| Case Report | ||
Open Vet J. 2022; 12(3): 308-311 Open Veterinary Journal, (2022), Vol. 12(3): 308–311 Case Report Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: A series of two casesYuki Shinomiya1, Shingo Takagaki2, Yoshiki Kawakami3 and Tomoki Motegi4*1Kameido Animal General Hospital, Tokyo, Japan 2Pigion Animal Hospital, Saitama, Japan 3Saito Animal Hospital, Gunma, Japan 4Veterinary Medical Center, Graduate School of Agricultural and Life Sciences, The University of Tokyo, Tokyo, Japan *Corresponding Author: Tomoki Motegi. Veterinary Medical Center, Graduate School of Agricultural and Life Sciences, The University of Tokyo, Tokyo, Japan. Email: a-t.motegi [at] g.ecc.u-tokyo.ac.jp Submitted: 31/01/2022 Accepted: 19/04/2022 Published: 10/05/2022 © 2022 Open Veterinary Journal
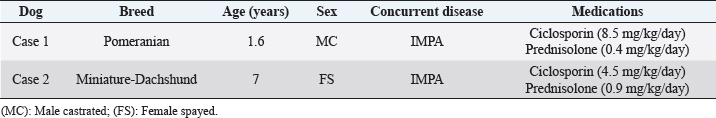
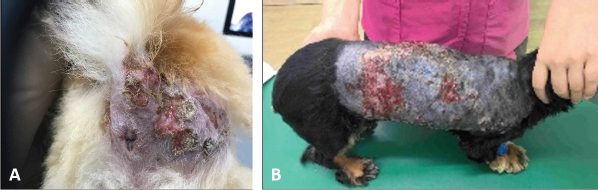
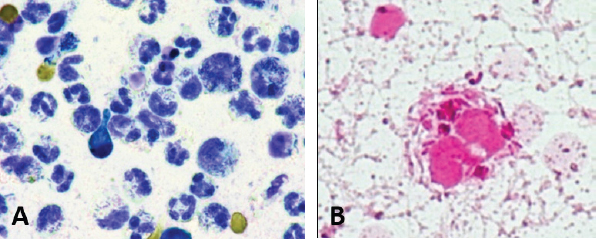
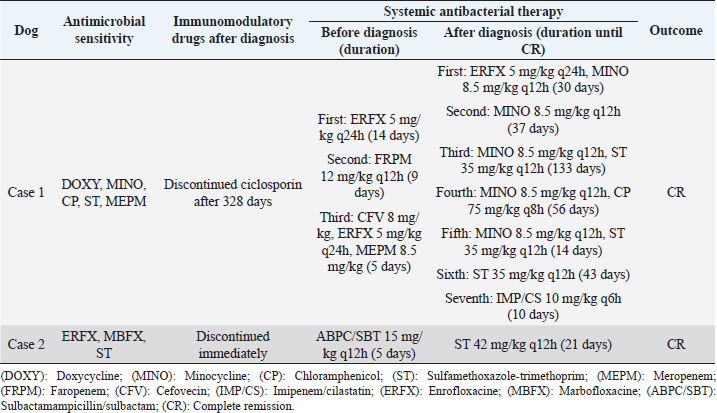
AbstractBackground: The Burkholderia cepacia complex (Bcc) is an opportunistic pathogen in humans and animals. Deep pyoderma caused by these bacteria in dogs has been previously reported. This case series aims to describe contrasting treatment responses in Bcc-related deep pyoderma in two dogs, a male and a female. Case Description: Both patients had a history of immune-mediated polyarthritis (IMPA) managed with oral ciclosporin and prednisolone. Their skin lesions were multifocal, irregular, erythematous to hemorrhagic, alopecic papules, plaques, and nodules, with extensive crusting, draining tracts, and ulceration. Cytological findings revealed a marked inflammatory response consisting of non-degenerative and degenerative neutrophils and macrophages, with moderate to abundant intracellular and extracellular Bcc. Ciclosporin and prednisolone were stopped in case 2 after diagnosis. However, it was challenging to stop the regimen in case 1 because of the recurrence of IMPA and the onset of iatrogenic hypoadrenocorticism. Case 1 did not achieve remission for approximately 66 weeks even with seven protocols because of multiple relapses, whereas it took only 3 weeks to achieve remission in case 2 while using one drug. Conclusion: For deep pyoderma with extensive lesions in immunosuppressed patients, one should consider infection with Bcc. Therefore, immunosuppressants should promptly be reduced in such patients, and then, intensive antimicrobial therapy may achieve remission. Keywords: Burkholderia cepacia complex, Deep pyoderma, Immunosuppressant, Dogs. IntroductionThe Burkholderia cepacia complex (Bcc) represents a group of motile, aerobic, glucose-nonfermenting gram-negative rods. These bacteria are ubiquitous in the natural environment and can be isolated from water, soil, fruits, and vegetables (Compant et al., 2008). Bcc organisms have emerged as important opportunistic pathogens in hospitalized (i.e., nosocomial infection) and immunocompromised patients and have been associated with contaminated disinfectants, hospital tap water, intravenous solutions, and medical devices (Nasser et al., 2004). In previous reports, Bcc-related deep pyoderma in dogs was successfully treated in a relatively short period with antimicrobials (Banovic et al., 2015; Cain et al., 2018). The objective of this case series is to describe different treatment responses in Bcc-related deep pyoderma in two dogs. Case DetailsThe signs and historical data of the two dogs are summarized in Table 1. Patient 1 was a castrated male, and patient 2 was a spayed female. Both patients had a history