| Case Report | ||
Open Vet J. 2021; 11(2): 217-221 Open Veterinary Journal, (2021), Vol. 11(2): 217–221 Case Report Long-term management of a cat with nasopharyngeal lymphoma by chlorambucilKaho Takahashi1, Takashi Baba1, Marin Hirokawa1, Masaki Miyajima1, Miori Kishimoto1, Junpei Kimura2, Hirotaka Kondo3 and Keitaro Ohmori1*1Cooperative Department of Veterinary Medicine, Faculty of Agriculture, Tokyo University of Agriculture and Technology, Tokyo, Japan 2College of Veterinary Medicine and Research Institute for Veterinary Medicine, Seoul National University, Seoul, South Korea 3Laboratory of Veterinary Pathology, College of Bioresource Sciences, Nihon University, Kanagawa, Japan *Corresponding Author: Keitaro Ohmori. Cooperative Department of Veterinary Medicine, Faculty of Agriculture, Tokyo University of Agriculture and Technology, Tokyo, Japan. Email: k-ohmori [at] cc.tuat.ac.jp Submitted: 29/01/2021 Accepted: 22/03/2021 Published: 25/04/2021 © 2021 Open Veterinary Journal
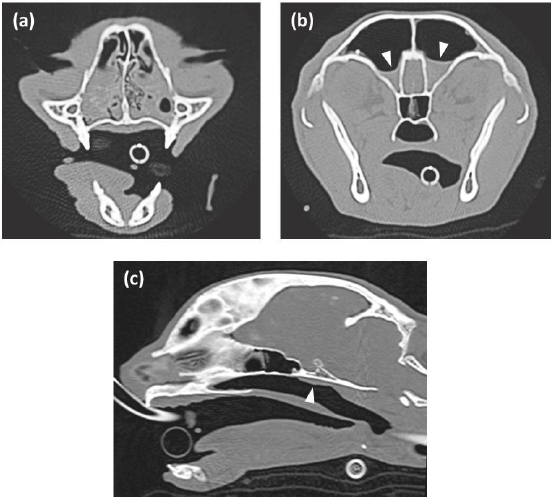
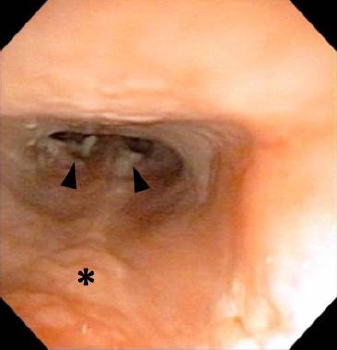
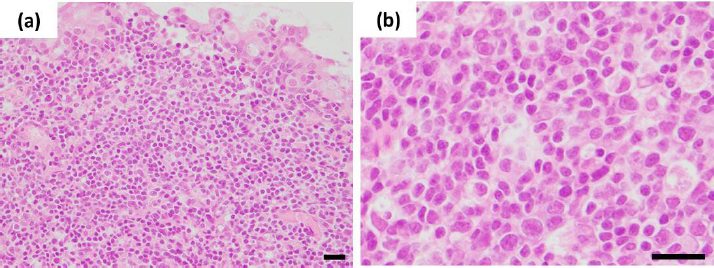
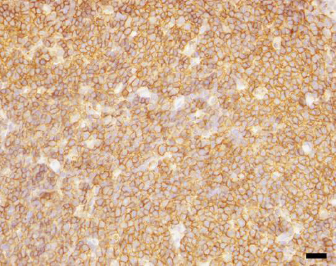
AbstractBackground: Lymphoma in the nasal cavity is the most common tumor of cats' upper respiratory tract. However, the effect of single-agent chlorambucil on nasal or nasopharyngeal lymphoma has not been evaluated in cats. Case Description: An 8-year-old, castrated male Scottish Fold weighing 3.5 kg presented with an 8-month history of nasal discharge, sneezing, and mild epistaxis. CT and rhinoscopy revealed nasal discharge and slight swelling of the nasopharyngeal mucosa, but no masses and local invasions were detected. Histopathological and immunohistochemical analyses of the nasopharyngeal mucosa demonstrated B-cell lymphoma in the cat. The treatment with chlorambucil led to long-term management of the cat without any side effects. No recurrences of clinical signs have been observed for 754 days. Conclusion: The present case report suggests that chlorambucil can be a therapeutic option for feline localized nasopharyngeal B-cell lymphoma without masses and local invasions. Keywords: Cat, Chlorambucil, Lymphoma, Nasal cavity, Nasopharynx. IntroductionLymphoma in the nasal cavity is the most common tumor of cats’ upper respiratory tract (Henderson et al., 2004; Ferguson et al., 2020). It can occur in the nasal site (67%–82%), nasopharynx (10%–16%), or both locations (8%–18%) (Little et al., 2007; Santagostino et al., 2015). Most immunophenotypes of feline lymphoma in the nasal cavity are of B-cell origin (Little et al., 2007; Santagostino et al., 2015). It shows aggressive behavior, but the prognosis varies from complete remission to short-term, depending on the treatment response (Moore, 2013). Therapeutic options include chemotherapy, radiation therapy, and combined chemoradiotherapy (Moore, 2013). In previous studies, various chemotherapeutic protocols consisting of multi-agent combinations were applied for cats with nasal and nasopharyngeal lymphomas (Sfiligoi et al., 2007; Haney et al., 2009; Taylor et al., 2009). The median survival time of cats with nasal and nasopharyngeal lymphomas treated with chemotherapy alone ranged from 116.5 to 140 days (Haney et al., 2009; Taylor et al., 2009). Chlorambucil and prednisolone are usually used for cats with gastrointestinal small-cell lymphoma, leading to clinical remission in these animals (Paulin et al., 2018). However, the effect of single-agent chlorambucil on nasal or nasopharyngeal lymphoma has not been evaluated in cats. Herein, we report nasopharyngeal B-cell lymphoma without obstructive masses, local invasions, or metastases in a successfully treated cat with