| Research Article | ||
Open Veterinary Journal, (2024), Vol. 14(1): 577-585 Original Research Antimicrobial resistance from one health perspective in the Middle East: A systematic reviewKhalid A. Alkheraije*Department of Veterinary Medicine, College of Agriculture and Veterinary Medicine, Qassim University, Buraidah, Saudi Arabia *Corresponding Author: Khalid A. Alkheraije. Department of Veterinary Medicine, College of Agriculture and Veterinary Medicine, Qassim University, Buraidah, Saudi Arabia. Email: k.alkheraije [at] qu.edu.sa Submitted: 01/10/2023 Accepted: 15/12/2023 Published: 31/01/2024 © 2024 Open Veterinary Journal
AbstractBackground: Antimicrobial resistance (AMR) is recognized globally as a significant health challenge, but its extent remains unclear in many regions. It is crucial to prioritize a foundational evaluation of AMR prevalence to facilitate the implementation of laboratory-based surveillance. Adopting a One Health perspective, this study outlines the present AMR status in the Middle East. Aim: To synthesize the current state of knowledge on AMR in the Middle East, delineate the contributions of different sectors (human health, animal health, and environment), and discern the effectiveness of One Health interventions in mitigating AMR. Methods: An exhaustive literature search was conducted via PubMed, ScienceDirect, and Google Scholar. Potential articles were screened and assessed for eligibility based on prescribed eligibility criteria. Data synthesis was done, and the results were reported and discussed thematically. Results: Twenty-three studies were included in the study and published between 2019 and 2023. Most studies reveal substantial challenges in treating infections, with a significant prevalence of resistance in critical care units, particularly against extended-spectrum beta-lactamases and carbapenem-resistant Gram-negative bacteria. Colistin and imipenem resistance in pediatric populations further emphasize the urgency of understanding and addressing diverse resistance mechanisms in the region. Studies on urinary pathogens, bacteremia, and biofilm formation highlight the multifaceted challenge of AMR. The emergence of resistance to key antibiotics emphasizes the urgency for tailored treatment strategies. Conclusion: Given the interconnectedness of human, animal, and environmental health, a One Health perspective is imperative. The diverse challenge demands coordinated efforts, including innovative interventions and public health policies. Bridging existing gaps through future research is crucial for evidence-based and context-specific strategies in combating AMR in the region. Keywords: Antimicrobial resistance, One Health, Middle East. IntroductionA ntimicrobial resistance (AMR) is a global public health emergency, challenging our ability