of immune-mediated polyarthritis (IMPA) managed with oral ciclosporin and prednisolone. Both dogs developed skin lesions within 4–5 months of starting ciclosporin. Skin lesions were initially dorsally distributed in both dogs, particularly in the buttocks area in case 1. These lesions were multifocal, irregular, erythematous to hemorrhagic, alopecic papules, plaques, and nodules, with extensive crusting, draining tracts, and ulceration (Fig. 1). Skin cytology in both dogs revealed a marked inflammatory response consisting of non-degenerative and degenerative neutrophils and macrophages, with moderate to abundant numbers of intracellular (neutrophils and macrophages) and extracellular rods (Fig. 2). These rod-shaped bacteria were identified as Bcc in a diagnostic laboratory. We axenically collected culture samples from non-ruptured comedones by fine-needle aspiration. After isolation and culturing with the rod-shaped bacteria, these samples were examined by a Matrix-assisted laser desorption/ionization-time of flight mass spectrometry imaging technique (MALDI Biotyper System, Bruker Corporation, Billerica, MA) in a commercial diagnostic laboratory (Sanritsu Zelkova, Chiba, Japan). As these mass spectrometry data matched B. cepacia, we diagnosed Bcc-related deep pyoderma. Table 1. Signalment and historical features of two dogs with Bcc-related deep pyoderma.
Fig. 1. Dorsal distribution of the skin lesions in both cases. (A): Lesions around the buttocks in case 1. (B): Lesions on the dorsum in case 2. The lesions appear multifocal, irregular, erythematous to haemorrhagic, alopecic papules, plaques, and nodules, with extensive crusting, draining tracts, and ulceration.
Fig. 2. Skin cytology in case 1. (A) Wright-Giemsa stain and (B) Gram stain revealing a marked inflammatory response consisting of non-degenerative and degenerative neutrophils and macrophages, with moderate to abundant numbers of intracellular (neutrophils and macrophages) and extracellular rods. Treatment approach and outcomeWe assessed the antimicrobial susceptibility after diagnosis by the broth microdilution method (He et al., 2016) (MicroScan WalkAway Plus System, Beckman Coulter, Inc., Brea, CA.) according to the Clinical & Laboratory Standards Institute guidelines (M100-S26). The treatment approach and outcomes for the two dogs are summarized in Table 2. In case 1, the first to third treatment protocols were performed in a primary hospital. Unfortunately, the primary doctor judged the microbiological report as contamination because of unawareness about Bcc and provided the treatment for Pseudomonas aeruginosa-related deep pyoderma. Case 1 did not achieve remission for approximately 66 weeks even with seven protocols, whereas it took only 3 weeks to achieve remission in case 2. Ciclosporin and prednisolone were stopped immediately in case 2 after diagnosis with Bcc infection; however, it was challenging to stop the regimen in case 1 because of IMPA recurrence and onset of iatrogenic hypoadrenocorticism. Case 1 was treated with topical therapy and general antibiotic administration. Antibiotics were selected based on susceptibility testing, and the treatment regimen included enrofloxacin, minocycline, sulfamethoxazole-trimethoprim, and chloramphenicol, but all these medications led to multiple relapses during treatment. Finally, ciclosporin was withdrawn, and imipenem-cilastatin was administered in the hospital for 10 days, after which remission was achieved. Table 2. Treatment approach and outcome in two dogs with Bcc-related deep pyoderma.
