Open Veterinary Journal, (2021), Vol. 11(3): 431–435
Case Report
10.5455/OVJ.2021.v11.i3.15
An unusual case of traumatic dorsolateral sacral hernia with retroflexion of the urinary bladder in a cat
Çağrı Gültekin*  , Gül Çıray Akbaş
, Gül Çıray Akbaş and Deniz Seyrek-İntaş
and Deniz Seyrek-İntaş
Department of Surgery, Faculty of Veterinary Medicine, Near East University, Nicosia, Cyprus
*Corresponding Author: Çağrı Gültekin. Department of Surgery, Faculty of Veterinary Medicine, Near East University, Nicosia, Cyprus. Email: cagri.gultekin [at] neu.edu.tr
Submitted: 08/06/2021 Accepted: 14/07/2021 Published: 18/08/2021
© 2021 Open Veterinary Journal
This is an Open Access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License (http://creativecommons.org/licenses/by-nc-nd/4.0/), which permits non-commercial re-use, distribution, and reproduction in any medium, provided the original work is properly cited, and is not altered, transformed, or built upon in any way.
Abstract
Background: Perineal hernias are rarely seen in cats and can be caused by congenital or trauma. The urinary bladder is the most herniated organ and was being observed in prepubic, ventral perineal, umbilical, or caudoventral abdominal regions.
Case Description: A 1-year-old female domestic short-haired cat was presented to the Animal Hospital of the Near East University Faculty of Veterinary Medicine with complaints of urinary retention as well as the inability to defecate. The patient owner reported that the cat had been struck by a car around 4 months previously, which resulted in a pelvic fracture. On clinical examination, a fluctuating mass was detected in the dorso-lateral region of the pelvis. After radiographic and ultrasonographic examination, the mass was diagnosed as the urinary bladder. A cystopexy operation was performed on the urinary bladder, which herniated through a muscular tear to the right dorsolateral pelvic region.
Conclusion: Unusual case report of a sacral hernia resulting from a traumatic rupture of the sacral muscles together with urinary bladder retroflexion was reported in a cat.
Keywords: Cystopexy, Feline, Pelvic fractures, Retroflexion, Sacral hernia.
Introduction
One of the most common causes of pelvic trauma of outdoor or stray cats is traffic accidents. This is commonly seen in young cats and causes rupture of organs, bleeding, hernias, and numerous neurologic problems along with orthopaedic problems (Meeson and Corr, 2011). A hernia is defined as the dislocation of an organ or other bodily structures through a congenital or traumatic defect or tear in the wall that usually contains it. Abdominal wall hernias and ruptures can be seen in cats as congenital or acquired inguinal canal hernias (Zulauf et al., 2007; de la Vega et al., 2018). Perineal hernias are rare in cats. Even though they can be unilateral, they have been mostly observed bilaterally. Perineal hernia can be caused by long-term complications of the perineal urethrostomy or megacolon (Mann et al., 2014). When the pelvic muscle structure is disrupted, the urinary bladder can flip caudally to pass from the abdomen to the pelvic or perineal region; in other words, retroflexion occurs. Retroflexion of the urinary bladder is encountered in 20% of perineal hernia cases (Yool, 2012). Clinical symptoms of bladder retroflexion include stranguria, dysuria, and anuria. Emergency surgery is required when the bladder cannot be emptied or repositioned (Mann et al., 2014). This case report describes the clinical findings, diagnostics, and operative treatment of an unusual case involving a sacral hernia resulting from a traumatic rupture of the sacral muscles together with urinary bladder retroflexion in a cat.
Case Details
A 1-year-old female domestic short-haired cat struck by a car 4 months previously was referred to the Animal Hospital of the Near East University Faculty of Veterinary Medicine with weakness, lack of appetite, dysuria and dyschezia. Conservative treatment had been recommended for multiple pelvic fractures in another veterinary clinic. One month after the traffic accident, the cat was presented to the same clinic with complaints of stranguria, haematuria, anuria and was diagnosed with and treated for cystitis.
