| Case Report | ||
Open Vet J. 2022; 12(3): 375-382 Open Veterinary Journal, (2022), Vol. 12(3): 375–382 Case Report Long-term outcome following synthetical reconstruction of the medial collateral tarsal ligament in a dogPhilippe Buttin1†, Vincenzo Santoro2†, Mathilde Agbalé3, Bastien Goin4,5,6*, Thibaut Cachon4, Eric Viguier4 and Filippo Maria Martini2,71Itinerant surgeon, Villaz, France 2Ortovet stp srl, Parma, Italy 3National Veterinary School of Alfort, Maisons-Alfort, France 4University of Lyon, VetAgro Sup, Interactions Cellules Environnement (ICE), Marcy l’Etoile, France 5Univ Lyon, Univ Gustave Eiffel, Univ Claude Bernard Lyon 1, LBMC UMR T_9406, F-69622 Lyon, France 6Novetech Surgery, Monaco 7University of Parma, Department of Veterinary Sciences, Parma, Italy †These two authors contributed equally to this work. *Corresponding Author: Bastien Goin. Unité pédagogique de Chirurgie Campus Vétérinaire de Lyon, VetAgro Sup BP 83 - 1 Avenue Bourgelat, 69280 Marcy l'Etoile, France. Email: bastien.goin [at] vetagro-sup.fr Submitted: 30/03/2022 Accepted: 16/05/2022 Published: 06/06/2022 © 2022 Open Veterinary Journal
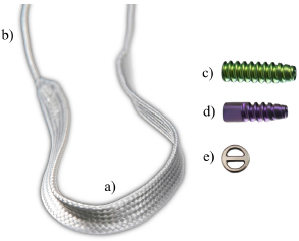
AbstractBackground: Tibiotarsal instabilities caused by partial or complete rupture of the medial collateral tarsal ligament (MCTL) are commonly treated by arthrodesis techniques with poor functional results and significant complication rates. Case Description: This study describes a new surgical technique for synthetic reconstruction of the MCTL in an overweight dog (estimated body condition score 8/9) with an avulsion of the long head of the MCTL. Three bone tunnels were drilled in the distal tibia, the talus, and the central tarsal bone, thus respecting the anatomical insertions of the physiological ligament. An Ultra-High Molecular Weight Polyethylene (UHMWPE) implant was fixed with interference screws to reconstruct the long and short heads of the MCTL. Premature weight-bearing was reported at 2 weeks postoperatively following early removal of the flexible restraint (bivalve resin boot), which had initially been prescribed for 6 weeks. At 11 weeks postoperatively, the tibiotarsal joint showed good valgus stability and the dog’s gait was subnormal. At 12 and 16 months postoperatively, the dog regained full function of the operated limb although no weight loss was initiated as recommended. Conclusion: The use of a UHMWPE implant fixed with interference screws to reconstruct the MCTL allowed a return to full function of the tibiotarsal joint, without complications despite an early return to weight-bearing without external restraint. The success of this isolated surgical technique could lead to improvements in the surgical management of MCTL rupture if these initial results are confirmed by a prospective study with a larger number of patients. Keywords: Tibiotarsal joint, Medial collateral tarsal ligament, Synthetic ligament reconstruction, UHMWPE implant, Dog. IntroductionThe tarsus is a complex joint that relies on numerous ligaments for stability (Johnston and Tobias, 2017). It is particularly vulnerable to external trauma such as road traffic accidents, resulting in fractures, (sub)dislocations, sprains, or tendinopathies associated with tissue decay that may be significant (Vaughan, 1987; Fossum, 2013; Linn and Duerr, 2020). In such context, the animal is usually presented with variable degrees of lameness, edema or hematoma, pain on palpation, and possibly abnormal angulation associated with crackling on mobilization (Fossum, 2013; Linn and Duerr, 2020). Collateral ligaments are often injured or even ruptured during malleolar fractures, abrasive accidents, strenuous exercise, or falls (Vaughan, 1987; Linn and Duerr, 2020). Dogs have a slight physiological valgus of the pelvic limbs, which is why the medial collateral tarsal ligament (MCTL) (which limits the valgus and the internal rotation of the tibiotarsal joint) is more frequently affected than its lateral counterpart (Linn and Duerr, 2020). Suspicion of MCTL injury may be confirmed by orthopedic examination combined with stress radiographs (Vaughan, 1987; Fossum, 2013; Bogisch and Schuenemann, 2019; Linn and Duerr, 2020). Following diagnosis, two surgical management options are most commonly performed: the placement of a joint osteosynthesis plate (Muir and Norris, 1999; Benson and Boudrieau, 2002; Mckee et al., 2004; Scrimgeour et al., 2012) or less frequently, the placement of a synthetic implant (Aron and Purinton, 1985; Diamond et al., 1999; Harasen, 2000; Martin et al., 2019; Luescher et al., 2020). These synthetic implants may be diverse, such as nylon monofilament, braided polyester wire or orthopedic wire that can be tied in a figure 8 around previously implanted screws in the tibia and the talus (Aron and Purinton, 1985; Diamond et al., 1999; Harasen, 2000). The