chlorambucil. Case DetailsAn 8-year-old, castrated male Scottish Fold weighing 3.5 kg presented with an 8-month history of nasal discharge, sneezing (>10 times/day), and mild epistaxis (day 1). Two-and-a-half months before the current presentation, Pseudomonas aeruginosa was detected in the nasal discharge. The cat had been treated with nebulization and several oral antibiotics sensitive to P. aeruginosa by a referring veterinarian; however, clinical signs did not improve and gradually worsened in the treatment period. On day 1, the complete blood count, blood biochemical analysis, and radiographic examination for the skull revealed no specific abnormalities. A thoracic ultrasound identified hypertrophic cardiomyopathy (HCM), while an abdominal ultrasound did not find any masses and lesions suspicious of neoplasm. To further elucidate the cause of nasal signs, head, chest, and abdominal CT and rhinoscopy were carried out on day 1 under general anesthesia. Head CT in the transverse plane revealed that the nasal cavity was filled with soft tissue material suspicious of nasal discharge (Fig. 1a), and the frontal sinus was partly filled with the same material (Fig. 1b). There were no contrast effects in either area (Fig. 1a and b). Head CT in the mid-sagittal plane revealed slight nasopharyngeal swelling in the dorsal portion, but there were no abnormal contrast effects, osteolytic changes, or lymphadenopathies (Fig. 1c). Chest and abdominal CT did not show any lymphadenopathies and masses in the body. After the nasal cavity was cleansed with saline several times, it was examined by anterograde and retrograde rhinoscopy. Anterograde rhinoscopy found only a little nasal discharge, while retrograde rhinoscopy detected a little nasal discharge and slight swelling of the nasopharyngeal mucosa but without masses (Fig. 2). Several biopsy specimens were obtained from the nasopharyngeal mucosa’ swollen sites with endoscopic biopsy forceps for histopathological and immunohistochemical analyses. The histopathological and immunohistochemical specimens were reviewed by a single board-certified veterinary anatomic pathologist (H.K.). The collected nasal discharge was subjected to bacterial culture and antimicrobial susceptibility tests. To prevent rhinoscopy-associated infection and bleeding in the nasal cavity, the cat was subcutaneously injected with enrofloxacin (Baytril; Bayer, Tokyo, Japan, 5 mg/kg q24h), carbazochrome (Adona; Nipro ES Pharma, Osaka, Japan, 1 mg/kg q12h), and tranexamic acid (Vasolamine; Meiji Seika Pharma, Tokyo, Japan, 10 mg/kg q12h) on day 1. The cat was orally administered with the same drugs on days 2 and 3 with slight modifications as follows: carbazochrome (Adona; Nipro ES Pharma, 0.5 mg/kg q12h) and tranexamic acid (Transamin; Daiichi Sankyo, Tokyo, Japan, 10 mg/kg q12h). Also, because the cat had HCM, oral administration of carvedilol (Artist; Daiichi Sankyo, 0.05 mg/kg q24h) was initiated on day 2. The histopathological analysis demonstrated that the nasopharyngeal tissue’s submucosa had expanded by a neoplasm composed of solid sheets of round cells (Fig. 3a). The neoplastic cells had distinct cell borders with small amounts of eosinophilic cytoplasm. Nuclei were round to oval, measured two erythrocytes in diameter, and had one to three nucleoli (Fig. 3b). Anisocytosis and anisokaryosis were moderate, and there were five mitoses per 10 ×400 fields. Immunohistochemically, most neoplastic cells were positive for CD20 (rabbit anti-CD20 polyclonal antibody; Thermo Fisher Scientific, Waltham, MA) (Fig. 4), but only a few cells were positive for CD3 (mouse anti-CD3 monoclonal antibody, clone F7.2.38; Agilent Technologies Japan, Tokyo, Japan) (data not shown). Based on the histopathological and immunohistochemical analyses, the cat was diagnosed with nasopharyngeal large B-cell lymphoma.