In contrast, case 2 attained remission using only sulfamethoxazole-trimethoprim administration and topical therapy by hair clipping and irrigation of lesions at the first visit. Ethical approvalNo ethical approval was required for these cases. DiscussionOur two cases confirm previous findings that immunosuppression, particularly related to ciclosporin treatment, is involved in the onset of Bcc-related deep pyoderma (Banovic et al., 2015; Cain et al., 2018). Case 2 achieved remission less than a month after infection onset, whereas in case 1, new lesions continued to appear despite treatment with various antibiotics, and it took over a year to achieve remission. In previous reports, the median treatment period to achieve remission was 56 days, with a maximum of 154 days, indicating that the treatment period for case 1 was very long (Banovic et al., 2015; Cain et al., 2018). The primary possible reason for this prolonged treatment duration was that the patient’s immunosuppressants could not be reduced promptly. In case 1, remission was achieved after ciclosporin withdrawal, and in previous reports, many cases achieved remission immediately following immunosuppressive treatment withdrawal (Banovic et al., 2015; Cain et al., 2018). Thus, it has been suggested that the treatment period might be prolonged if immunosuppressive treatment is difficult to discontinue. However, in a previous report, one case of continued immunosuppression achieved remission in the short term (Banovic et al., 2015); therefore, further examination is required regarding the relationship between the presence or absence of immunosuppressive treatment and the duration of the treatment. The second possibility for the prolonged treatment duration in case 1 is that antibiotics may not have been effective in vivo. In case 1, various antibiotics were used, but new lesions continued to appear for a long time. This may be because Bcc has developed several resistance mechanisms to antibacterial drugs, including β-lactamase production, drug excretion pumps, decreased drug permeability of the outer membrane, and structural changes in antimicrobial target sites (Rhodes and Schweizer, 2016). Furthermore, it has been reported that Bcc can survive in phagocytic cells, such as macrophages (Valvano, 2015). In case 1, lesion cytology confirmed the presence of many bacilli in macrophages and neutrophils. These antibiotics might have had an insufficient effect on Bcc in phagocytic cells. Our findings suggest that careful consideration of dosage and treatment evaluation for antibiotic administration for the treatment of Bcc is required. In previous reports, dermatological diseases, such as allergic dermatitis and sebaceous adenitis, were mainly reported as underlying conditions (Banovic et al., 2015; Cain et al., 2018). No case was diagnosed with Bcc infection concurrent with IMPA, and, likely, treatment for other autoimmune diseases might also be a risk factor for Bcc infection. Moreover, previous case reports only included males; however, patient 2 in this report was female; to our knowledge, this case series describes the first case of a female patient with Bcc undergoing treatment for deep pyoderma. In a recent report, one female dog had an emphysematous hepatic abscess associated with pyometra caused by Bcc (Carrillo et al., 2021). Hence, Bcc infection is not a male-specific condition. Furthermore, as Bcc-related deep pyoderma is very rare, the mechanisms leading to the infection becoming intractable, such as in case 1, remain unclear. Therefore, it is necessary to analyze similar cases in the future and to examine possible sex-based differences in patients’ predisposition to Bcc-related treatment difficulties. In conclusion, Bcc-related deep pyoderma should be considered in immunosuppressed patients. If diagnosed, promptly reducing the immunosuppressants and intensive antimicrobial therapy may be helpful to achieve remission. Conflicts of interestThe authors declare that there is no conflict of interest. FundingThis work was funded by the JSPS KAKENHI Grant-in-Aid for Young Scientists (grant JP20K15675). ReferencesBanovic, F., Koch, S., Robson, D., Jacob, M. and Olivry, T. 2015. Deep pyoderma caused by Burkholderia cepacia complex associated with ciclosporin administration in dogs: a case series. Vet. Dermatol. 