stability of a joint treated with nylon monofilament or with braided ultra-high molecular weight polyethylene (UHMWPE) wire attached with anchors appears to be satisfactory in view of the biomechanical results obtained on anatomical parts (Martin et al., 2019). The use of polypropylene or polyethylene wire tied in a figure of 8 after passing through bone tunnels or polyethylene wire passed through a tibial tunnel and fixed distally via anchors at the level of the calcaneus and the talus also seem to provide promising ex vivo biomechanical results (Luescher et al., 2020). The insertion of a transarticular external fixator (TEF) or a calcaneo-tibial screw are frequently used stabilization methods following the placement of an osteosynthesis plate or a synthetic implant (Diamond et al., 1999; Harasen, 2000; Benson and Boudrieau, 2002; Mckee et al., 2004; Jaeger et al., 2005; Yardımcı et al., 2016; Frame et al., 2017). TEFs are also used alone in cats, particularly when tissue damage is not compatible with the implantation of surgical hardware in direct contact with the joint; the device then allows the affected limb to be immobilized while secondary tissue fibrosis takes place (Diamond et al., 1999; Kulendra et al., 2011). Currently, there is no consensus on a particular surgical technique for the management of partial or complete rupture of one or both heads of the MCTL. Although arthrodesis techniques are commonly used, they do not maintain joint mobility and a 75% complication rate is reported, half of which are major complications such as diffuse plantar necrosis (Roch et al., 2008; Scrimgeour et al., 2012; Beever et al., 2016). Similarly, although one of the goals of synthetic implants described in the literature is to maintain joint mobility, the latter have high complication rates, especially when braided wire or orthopedic wire is used (Aron and Purinton, 1985; Beever et al., 2016). These complications are most commonly associated with the use of transarticular immobilization methods such as TEFs: infection at pin site or pin rupture requiring revision surgery in 70% of cases (Beever et al., 2016). In addition, TEFs may cause joint ankylosis associated with amyotrophy of the affected limb, thus increasing the animal’s functional recovery period (Lieber and Danzig, 1988; Seibert et al., 2011). In recent years, there has been renewed interest in MCTL reconstruction techniques using synthetic implants in cats (Luescher et al., 2020) and dogs (Martin et al., 2019). To our knowledge, these techniques have not yet been applied to patients in vivo. The surgical technique of MCTL reconstruction described in this study is in line with this scientific trend. It is based on the use of a UHMWPE implant fixed with interference screws, which allows the synthetic reconstruction of the MCTL in place of the anatomical insertions of the physiological ligament. The goal of this new surgical technique is to preserve the mobility of the tibiotarsal joint without the need for rigid and invasive transarticular immobilization (such as TEFs) in the post-operative period. Case DetailsA 5-year-old castrated male Australian Shepherd weighing 40 kg with an estimated body condition score of 8/9 (Freeman et al., 2011) was presented with left hind limb lameness. Orthopedic examination revealed valgus instability of the tarsus in extension. Tissue swelling medial to the tarsus was visible on preoperative radiographs. The clinical and paraclinical picture was consistent with a first hypothesis of avulsion of the long head of the medial collateral ligament of the left tibiotarsal joint. The clinical context was therefore favorable to the use of a synthetic ligament reconstruction technique. Design implantsThe synthetic implant (Novalig 4000, Novetech Surgery, Monaco) is manufactured from a specific braiding of UHMWPE medical grade multi-filaments already used for orthopedic implants in several medical applications, such as anterior cruciate implants (Purchase et al., 2007). Once braided, the synthetic ligament is sterilized with ethylene oxide. It comprises two components: the implanted section (Fig. 1a) and a puller wire allowing the insertion of the implant into the bone tunnels (Fig. 1b). The fixation system is made of titanium interference screws (Fig. 1c and d) (Novetech Surgery, Monaco) for excellent biocompatibility. Its design offers minimal invasiveness as well as strong and immediate fixation (Blanc et al., 2019; Goin et al., 2019). Finally, the cortical button (Fig. 1e) (Novetech Surgery, Monaco) may be used to offer two distal bone reinsertion sites. Surgical techniqueThe animal was placed in left lateral decubitus position. The surgical site was prepared aseptically. A surgical drape glued to the entire left pelvic limb was used to isolate the skin from potential contact with the implants. A 10–15 cm