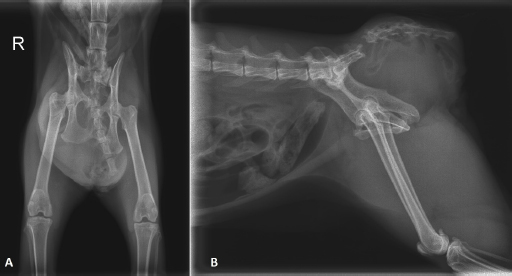
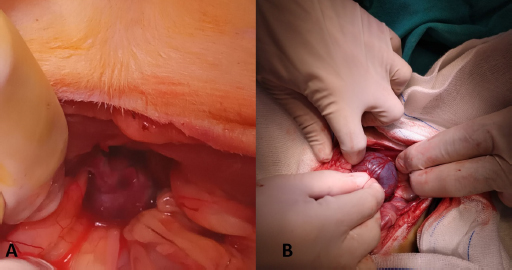
On clinical examination, the cat was in moderate general condition. On inspection, an asymmetry in the pelvic region was noted, and a fluctuant mass in the right dorso-lateral region of the pelvis could be palpated (Fig. 1). The urinary bladder could not be detected on abdominal palpation. On rectal palpation, the cat showed pain, and the mass noticeable from the outside was felt in the right dorsolateral pelvic region, and some faeces were detected. However, perineal muscle structures and anal reflexes could not be determined. The pelvis's right-lateral and ventral-dorsal radiographs revealed sacrococcygeal avulsion with a left caudodorsal dislocation of the sacral vertebrae. There was sacroiliac separation with cranial dislocation of the right hemipelvis.
Additionally, a fracture of the right ramus cranialis with dislocation and a fracture of the tabula ossis ischii with some callus formation. A round shaped, homogeneous soft tissue opacity ventral to the sacral vertebrae extends toward the right side, displacing the rectum dorsally. The urinary bladder was not visible in the caudal abdominal region (Fig. 2). There was no urinary bladder in the abdomen on ultrasound. Examination of the right sacral region with the mass revealed a fluid-filled structure directly under the skin without any evidence of sacral muscles. This structure was identified as the urinary bladder, with anechoic content and a normal wall. No urine flow could be elicited by gently massaging the urinary bladder.
Based on history, clinical, radiographical, and ultrasonographical findings, a traumatic herniation with retroflexion of the urinary bladder to the right sacral region was diagnosed. The decision was made to take the patient into an emergency operation. For preoperative antibiotherapy, Ceftriaxone (Equiceft 1 g vial, TümEkip) was administered intravenously at the dose of 30 mg/kg. For analgesia, Tramadol HCl (Tramosel 100 mg/2 ml ampoule, Haver) at the dose of 2 mg/kg IV, and Meloxicam (Anaflex 0.5% 100 ml vial, Hektaş) at the dose of 0.02 mg/kg SC were applied for 3 days. For the epithelization of the urinary bladder Dexpanthenol (Bepanthen 500 mg/2 ml ampoule, Bayer) was given at a dose of 11 mg/kg IV. CRI of 5% dextrose-lactated ringer (Poliflex, 1,000 ml solution, Polifarma) was given at a dose of 30 ml/hour.