Fig. 1. Head CT images in the transverse and mid-sagittal planes were reconstructed by bone function. (a) The nasal cavity was filled with soft tissue material suspicious of nasal discharge, and there were no contrast effects. (b) The frontal sinus was partly filled with the same material (arrowheads), and there were no contrast effects. (c) Slight nasopharyngeal swelling was detected in the dorsal portion (arrowhead). There were no abnormal contrast effects or osteolytic changes.
Fig. 2. Retrograde rhinoscopy for the nasopharynx. Nasal discharge (arrowheads) and slight swelling of the nasopharyngeal mucosa (asterisk) were detected.
Fig. 3. Histopathological findings of the nasopharyngeal mucosa. (a) The submucosa of the nasopharyngeal tissue had expanded by a neoplasm composed of solid sheets of round cells. (b) Nuclei were round to oval, measured two erythrocytes in diameter, and had one to three nucleoli. Hematoxylin and eosin stain (Bar=20 μm).
Fig. 4. Immunohistochemical analysis for CD20 of the nasopharyngeal mucosa. Most neoplastic cells were positive for anti-CD20 antibody (Bar=20 μm). No masses, local invasions in the nasal cavity, or metastases were found in the cat; therefore, the nasopharyngeal B-cell lymphoma in the cat was considered stage I lymphoma manifesting as a single tumor or localized in a single anatomic area (Moore, 2013). Because there were no masses in the cat, multidrug chemotherapy, but not radiation therapy, was proposed to the owner; however, the owner did not provide consent for it. Alternatively, although chlorambucil and prednisolone were considered, chlorambucil (Leukeran; Aspen Pharma, Baar, Switzerland, 2 mg/m2 q24h) without prednisolone was initiated on day 25 based on the owner’s request. Bacterial culture and antimicrobial susceptibility tests identified enrofloxacin-sensitive P. aeruginosa in the nasal discharge. The cat had already been administered with enrofloxacin on days 1–3; therefore, further antibiotics were not used. On day 36, the frequency of sneezing had decreased to two to three times/day, and nasal discharge and epistaxis were rare. The dosage of chlorambucil was, therefore, reduced to 2 mg/m2 q48h. Subsequently, the nasal signs were further improved with the treatment. To monitor the progression of nasopharyngeal lymphoma and possible adverse events associated with chlorambucil, physical and clinical examinations, including blood tests, radiography, and ultrasound, were carried ouin the cat every 2–3 months. However, no abnormalities and no adverse events had been observed in the treatment period. On day 754, the cat was administered with the same dosage of chlorambucil and remained in good condition. DiscussionAlthough nasal irrigation with saline or administration of enrofloxacin might have contributed to the short-term resolution of clinical signs, chlorambucil was considered to enable a cat’s long-term management of nasopharyngeal B-cell lymphoma without masses. No adverse events were observed in the cat in the period of the treatment with chlorambucil. A previous study reported that no masses were evident in 28% of cats with nasal or nasopharyngeal lymphoma manifesting as a rough thickened mucosa (Santagostino et al., 2015), indicating that nasal and nasopharyngeal lymphomas without masses are not uncommon in cats. Although the effect of combined chlorambucil and prednisolone was not evaluated in this case, the present report suggests that at least chlorambucil can be a therapeutic option for feline nasal and nasopharyngeal lymphomas without