical alterations in buffalo calves with dietary abomasal impaction. BMC. Vet. Res. 14, 1–7. Kahn, C.M. and Line, S. 2010. The merck veterinary manual, 10th ed. Merck & Co., Inc. Whitehouse Station, N.J., USA. pp: 144–145. Schultz, L.G., Tyler, J.W., Moll, H.D. and Constantinescu, G.M. 2008. Surgical approaches for cesarean section in cattle. Can. Vet. J. 49(6), 565–568. Wang, C.A. 2013. Prevention and treatment of dairy cattle diseases. China Agriculture Press. Beijing., China. pp: 551–558. Wang, L., Wang, F., Gao, H. and Wang, C.A. 2005. Diagnosis and surgical treatment of cow’s abomasal impactions. Chin. J. Vet. Med. 10, 26–27. Wittek, T., Constable, P.D. and Morin, D.E. 2005. Abomasal impaction in Holstein-Friesian cows: 80 cases (1980-2003). J. Am. Vet. Med. Assoc. 227, 287–291. Yasaswini, D., Kumari, K.N., Shobhamani, B., Prameela, D.R., Reddy, B.S. and Reddy, P.R.K. 2021. Clinical, haemato-biochemical, and ultrasonographic findings of abomasal impaction and abomasal ulcers in buffaloes. Trop. Anim. Health. Prod. 53(6), 543–554. Yasaswini, D., Kumari, K.N., Shobhamani, B., Prameela, D.R., Reddy, B.S., Reddy, K.P. and Reddy, P.R.K. 2022. Abomasal impaction in buffaloes: risk factors, clinical indicators, necropsy findings, and histology studies. Vet. Res. Commun. 47(1), 179–189. Yong, K., Luo, Z., Yang, Q., Zhang, C., Zhou, Q., Jiang, H., Zhang, Y. and Cao, S. 2021. Case report: abomasum impaction in beef cattle due to high intake of distillers’ grain and treatment options in Southwest China. Front. Vet. Sci. 8, 615871–615876. | ||
| How to Cite this Article |
| Pubmed Style Yong K, Luo Z, Yang Q, Li Y, Lv Q, Dai X, Zhong L, Huang Y, Cao S. Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report. Open Vet J. 2023; 13(12): 1776-1782. doi:10.5455/OVJ.2023.v13.i12.27 Web Style Yong K, Luo Z, Yang Q, Li Y, Lv Q, Dai X, Zhong L, Huang Y, Cao S. Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report. https://www.openveterinaryjournal.com/?mno=174286 [Access: May 13, 2024]. doi:10.5455/OVJ.2023.v13.i12.27 AMA (American Medical Association) Style Yong K, Luo Z, Yang Q, Li Y, Lv Q, Dai X, Zhong L, Huang Y, Cao S. Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report. Open Vet J. 2023; 13(12): 1776-1782. doi:10.5455/OVJ.2023.v13.i12.27 Vancouver/ICMJE Style Yong K, Luo Z, Yang Q, Li Y, Lv Q, Dai X, Zhong L, Huang Y, Cao S. Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report. Open Vet J. (2023), [cited May 13, 2024]; 13(12): 1776-1782. doi:10.5455/OVJ.2023.v13.i12.27 Harvard Style Yong, K., Luo, . Z., Yang, . Q., Li, . Y., Lv, . Q., Dai, . X., Zhong, . L., Huang, . Y. & Cao, . S. (2023) Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report. Open Vet J, 13 (12), 1776-1782. doi:10.5455/OVJ.2023.v13.i12.27 Turabian Style Yong, Kang, Zhengzhong Luo, Qingwen Yang, Yunning Li, Qian Lv, Xixi Dai, Liangpeng Zhong, Yixin Huang, and Suizhong Cao. 2023. Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report. Open Veterinary Journal, 13 (12), 1776-1782. doi:10.5455/OVJ.2023.v13.i12.27 Chicago Style Yong, Kang, Zhengzhong Luo, Qingwen Yang, Yunning Li, Qian Lv, Xixi Dai, Liangpeng Zhong, Yixin Huang, and Suizhong Cao. "Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report." Open Veterinary Journal 13 (2023), 1776-1782. doi:10.5455/OVJ.2023.v13.i12.27 MLA (The Modern Language Association) Style Yong, Kang, Zhengzhong Luo, Qingwen Yang, Yunning Li, Qian Lv, Xixi Dai, Liangpeng Zhong, Yixin Huang, and Suizhong Cao. "Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report." Open Veterinary Journal 13.12 (2023), 1776-1782. Print. doi:10.5455/OVJ.2023.v13.i12.27 APA (American Psychological Association) Style Yong, K., Luo, . Z., Yang, . Q., Li, . Y., Lv, . Q., Dai, . X., Zhong, . L., Huang, . Y. & Cao, . S. (2023) Diagnosis and treatment of traumatic reticulitis associated with abomasal obstruction in beef cattle during late pregnancy: A case report. Open Veterinary Journal, 13 (12), 1776-1782. doi:10.5455/OVJ.2023.v13.i12.27 |