Anaesthesia was induced by IV administration of Propofol (Propofol-lipuro 10 mg/ml, 10 ml ampoule, Braun) at a dose of 6 mg/kg before endotracheal intubation. Maintenance of anaesthesia was provided with Sevoflurane (Sevorane liquid, 250 ml vial, Abbvie) oxygen mixture. Access to the abdominal cavity was performed via a ventral midline incision in dorsal recumbency. The distended bladder was carefully removed manually from the sacral region and repositioned to its normal place in the abdomen (Fig. 3). Intraoperatively, the outer surface of the bladder appeared fragile and showed a dark red discoloration, with some regions more severely affected. Neither a structural abnormality of the organs nor any other herniated structures were observed in the abdominal cavity. Intraoperative catheterization of the urinary bladder was performed, and the bladder was rinsed with 0.9% NaCl solution. Ventral abdominal cystopexy was performed using a simple interrupted pattern, and the abdomen was closed routinely. Postoperatively, antibiotics, analgesics, and fluid therapy were continued. On the 2nd day postoperatively, swelling of the right sacral region and severe tenesmus and pain were observed, and it was determined that the bladder was herniated again on ultrasound. The patient was re-operated. Intraoperatively, the bladder stitches appeared ruptured, and the outer surface of the bladder was even darker red and fragile. It was observed that the bladder colour began to return to normal after repositioning. The urinary bladder was fixed by the ventral abdominal cystopexy method using a continuous locking suture technique. Haematuria was detected on the first postoperative day of the repeated operation, but the patient's general condition was good. On the 2nd postoperative day, the urine returned to normal, and the patient was discharged. However, the day after discharge, the patient owner informed us that the patient had died. Our request for a necropsy to determine the cause of death was declined.
Discussion
Hernias in cats are usually seen as diaphragmatic or inguinal hernias due to trauma (Zulauf et al., 2007; Meeson and Corr, 2011; de la Vega et al., 2018). The unilateral perineal hernia is rare in cats. Bladder hernias have been observed in prepubic, ventral perineal, umbilical, or caudoventral abdominal regions (Risselada et al., 2003; Vnuk et al., 2005; Neville-Towle and Sakals, 2015; Rizk and Samy, 2016). In our case, as a result of the clinical and imaging examinations performed, the location of the urinary bladder in the dorso-lateral of the os ischii, which extends toward the os ilium, presented a different appearance from the reported hernia cases.

Fig. 1. A fluctuant mass in the right dorso-lateral region of the pelvis was found on clinical examination.
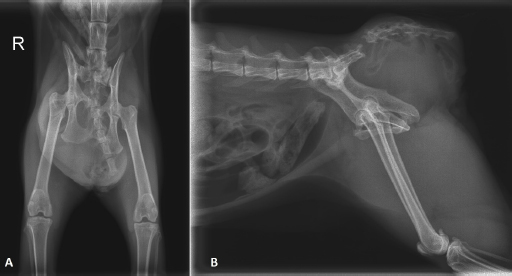
Fig. 2. Ventrodorsal (A) and right-lateral (B) radiographs of the pelvis.
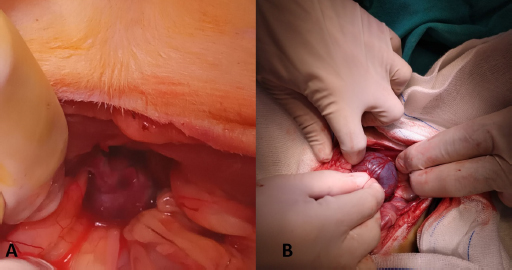
Fig. 3. Intraoperative appearance of the displaced urinary bladder to the sacral area (A), manual repositioning of the urinary bladder (B).
Due to the large muscle masses surrounding the pelvis, severe traumatic force must fracture the pelvic bones. Therefore, in more than half of traumatic cases, non-orthopaedic injuries occur mostly in cats and less frequently in dogs (Meeson and Corr, 2011). In a study with female dogs conducted by Hayashi et al. (2016), it was reported that pelvic traumas that are not properly treated can predispose dogs to perineal hernia. Rectal tone and perineal reflex may decrease due to pudendal or caudal rectal nerve damage. Additionally, there is no effective treatment for the reinnervation of the external anal sphincter muscle (Snow, 2016). Also, sacrococcygeal fractures or luxations /subluxations may be seen in traffic accidents or what is known as tail pull injury cases. In these cases, pudendal or pelvic nerve damage occurs due to the effect of sacrococcygeal nerve or cauda equina. As a result, temporary or permanent damage may occur, and difficulty in urinating can be seen due to insufficient urethral relaxation and contraction of the detrusor muscles. Prognosis is determined by the presence of the anal reflex and perineal sensation. It is stated that the damage is permanent in cats that cannot urinate normally after 1 month (Eminaga et al., 2011). In this case, partial healing was seen in the pelvic bones during the 4 months after the trauma. Possible neurological and muscle damage cannot be reliably determined radiographically. For this purpose, advanced imaging techniques should be used. In the presented case, loss of tone in the anal sphincter on rectal palpation may have been due to pudendal/caudal rectal or pelvic nerve damage resulting from sacrococcygeal luxation. Cystitis developing 1 month after trauma may be the first sign of possible neurological damage affecting the urinary bladder. It was thought that retroflexion of the urinary bladder could have been caused by increased dysuria and abdominal contractions due to progressive neurological damage.