masses. The cat in this case report was diagnosed with nasopharyngeal large B-cell lymphoma based on histopathological and immunohistochemical analyses. Large-cell lymphomas tend to behave aggressively and develop as enlarged neoplasm in the tissue. However, rhinoscopy and diagnostic imaging with radiography, ultrasound, and CT revealed no masses, local invasions, or metastases to the local lymph nodes and other tissues or organs in the cat, suggesting that nasopharyngeal lymphoma in the cat may not be aggressive. Alternatively, nasopharyngeal lymphoma in the cat might have been in an early stage of tumor development. However, this assumption was not supported by the 8-month history of clinical signs, including nasal discharge, sneezing, and mild epistaxis. A plausible explanation for our assumption could be that P. aeruginosa induced chronic rhinitis, and then nasopharyngeal lymphoma developed. Although it is unclear when nasopharyngeal lymphoma occurred in the cat, it would not have been very long before the referral to our hospital. A recent case report showed that a functional endoscopic sinus surgery completely removed localized stage I nasal lymphoma without local invasions or metastases in a cat, resulting in no recurrences for 15 postoperative months (Marchesi et al., 2019). In this report, chlorambucil was effective for stage I lymphoma localized to the nasopharyngeal mucosa, and no recurrences of clinical signs were observed for more than 25 months. These case reports collectively suggest that early medical, surgical, or radiation intervention to the localized stage I lymphoma in the nasal cavity may lead to long-term clinical remission in cats. Long-term management was accomplished by treatment with chlorambucil in the cat. However, since follow-up CT or rhinoscopy could not be carried out, it was not determined whether chlorambucil induced complete remission in the cat. The nature of nasopharyngeal large-cell lymphoma in the cat is considered malignant and aggressive. Therefore, the recurrences of nasopharyngeal lymphoma should be monitored in the cat. In conclusion, the present case report demonstrated that chlorambucil led to long-term clinical signs’ resolution without any side effects in a cat with nasopharyngeal B-cell lymphoma without masses, local invasions, or metastases. The findings of this case suggest that chlorambucil can be a treatment option for an early stage of localized nasal or nasopharyngeal lymphoma in cats. However, to determine which type of feline lymphoma in the nasal cavity responds to chlorambucil, further studies should be carried out in a large population of cats with nasal or nasopharyngeal lymphoma. Authors’ contributionsK.T. and K.O. wrote the paper; K.T., T.B., M.H., and M.M managed the case; M.K. analyzed the CT images; H.K. made the pathological diagnosis; K.T., J.K., and K.O. analyzed all clinical data; K.O. supervised the case. All authors have read and agreed to the published version of the manuscript. Conflict of interestThe authors declare that there is no conflict of interest. ReferencesFerguson, S., Smith, K.C., Welsh, C.E. and Dobromylskyj, M.J. 2020. A retrospective study of more than 400 feline nasal biopsy samples in the UK (2006-2013). J. Feline Med. Surg. 22, 736–743. Haney, S.M., Beaver, L., Turrel, J., Clifford, C.A., Klein, M.K., Crawford, S., Poulson, J.M. and Azuma, C. 2009. Survival analysis of 97 cats with nasal lymphoma: a multi-institutional retrospective study (1986-2006). J. Vet. Intern. Med. 23, 287–294. Henderson, S.M., Bradley, K., Day, M.J., Tasker, S., Caney, S.M., Hotston Moore, A. and Gruffydd-Jones, T.J. 2004. Investigation of nasal disease in the cat--a retrospective study of 77 cases. J. Feline Med. Surg. 6, 245–257. Little, L., Patel, R. and Goldschmidt, M. 2007. Nasal and nasopharyngeal lymphoma in cats: 50 cases (1989-2005). Vet. Pathol. 