medial approach to the tibiotarsal joint was performed. The drape, which was previously taped to the skin, was sutured around the surgical approach. Soft tissues were dissected to reveal the proximal insertion of the MCTL and its two distal insertions (short head and long head). Three holes were drilled successively through the distal tibia, the talus and the central tarsal bone. Distal tibial drilling was performed from the medial side in a latero-cranial direction, thus allowing the passage of the prosthesis without a lateral skin incision and avoiding drilling into the fibular malleolus. A 2-mm guide pin was implanted thanks to a viewfinder, the bore sighter of which was placed from the medial to the lateral side of the distal tibial epiphysis (Fig. 2). The tibial tunnel was then drilled with a 3.6-mm cannulated drill following the axis of the guide pin. The depth of the tunnel was then measured to determine the appropriate length for the interference screw. The tibial tunnel was then preformed with a 4.5 × 20-mm interference screw (Novetech Surgery, Monaco) from the medial to the lateral side. Once the 2-mm guide pin was implanted at the level of the talus, it was removed and replaced with a 1.2-mm one. The tunnel was drilled with a 3-mm cannulated drill following the axis of the guide pin and then preformed with a 4 × 13-mm screw (Novetech Surgery, Monaco). Finally, the central tarsal bone was drilled from its medio-plantar side in a dorso-lateral direction to avoid tarsal bones II and III, which are too small to be implanted. Tarsal bone IV must also be avoided because it is not in a favorable axis to hold a screw without causing a fracture. A screw that would pass through several tarsal bones with shared mobility may also create a fracture through impingement when the tarsus is mobilized again. The tunnel of the central tarsal bone was preformed following the same procedure as for the talus. The entrance to each tunnel was smoothed using a No. 11 scalpel blade to remove any blunt splinters caused by drilling, and then rinsed with sterile physiological fluid.
Fig. 1. Photo of implants for synthetic reconstruction of MCTL: synthetic UHMWPE implant composed of two parts: implantable section (a) and traction wire (b); associated with 4.5 × 20 mm (c) and 4 × 13 mm (d) interference screw fixation system, and cortical button (e).
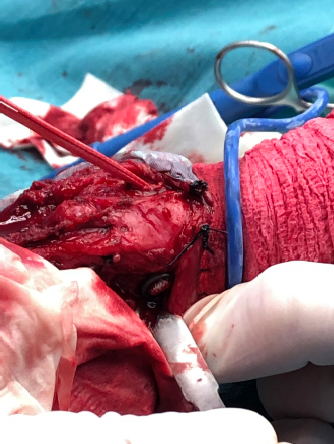
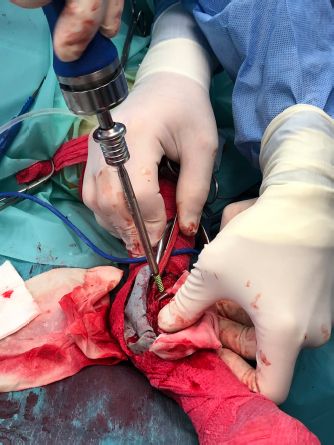
Fig. 2. Intraoperative photograph showing the placement of the viewfinder to implant the pin that will be used to guide the drilling of the distal tibia. After all the holes were drilled and preformed and the surgical site was thoroughly rinsed with physiological fluid, the UHMWPE implant (Novalig 4000®, Novetech Surgery, Monaco) was removed from its sterile bag and isolated in a sterile compress moistened with physiological fluid. The UHMWPE implant was slid into the cortical button (Novetech Surgery, Monaco) using the traction wires up to the middle of the synthetic implant. The transition area between the traction wire and the operating section was bent in half with Kocher forceps to facilitate its passage into the bone tunnel. To pass the UHMWPE implant through the tibial bone tunnel, a guide tube was passed through the tunnel from the medial to the lateral side. A gelpi retractor was used to keep the skin away from lateral bone surfaces (Fig. 2). The grommet was inserted inside the guide tube so that the bent portion emerged laterally from the tibial tunnel. A first traction wire of the UHMWPE implant was then placed inside the grommet. The wire was then passed from the lateral to the medial side of the tibial tunnel by pulling on the guide tube and the grommet. The same operation was repeated with the second traction wire. Given the orientation of the tunnel, the button was applied to a good quality, non-weakened bone surface (Fig. 3). The UHMWPE implant was repositioned in the cortical button so that one strand emerging from the medial side of the tibia would be twice as long as the other. The shorter strand was for reconstructing the short head of the MCTL and the second strand for the long head. At this point, the tibial insertion of the MCTL had to be locked with an interference screw. Each strand of the UHMWPE implant was wrapped around a Kocher clamp until sufficient tension was achieved. The depth of the tibial tunnel was measured and the appropriate 4.5x20-mm cannulated screw was selected. A 1-mm blunt guide pin was carefully inserted into the tibial tunnel. The previously selected screw was slid along the pin. A snap-in screwdriver was then placed along the axis of the pin and the interference screw was implanted flush with the bone surface, respecting the axis of the guide pin while maintaining significant tension on both strands of the UHMWPE implant (Fig. 4).