The pelvic diaphragm consists of the levator ani and coccygeal muscles and the inner and outer perineal fascia. Furthermore, the borders of the perineum are formed by the sacrotuberous ligaments, which are not found in cats, and the superficial gluteal muscles laterally, the caudal vertebrae dorsally and the ischium ventrally (Mann et al., 2014). Most hernias occur between the levator ani, external anal sphincter, and internal obturator muscles (caudal hernia); however, some hernias occur between the sacrotuberous ligament and the coccygeal muscle (sciatic hernia), the levator ani and coccygeal muscles (dorsal hernia), or the ischiourethralis, bulbocavernosus, and ischiocavernosus muscles (ventral hernia) (Fossum, 2013). In our case, the unilateral swelling was not located around the anus but in the sacral region and more dorsally. On rectal palpation, the pelvic muscles could not be palpated on the right side. On ultrasonographic examination, continuity could not be determined in the sacral region muscles. The rupture of the coccygeal and levator ani muscles due to sacrococcygeal luxation, together with the cranial displacement of the right pelvic half by sacroiliac separation, likely suggests that the superficial gluteal muscle was also ruptured. Therefore, we think that it would be more accurate to describe the case as a sacral hernia.
Postoperative complications of perineal hernia cases include sciatic nerve damage, faecal incontinence, infection at the incision line, rectal prolapse associated with severe tenesmus, incorrect placement of stitches in the anal sacs or rectal lumen, bladder necrosis, urinary incontinence and recurrence of perineal hernia (Mann et al., 2014). In perineal hernias, methods such as cystopexy and colopexy and herniorrhaphy are recommended to prevent a recurrence. However, it was observed that the recurrence rate in dogs on which cystopexy was performed without herniorrhaphy was found to be similar to that in dogs on whom cystopexy and herniorrhaphy were performed (Risselada et al., 2003). However, herniorrhaphy techniques recommended in dogs are difficult to apply in cats due to their smaller muscles and lack of sacrotuberous ligament (Mann et al., 2014). In our case, the recurrence of bladder retroflexion was observed, and it was determined that this was caused by the rupture of the sutures in the first cystopexy operation. In the retroflexion case, it was concluded that the continuous locking suture technique was more effective than the simple interrupted suture technique applied in the first operation. Although 3 months had passed since the trauma and there was partial recovery of the fractures, and infrastructure that could be reconstructed in the sacral muscles of the cat could not be determined. Therefore, it was decided that the sacral muscle tear could not be repaired with herniorrhaphy, and intraoperative cystopexy would be sufficient.
Retroflexion of the bladder can affect the nerves that innervate the bladder and urethral sphincter, causing bladder atony by stretching the detrusor muscle or blocking blood flow to the bladder. In addition, bladder necrosis causes obstruction and enlargement and is seen in long-lasting cases. The necrotic part of the bladder can be resected, if present, but widespread necrosis may prevent successful resection. Secondary clinical findings in necrosis of the urinary bladder are rupture and uroperitoneum (Mann et al., 2014). In the presented case, the dark red colour and fragile structure of the outer surface of the urinary bladder was remarkable. Petechial bleeding foci were seen in some areas. There was no obvious necrotic focus in the urinary bladder. Resection was not performed because the colour returned to normal after bladder reposition, and the bladder was left to heal spontaneously. Although haematuria was observed after the first operation, it was observed that urine returned to normal after the second operation. The patient died the day after discharge. Our necropsy request was not approved by the patient’s owner. Therefore, the cause of death could not be determined. However, atony of the bladder and insufficient blood flow are consistent with intraoperative discoloration findings of the bladder. It was thought that the treatment continued and the bladder, which was left to heal spontaneously, did not respond to the treatment and necrosis developed, and therefore, bladder rupture and/or uroperitoneum developed as the cause of death.