44, 885–892. Marchesi, M.C., Valli, L., Angeli, G., Savastano, V. and Caivano, D. 2019. Functional endoscopic sinus surgery in a cat with nasal tumor. J. Vet. Med. Sci. 81, 1219–1222. Moore, A. 2013. Extranodal lymphoma in the cat: prognostic factors and treatment options. J. Feline Med. Surg. 15, 379–390. Paulin, M.V., Couronné, L., Beguin, J., Le Poder, S., Delverdier, M., Semin, M.O., Bruneau, J., Cerf-Bensussan, N., Malamut, G., Cellier, C., Benchekroun, G., Tiret, L., German, A.J., Hermine, O. and Freiche, V. 2018. Feline low-grade alimentary lymphoma: an emerging entity and a potential animal model for human disease. BMC Vet. Res. 14, 306. Santagostino, S.F., Mortellaro, C.M., Boracchi, P., Avallone, G., Caniatti, M., Forlani, A. and Roccabianca, P. 2015. Feline upper respiratory tract lymphoma: site, cyto-histology, phenotype, FeLV expression, and prognosis. Vet. Pathol. 52, 250–259. Sfiligoi, G., Théon, A.P. and Kent, M.S. 2007. Response of nineteen cats with nasal lymphoma to radiation therapy and chemotherapy. Vet. Radiol. Ultrasound. 48, 388–393. Taylor, S.S., Goodfellow, M.R., Browne, W.J., Walding, B., Murphy, S., Tzannes, S., Gerou-Ferriani, M., Schwartz, A. and Dobson, J.M. 2009. Feline extranodal lymphoma: response to chemotherapy and survival in 110 cats. J. Small Anim. Pract. 50, 584–592. | ||
| How to Cite this Article |
| Pubmed Style KT, TB, MH, MM, MK, JK, HK, Ohmori K. Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil. Open Vet J. 2021; 11(2): 217-221. doi:10.5455/OVJ.2021.v11.i2.5 Web Style KT, TB, MH, MM, MK, JK, HK, Ohmori K. Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil. https://www.openveterinaryjournal.com/?mno=50160 [Access: July 27, 2024]. doi:10.5455/OVJ.2021.v11.i2.5 AMA (American Medical Association) Style KT, TB, MH, MM, MK, JK, HK, Ohmori K. Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil. Open Vet J. 2021; 11(2): 217-221. doi:10.5455/OVJ.2021.v11.i2.5 Vancouver/ICMJE Style KT, TB, MH, MM, MK, JK, HK, Ohmori K. Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil. Open Vet J. (2021), [cited July 27, 2024]; 11(2): 217-221. doi:10.5455/OVJ.2021.v11.i2.5 Harvard Style , K. T., , . T. B., , . M. H., , . M. M., , . M. K., , . J. K., , . H. K. & Ohmori, . K. (2021) Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil. Open Vet J, 11 (2), 217-221. doi:10.5455/OVJ.2021.v11.i2.5 Turabian Style , Kaho Takahashi, Takashi Baba, Marin Hirokawa, Masaki Miyajima, Miori Kishimoto, Junpei Kimura, Hirotaka Kondo, and Keitaro Ohmori. 2021. Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil. Open Veterinary Journal, 11 (2), 217-221. doi:10.5455/OVJ.2021.v11.i2.5 Chicago Style , Kaho Takahashi, Takashi Baba, Marin Hirokawa, Masaki Miyajima, Miori Kishimoto, Junpei Kimura, Hirotaka Kondo, and Keitaro Ohmori. "Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil." Open Veterinary Journal 11 (2021), 217-221. doi:10.5455/OVJ.2021.v11.i2.5 MLA (The Modern Language Association) Style , Kaho Takahashi, Takashi Baba, Marin Hirokawa, Masaki Miyajima, Miori Kishimoto, Junpei Kimura, Hirotaka Kondo, and Keitaro Ohmori. "Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil." Open Veterinary Journal 11.2 (2021), 217-221. Print. doi:10.5455/OVJ.2021.v11.i2.5 APA (American Psychological Association) Style , K. T., , . T. B., , . M. H., , . M. M., , . M. K., , . J. K., , . H. K. & Ohmori, . K. (2021) Long-term management of a cat with nasopharyngeal lymphoma by chlorambucil. Open Veterinary Journal, 11 (2), 217-221. doi:10.5455/OVJ.2021.v11.i2.5 |