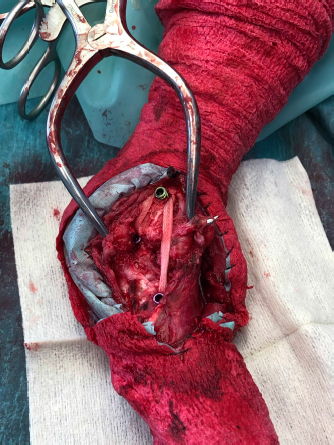
Fig. 3. Verification of correct positioning of cortical button on lateral side of distal tibia. To reconstruct the short head of the MCTL, the short strand of the UHMWPE implant was passed through the talar tunnel from the medial to the lateral side, using the guide tube and the grommet. Its distal insertion was then locked using the same procedure as for tibial locking, with the tibiotarsal joint at 90° and material adapted to the size of the tunnel: 1-mm blunt guide pin and 4x13-mm interference screw. Reconstruction of the long head of the MCTL and locking of its distal insertion at the level of the tarsal tunnel was performed according to the same procedure, with the long strand of the UHMWPE implant. This time, the tibiotarsal joint was placed in extension. Traction wires were cut flush with the bone on the lateral side of the limb, thus completing the synthetic MCTL reconstruction technique (Fig. 5). The surgical site was then closed plane by plane. Immediate postoperative radiographs showed a good implantation of the interference screws in the bone drillings through the distal tibia and the talus. However, the bone drilling corresponding to the distal insertion of the long head of the MCTL was not satisfactory: it was drilled between the tarsal midbone and tarsal bones II and III, while it should have been drilled through the tarsal midbone (Fig. 6).
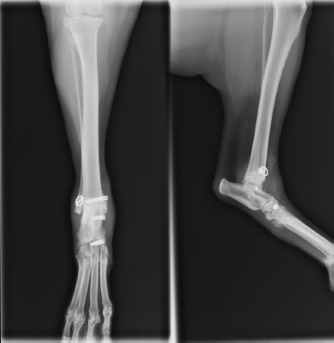
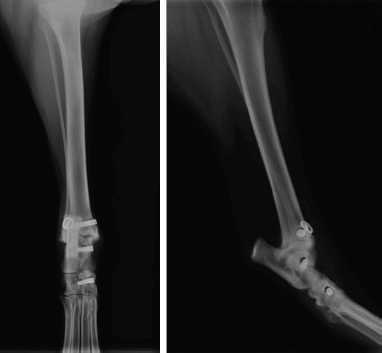
Fig. 4. Implantation of interference screw in distal tibial drilling. Providing external restraint with a bivalve resin boot was recommended. It was cut along the medial and lateral side of the operated pelvic limb and maintained by straps to allow supervision of the healing process during postoperative follow-up. This restraint had to be kept in place for a minimum of 6 weeks. Immobilization was recommended for 6 to 8 weeks if the animal was active or lived outside before the operation, as well as a strict two-month rest period. A radiographic check-up was prescribed at one and three months post-operatively. Owners were highly recommended to modify their animal’s diet to make him lose weight, in order to increase the surgery’s chances of success. ResultsAn approximation in the third drilling (distal reconstruction of the long head of the MCTL) was observed during the immediate postoperative radiographic control (Fig. 6). No other intraoperative complications occurred. Unfortunately, postoperative advice was not followed properly. The bivalve resin boot was completely removed at only 2 weeks postoperatively. However, a first radiographic check at 11 weeks showed good valgus stability of the tibiotarsal joint and the orthopedic examination showed a return to subnormal function of the pelvic limb during locomotion. At 12 months postoperatively, valgus stability of the tibiotarsal joint was maintained and the pelvic limb returned to normal function during locomotion. At 16 months post-op, radiographic control showed ovalization of the bone tunnels with no clinical impact on the stability of the tibiotarsal joint (Fig. 7). The dog’s body condition score did not change over the 16 months of postoperative follow-up and was still estimated at 8/9 at each of the four check-ups performed during this period (Freeman et al., 2011). However, the dog still regained full function of his operated limb by synthetic reconstruction of the MCTL.