Determination of soft tissue and possible neurological damage is as important as orthopaedic treatment in pelvic fractures. In our case, the pelvic fractures healed partially. However, 3 months after the trauma, sacral retroflexion of the urinary bladder was detected by clinical examination and diagnostic imaging techniques. Anatomically, the asymmetric structure of the pelvic region and rupture in the sacral muscles, together with sacrococcygeal luxation, should be considered the differential diagnosis that may cause retroflexion of the urinary bladder sacral region.
Acknowledgments
The authors would like to thank E-Study Box for the English language proofreading.
Conflict of interest
The authors declare that there is no conflict of interest.
Authors contributions
Deniz Seyrek-İntaş performed the diagnosis on radiographical and ultrasonographical examination. Çağrı Gültekin and Gül Çıray Akbaş performed on clinical examination and operation. All the authors contributed for the manuscript.
References
de la Vega, M., Townsend, K.L., Terry, J. and Nemanic, S. 2018. Urinary bladder herniation through inguinal ring in a female cat. Can. Vet. J. 59, 1085–1088.
Eminaga, S., Palus, V. and Cherubini, G.B. 2011. Acute spinal cord injury in the cat: causes, treatment and prognosis. J. Feline Med. Surg. 13, 850–862.
Fossum, T.W. 2013. Small animal surgery. Elsevier Health Sciences, Alpharetta, GA, pp: 568–573.
Hayashi, A.M., Rosner, S.A., de Assumpcao, T.C.A., Stopiglia, A.J. and Matera, J.M. 2016. Retrospective study (2009–2014): perineal hernias and related comorbidities in bitches. Top. Companion Anim. Med. 31, 130–133.
Mann, F.A., Constantinescu, G.M. and Anderson, M.A. 2014. Hernias. In Current techniques in small animal surgery. Eds., Bojrab. M.J., Waldron, D.R., Toombs, J.P. Jackson, WY: Teton New Media, pp: 564–588.
Meeson, R. and Corr, S. 2011. Management of pelvic trauma: neurological damage, urinary tract disruption and pelvic fractures. J. Feline Med. Surg. 13, 347–361.
Neville-Towle, J. and Sakals, S. 2015. Urinary bladder herniation through a caudoventral abdominal wall defect in a mature cat. Can. Vet. J. 56, 934–936.
Risselada, M., Kramer, M., Van de Velde, B., Poils, I. and Görtz, K. 2003. Retroflexion of the urinary bladder associated with a perineal hernia in a female cat. J. Small Anim. Pract. 44, 508–510.
Rizk, A. and Samy, A. 2016. Diagnosis and surgical repair of entero-cystocele in a cat. Open Vet. J. 6, 162–163.
Snow, L.A. 2016. Perineal herniorrhaphy. In: Complications in small animal surgery. Eds., Griffon, D., Hamaide, A. Hoboken, NJ: John Wiley & Sons. pp: 388–394.
Vnuk, D., Babic, T., Stejskal, M., Capak, D., Harapin, I. and Pirkic, B. 2005. Application of a semitendinosus muscle flap in the treatment of perineal hernia in a cat. Vet. Rec. 156, 182–183.
Yool, D.A. 2012. Small animal soft tissue surgery. Wallingford, UK: CAB International, pp: 149–171.
Zulauf, D., Voss, K. and Reichler, I.M. 2007. Herniation of the urinary bladder through a congenitally enlarged inguinal canal in a cat. Schweiz. Arch. Tierheilkd. 149, 559–562.