26(4), 287–e64. Cain, C.L., Cole, S.D., Bradley, C.W., Canfield, M.S. and Mauldin, E.A. 2018. Clinical and histopathological features of Burkholderia cepacia complex dermatitis in dogs: a series of four cases. Vet. Dermatol. 29(5), 457–e156. Carrillo, J., Escobar, M.T., Porlan, S., Rodenas, C. and Agut, A. 2021. Emphysematous hepatic abscess and pyometra, both caused by Burkholderia cepacia, in a bitch. Vet. Rec. Case Rep. 9, e53. Compant, S., Nowak, J., Coenye, T., Clément, C. and Ait Barka, E. 2008. Diversity and occurrence of Burkholderia spp. in the natural environment. FEMS Microbiol. Rev. 32, 607–626. He, Q., Chen, W., Huang, L., Lin, Q., Zhang, J., Liu, R. and Li, B. 2016. Performance evaluation of three automated identification systems in detecting carbapenem-resistant Enterobacteriaceae. Ann. Clin. Microbiol. Antimicrob. 15, 40. Nasser, R.M., Rahi, A.C., Haddad, M.F., Daoud, Z., Irani-Hakime, N. and Almawi, W.Y. 2004. Outbreak of Burkholderia cepacia bacteremia traced to contaminated hospital water used for dilution of an alcohol skin antiseptic. Infect. Control Hosp. Epidemiol. 25, 231–239. Rhodes, K.A. and Schweizer, H.P. 2016. Antibiotic resistance in Burkholderia species. Drug Resist. Updat. 28, 82–90. Valvano, M.A. 2015. Intracellular survival of Burkholderia cepacia complex in phagocytic cells. Can. J. Microbiol. 61, 607–615. | ||
| How to Cite this Article |
| Pubmed Style Shinomiya Y, Takagaki S, Kawakami Y, Motegi T, . Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases. Open Vet J. 2022; 12(3): 308-311. doi:10.5455/OVJ.2022.v12.i3.1 Web Style Shinomiya Y, Takagaki S, Kawakami Y, Motegi T, . Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases. https://www.openveterinaryjournal.com/?mno=22089 [Access: July 27, 2024]. doi:10.5455/OVJ.2022.v12.i3.1 AMA (American Medical Association) Style Shinomiya Y, Takagaki S, Kawakami Y, Motegi T, . Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases. Open Vet J. 2022; 12(3): 308-311. doi:10.5455/OVJ.2022.v12.i3.1 Vancouver/ICMJE Style Shinomiya Y, Takagaki S, Kawakami Y, Motegi T, . Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases. Open Vet J. (2022), [cited July 27, 2024]; 12(3): 308-311. doi:10.5455/OVJ.2022.v12.i3.1 Harvard Style Shinomiya, Y., Takagaki, S., Kawakami, Y., Motegi, T. & (2022) Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases. Open Vet J, 12 (3), 308-311. doi:10.5455/OVJ.2022.v12.i3.1 Turabian Style Shinomiya, Yuki, Shingo Takagaki, Yoshiki Kawakami, Tomoki Motegi, and . 2022. Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases. Open Veterinary Journal, 12 (3), 308-311. doi:10.5455/OVJ.2022.v12.i3.1 Chicago Style Shinomiya, Yuki, Shingo Takagaki, Yoshiki Kawakami, Tomoki Motegi, and . "Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases." Open Veterinary Journal 12 (2022), 308-311. doi:10.5455/OVJ.2022.v12.i3.1 MLA (The Modern Language Association) Style Shinomiya, Yuki, Shingo Takagaki, Yoshiki Kawakami, Tomoki Motegi, and . "Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases." Open Veterinary Journal 12.3 (2022), 308-311. Print. doi:10.5455/OVJ.2022.v12.i3.1 APA (American Psychological Association) Style Shinomiya, Y., Takagaki, S., Kawakami, Y., Motegi, T. & (2022) Contrasting treatment responses by Burkholderia cepacia complex-related deep pyoderma: a series of two cases. Open Veterinary Journal, 12 (3), 308-311. doi:10.5455/OVJ.2022.v12.i3.1 |