Fig. 5. Intraoperative view at the end of the synthetic MCTL reconstruction technique. DiscussionAvulsion of the long head of the left MCTL was diagnosed in a five-year-old overweight castrated male Australian Shepherd. The context was favorable to the implementation of the surgical ligament reconstruction technique previously described. Although the immediate postoperative radiographic control showed an approximation of the third drilling (distal reconstruction of the long head of the MCTL), the surgeon chose not to reopen the surgical site (Fig. 6). The reason for this choice was that sufficient tightening torque was perceived by the veterinary surgeon during the implantation of the 4x13-mm interference screw, which was compatible with satisfactory primary fixation of the UHMWPE implant according to his empirical experience. Although external restraint was maintained for only 2 weeks and the animal did not lose weight as advised, no postoperative complications were identified and one year after surgery, the animal regained normal locomotion. This synthetic MCTL reconstruction technique thus allowed a complete and durable functional and clinical recovery without the need for invasive transarticular immobilization, such as the placement of a transarticular external fixator (TEF). However, the use of a bivalve resin boot was recommended for a minimum of 6 weeks, which was not respected. In addition, the animal did not lose weight as advised. Early weight-bearing on the limb without any other form of restraint and the excess weight were potentially the cause of the progressive ovalization of the tunnels observed on the radiographic images taken 16 months postoperatively. In humans, obesity has been shown to be a leading risk factor for intraoperative complications in total hip arthroplasty (Haynes et al., 2017). Similarly, weight loss in dogs would be an essential element in the treatment of osteoarthritis, which is a frequent complication in osteoarticular surgery (Marshall et al., 2009). The ovalization of the tunnels could lead to a loss of biomechanical strength of the fixation system owing to a reduced contact surface in the bone tunnels at the bone/UHMWPE implant/interference screw interface. This loss of strength could even lead to implant slippage at this interface, resulting in a complete loss of functionality of the fixation system. However, none of this was observed from a clinical point of view during the 16 months of postoperative follow-up. The tibiotarsal joint always remained stable in valgus position. A secondary biological stabilization (Kulendra et al., 2011) may have reinforced or even supplemented the primary mechanical stabilization achieved during surgery and thus ensured durable stability of the tibiotarsal joint.
Fig. 6. Radiographic views of dog’s left pelvic limb from side (left) and front (right) in immediate postoperative period.
Fig. 7. Profile (left) and front (right) radiographs of dog’s left pelvic limb at 16-month postoperative check-up. The objective of this new surgical management is to preserve the mobility of the tibiotarsal joint without having to resort to rigid and invasive transarticular immobilization devices such as TEFs during the postoperative period. As commonly used arthrodesis techniques cannot reach this goal, the placement of an implant was decided according to a different technique from those described in the literature (Aron and Purinton, 1985; Diamond et al., 1999; Harasen, 2000; Martin et al., 2019; Luescher et al., 2020). Initially, the choice of the location of implant insertions varied between authors. In this study, a distal tibial insertion, a talar insertion and an insertion at the level of the central tarsal bone were performed, thus respecting the anatomical insertions of the physiological ligament to maintain joint function. While some research teams chose to create one tibial and two talar insertions (Aron and Purinton, 1985; Harasen, 2000; Martin et al., 2019), others suggested recreating three insertions: a tibial one, one at the level of the calcaneus, and one at the level of the central tarsal bone or the talus (Luescher et al., 2020). However, none of the MCTL heads inserts at calcaneal level (Johnston and Tobias, 2017). Second, the material used is likely to have a strong impact on the outcome of the procedure as sutures, particularly braided and orthopedic sutures, are associated with a high risk of infection compromising the stability of the device and often necessitating its removal (Aron and Purinton, 1985; Beever et al., 2016). The implant selected in this study is therefore a UHMWPE implant that is similar to the one used by Marin et al. (2019). Its combined use with an interference screw fixation system was initially described as a surgical technique for synthetic cranial cruciate ligament reconstruction. Ex vivo biomechanical, pull-out and fatigue studies have reported very encouraging results regarding the strength of the implant itself, as well as the reliability of its interference screw fixation system (Blanc et al., 2019; Goin et al., 2019). Tunnel drilling, the use of a cortical button and interference screw locking provide greater stability than implanted screws connected with suture or orthopedic wire (Aron and Purinton, 1985; Diamond et al., 1999; Harasen, 2000; Martin et al., 2019). The knotting technique and the vertical drilling technique associated with distal locking by suture anchors seem interesting, but they have only been tested on anatomical cat parts (Luescher et al., 2020). Their efficacy on an ex vivo and in situ canine format is therefore not known. The orientation of the tunnels also contributes to the stability of the synthetic implant. The distal tibial tunnel was drilled from the medial side in a latero-cranial direction, which avoids drilling through the fibular malleolus and helps positioning the cortical button on a good quality and non-weakened bone surface. Martin et al. (2019) chose to extend the drillings into the calcaneus so that the cortical button is applied laterally against the calcaneus, which potentially creates a risk of fracture. The tunnels were drilled with a larger diameter relatively to the size of the animal and at a smaller distance from each other than in our study. Finally, implant tensioning was performed using Kocher forceps (Buttin et al., 2020). This method was preferred to the less accurate subjective tensioning described by some authors (Luescher et al., 2020). The arthrodesis techniques described in the literature have high complication rates, with about 30% of the plates having to be removed (Roch et al., 2008; Scrimgeour et al., 2012). Skin lesions (dermatitis, ulceration, plantar necrosis), assembly ruptures (of TEFs) and septic arthritis are common (Roch et al., 2008; Beever et al., 2016). The ligament reconstruction technique described here is minimally invasive and only requires one surgical procedure, thus decreasing the risk of complication. The use of a bivalve resin boot to provide external restraint reduces the risk of skin damage, while providing sufficient stabilization of the limb (Meeson et al., 2011; Henderson et al., 2015). Indeed, invasive techniques such as the use of TEFs or a calcaneo-tibial screw are associated with complication rates of 31% (Nielsen and Pluhar, 2006) and 8% (Corr et al., 2010) respectively. In addition, the surgical site is easily accessible, and healing can be monitored regularly. Our study has certain limitations. The intraoperative surgical technique would have been better if the lateral side of the distal tibia had been deperiostealized. The cortical button would thus have been in direct contact with bone and not in conflict with the soft tissues on which it could have been affixed. High-field magnetic resonance imaging or an ultrasound at the 16-month post-operative check-up would have given us a better understanding of the periarticular environment of the tibiotarsal joint. It would also have allowed us to identify whether fibrosis was involved in maintaining joint stability. Moreover, this is a unique result. The recruitment of a cohort of dogs benefiting from this technique would allow its application to be validated in a more extensive and objective manner. Nevertheless, the low prevalence of the condition and the difficulty in defining the inclusion criteria (exact nature of lesions, head(s) involved, traumatic or non-traumatic context, joint laxity of either metabolic or genetic origin, etc...) make this clinical study difficult to implement. Similarly, monitoring how the distribution of the reaction forces of each limb evolves could be an objective indicator of success (Bockstahler et al., 2007; Katic et al., 2009). Interestingly, this result was obtained in an uncommonly favorable context with no marked tissue decay present at the joint (Vaughan, 1987; Fossum, 2013; Linn and Duerr, 2020). However, the surgical site is considered contaminated in such a context, which considerably increases the risk of infectious complications. It would therefore seem advisable to postpone the possible placement of an implant and to proceed only with conventional wound management in the first place. Considering the potential sequelae of tissue and bone remodeling, the question arises as to the feasibility and efficacy of implementing the technique described in our study following a traumatic event causing tissue decay. Data availabilityAll the data are presented in tables or figures directly in this article. Conflict of interestThe authors have no conflicts of interest to declare. Funding statementThis study was supported by the company Novetech Surgery, which provided human resources in the person of Bastien Goin for data processing and writing of this scientific article during his thesis. AcknowledgmentsThe authors would like to thank Mrs. Cooke-Martageix for English copyediting of this article. ReferencesAron, D.N. and Purinton, P.T. 1985. Replacement of the collateral ligaments of the canine tarsocrural joint: a proposed technique. Vet. Surg. 14(3), 178–184. Beever, L.J., Kulendra, E.R. and Meeson, R.L. 2016. Short and long-term outcome following surgical stabilization of tarsocrural instability in dogs. Vet. Comp. Orthop. Traumatol. 29(2), 142–148. Benson, J.A. and Boudrieau, R.J. 2002. Severe carpal and tarsal shearing injuries treated with an immediate arthrodesis in seven dogs. J. Am. Anim. Hosp. Assoc. 38(4), 370–380. Blanc, Q., Goin, B., Rafael, P., Moissonnier, P., Carozzo, C., Buttin, P., Cachon, T. and Viguier, E. 2019. Effect of the number of interference screws for the fixation of an intra-articular cranial cruciate ligament prosthesis in dogs: Biomechanical study. Comput. Methods Biomech. Biomed. Engin. 22(Suppl. 1), S102–S104. Bockstahler, B.A., Skalicky, M., Peham, C., Müller, M. and Lorinson, D. 2007. Reliability of ground reaction forces measured on a treadmill system in healthy dogs. Vet. J. 173(2), 373–378. Bogisch, S. and Schuenemann, R. 2019. The function of the short medial collateral ligaments of the canine tarsus: a cadaveric study. J. Am. Anim. Hosp. Assoc. 55(5), 215–219. Buttin, P., Goin, B., Cachon, T. and Viguier, E. 2020. Repair of tendon disruption using a novel synthetic fiber implant in dogs and cats: the surgical procedure and three case reports. Vet. Med. Int. 2020, 1–9. Corr, S.A., Draffan, D., Kulendra, E., Carmichael, S. and Brodbelt, D. 2010. Retrospective study of Achilles mechanism disruption in 45 dogs. Vet. Rec. 167(11), 407–411. Diamond, D., Besso, J. and Boudrieau, R. 1999. Evaluation of joint stabilization for treatment of shearing injuries of the tarsus in 20 dogs. J. Am. Anim. Hosp. Assoc. 35(2), 147–153. Fossum, T.W. 2013. Small animal surgery, 4th ed. St. Louis, MO: Elsevier Mosby. Frame, K., Bridges, J. and Worth, A. 2017. Effect of a calcaneo-tibial screw on medial and lateral stability of the canine tarsocrural joint ex vivo. Vet. Comp. Orthop. Traumatol. 30(05), 331–338. Freeman, L., Becvarova, I., Cave, N., MacKay, C., Nguyen, P., Rama, B., Takashima, G., Tiffin, R., van Beukelen, P. and Yathiraj, S. 2011. WSAVA nutritional assessment guidelines. J. Feline Med. Surg. 13(7), 516–525. Goin, B., Rafael, P., Blanc, Q., Cachon, T., Buttin, P., Carozzo, C., Chabrand, P. and Viguier, E. 2019. Biomechanical analysis of a ligament fixation system for CCL reconstruction in a canine cadaver model. Comput. Methods Biomech. Biomed. Engin. 22(Suppl. 1), S109–S111. Harasen, G.L.G. 2000. Tarsal shearing injuries in the dog. Can. Vet. J. 41(12), 940–943. Haynes, J., Nam, D. and Barrack, R.L. 2017. Obesity in total hip arthroplasty. Bone Jt. J. 99-B(1_Supple_A), 31–36. Henderson, A.L., Latimer, C. and Millis, D.L. 2015. Rehabilitation and physical therapy for selected orthopedic conditions in veterinary patients. Vet. Clin. North Am. Small Anim. Pract. 45(1), 91–121. Jaeger, G.H., Wosar, M.A., Marcellin-Little, D.J. and Lascelles, B.D.X. 2005. Use of hinged transarticular external fixation for adjunctive joint stabilization in dogs and cats: 14 cases (1999–2003). J. Am. Vet. Med. Assoc. 227(4), 586–591. Johnston, S.A. and Tobias, K.M. 2017. Veterinary surgery: small animal expert. Elsevier-Health Sciences Division. Katic, N., Bockstahler, B.A., Mueller, M. and Peham, C. 2009. Fourier analysis of vertical ground reaction forces in dogs with unilateral hind limb lameness caused by degenerative disease of the hip joint and in dogs without lameness. Am. J. Vet. Res. 70(1), 118–126. Kulendra, E., Grierson, J., Okushima, S., Cariou, M. and House, A. 2011. Evaluation of the transarticular external skeletal fixator for the treatment of tarsocrural instability in 32 cats. Vet. Comp. Orthop. Traumatol. 24(5), 320–325. Lieber, R.L. and Danzig, L.A. 1988. Differential response of the dog quadriceps muscle to external skeletal fixation of the knee. Muscle. Nerve. 11(3), 193–201. Linn, K. and Duerr, F.M. 2020. Tarsal region. In Canine lameness. Hoboken, NJ: John Wiley & Sons, Ltd; pp: 279–306. Luescher, M., Schmierer, P.A., Park, B.H., Pozzi, A., Gutbrod, A., Evans, R. and Knell, S.C. 2020. Biomechanical comparison of knotted and knotless stabilization techniques of the tarsal medial collateral ligament in cats: a cadaveric study. Vet. Surg. 49(2), 390–400. Marshall, W.G., Bockstahler, B.A., Hulse, D.A. and Carmichael, S. 2009. A review of osteoarthritis and obesity: current understanding of the relationship and benefit of obesity treatment and prevention in the dog. Vet. Comp. Orthop. Traumatol. 22(5), 339–345. Martin, Y., Johnson, M.D., Travers, C.J., Colee, J., McConkey, M.J. and Banks, S.A. 2019. Biomechanical comparison of four prosthetic ligament repair techniques for tarsal medial collateral ligament injury in dogs. Am. J. Vet. Res. 80(5), 469–479. Mckee, W.M., May, C., Macias, C. and Lapish, J.R. 2004. Pantarsal arthrodesis with a customised medial or lateral bone plate in 13 dogs. Vet. Rec. 154(6), 165–170. Meeson, R.L., Davidson, C. and Arthurs, G.I. 2011. Soft-tissue injuries associated with cast application for distal limb orthopaedic conditions: a retrospective study of sixty dogs and cats. Vet. Comp. Orthop. Traumatol. 24(2), 126–131. Muir, P. and Norris, J. 1999. Tarsometatarsal subluxation in dogs: partial arthrodesis by plate fixation. J. Am. Anim. Hosp. Assoc. 35(2), 155–162. Nielsen, C. and Pluhar, G.E. 2006. Outcome following surgical repair of achilles tendon rupture and comparison between postoperative tibiotarsal immobilization methods in dogs: 28 cases (1997–2004). Vet. Comp. Orthop. Traumatol. 19(4), 246–249. Purchase, R., Mason, R., Hsu, V., Rogers, K., Gaughan, J.P. and Torg, J. 2007. Fourteen-year prospective results of a high-density polyethylene prosthetic anterior cruciate ligament reconstruction. J. Long Term Eff. Med. Implants. 17(1), 13–19. Roch, S.P., Clements, D.N., Mitchell, R.A.S., Downes, C., Gemmill, T.J., Macias, C. and McKee, W.M. 2008. Complications following tarsal arthrodesis using bone plate fixation in dogs. J. Small Anim. Pract. 49(3), 117–126. Scrimgeour, A., Bruce, W., Bridges, J., Walsh, V. and Worth, A. 2012. Long-term outcomes after partial tarsal arthrodesis in working farm dogs in New Zealand. N. Z. Vet. J. 60(1), 50–55. Seibert, R., Lewis, D., Coomer, A., Sereda, C., Royals, S. and Leasure, C. 2011. Stabilisation of metacarpal or metatarsal fractures in three dogs, using circular external skeletal. N. Z. Vet. J. 59(2), 96–103. Vaughan, L.C. 1987. Disorders of the tarsus in the dog. I. Br. Vet. J. 143(5), 388–401. Yardımcı, C., Özak, A., Önyay, T. and Serdar İnal, K. 2016. Management of traumatic tarsal luxations with transarticular external fixation in cats. Vet. Comp. Orthop. Traumatol. 29(3), 232–238. | ||
| How to Cite this Article |
| Pubmed Style Buttin P, Santoro V, Agbale M, Goin B, Cachon T, Viguier E, Martini FM, . Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog. Open Vet J. 2022; 12(3): 375-382. doi:10.5455/OVJ.2022.v12.i3.11 Web Style Buttin P, Santoro V, Agbale M, Goin B, Cachon T, Viguier E, Martini FM, . Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog. https://www.openveterinaryjournal.com/?mno=280 [Access: July 27, 2024]. doi:10.5455/OVJ.2022.v12.i3.11 AMA (American Medical Association) Style Buttin P, Santoro V, Agbale M, Goin B, Cachon T, Viguier E, Martini FM, . Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog. Open Vet J. 2022; 12(3): 375-382. doi:10.5455/OVJ.2022.v12.i3.11 Vancouver/ICMJE Style Buttin P, Santoro V, Agbale M, Goin B, Cachon T, Viguier E, Martini FM, . Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog. Open Vet J. (2022), [cited July 27, 2024]; 12(3): 375-382. doi:10.5455/OVJ.2022.v12.i3.11 Harvard Style Buttin, P., Santoro, V., Agbale, M., Goin, B., Cachon, T., Viguier, E., Martini, F. M. & (2022) Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog. Open Vet J, 12 (3), 375-382. doi:10.5455/OVJ.2022.v12.i3.11 Turabian Style Buttin, Philippe, Vincenzo Santoro, Mathilde Agbale, Bastien Goin, Thibaut Cachon, Eric Viguier, Filippo Maria Martini, and . 2022. Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog. Open Veterinary Journal, 12 (3), 375-382. doi:10.5455/OVJ.2022.v12.i3.11 Chicago Style Buttin, Philippe, Vincenzo Santoro, Mathilde Agbale, Bastien Goin, Thibaut Cachon, Eric Viguier, Filippo Maria Martini, and . "Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog." Open Veterinary Journal 12 (2022), 375-382. doi:10.5455/OVJ.2022.v12.i3.11 MLA (The Modern Language Association) Style Buttin, Philippe, Vincenzo Santoro, Mathilde Agbale, Bastien Goin, Thibaut Cachon, Eric Viguier, Filippo Maria Martini, and . "Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog." Open Veterinary Journal 12.3 (2022), 375-382. Print. doi:10.5455/OVJ.2022.v12.i3.11 APA (American Psychological Association) Style Buttin, P., Santoro, V., Agbale, M., Goin, B., Cachon, T., Viguier, E., Martini, F. M. & (2022) Long-term outcome following synthetical reconstruction of the tarsal medial collateral ligament in a dog. Open Veterinary Journal, 12 (3), 375-382. doi:10.5455/OVJ.2022.v12.i3.11 |