to combat bacterial infections. In their pursuit of improving health and agricultural productivity, middle-income countries often misuse antimicrobials, contributing to widespread resistance (Tadesse et al., 2017). The lack of awareness among farmers and the extensive use of food-producing animals are vital factors (Tadesse et al., 2017). In our interconnected world, AMR can swiftly spread across humans, animals, plants, and the environment, undermining infection treatment and causing economic repercussions. The escalating threat of AMR requires a One Health approach, recognizing the interdependence of humans, animals, and the environment (Adisasmito et al., 2022). Our investigation centers on the One Health paradigm, acknowledging human, animal, and environmental health links. Rudolf Virchow's concept of "zoonosis" in the 19th century and Calvin Schwabe's "one medicine" underscored these connections (Schwabe, 1964). In the Middle East, unique socio-economic factors contribute to the complexity of AMR, requiring region-specific interventions. This study explores the interplay between One Health and AMR in the Middle East, aiming to uncover patterns, identify gaps, and provide insights for targeted interventions. Our systematic review will offer stakeholders and policymakers a robust foundation for informed decision-making in the fight against AMR in this region. What is the current state of AMR in the Middle East, and how do different sectors, including human health, animal health, and the environment, contribute to the development and spread of AMR? Furthermore, what evidence exists regarding the effectiveness of One Health interventions in mitigating AMR in the Middle East? Hence, the primary objectives are to synthesize the current state of knowledge on AMR in the Middle East, delineate the contributions of different sectors (human health, animal health, and environment), and discern the effectiveness of One Health interventions in mitigating AMR. Materials and MethodsThis study followed preferred reporting items for systematic review and meta-analysis (PRISMA) 2020 guidelines (Page et al., 2021). Identification and selection of studiesSearch strategyThe search strategy involved a combination of keywords in different combinations including antimicrobial, antibiotic, drug, Gram-negative, Gram-positive, one-health, and Middle East. In addition, specific infections and countries in the Middle East were included in the search strings. Eligibility criteriaInclusion criteriaAll studies had to meet the following pre-defined inclusion criteria:
Exclusion criteriaStudies that satisfied the following criteria were excluded:
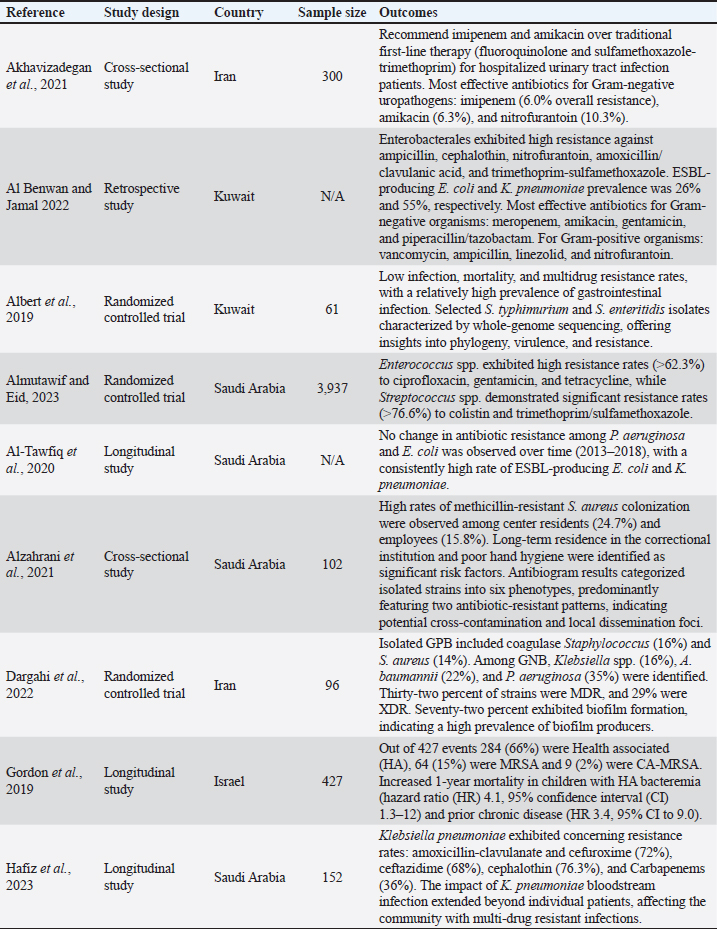
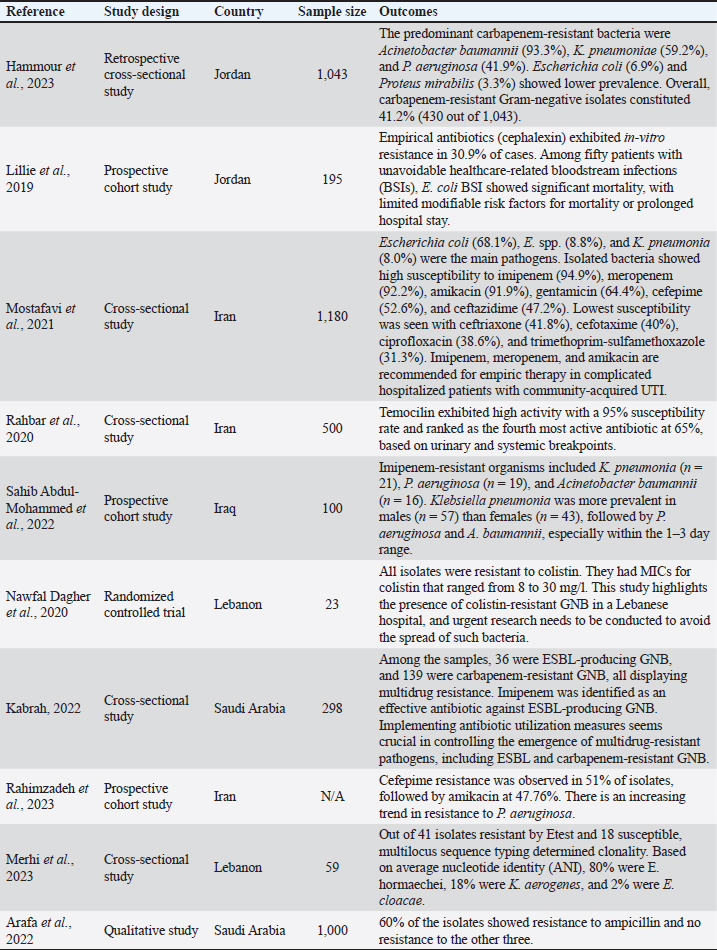
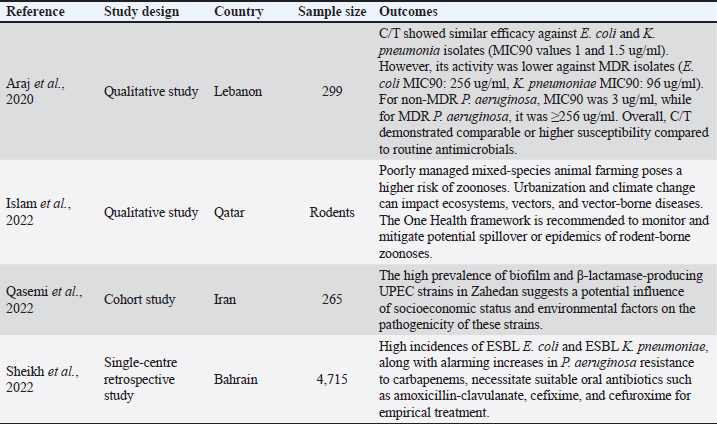
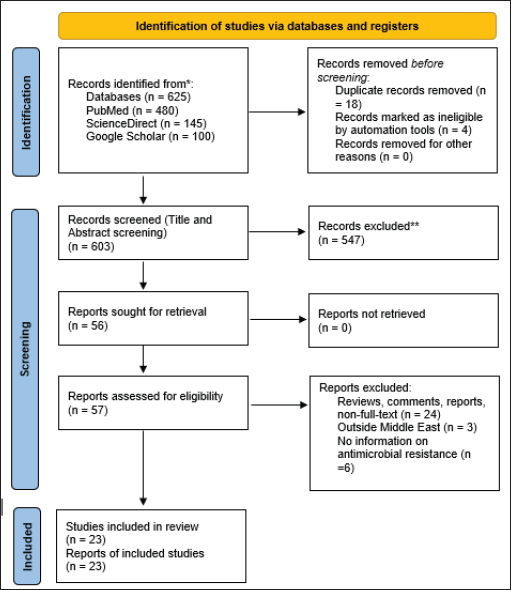
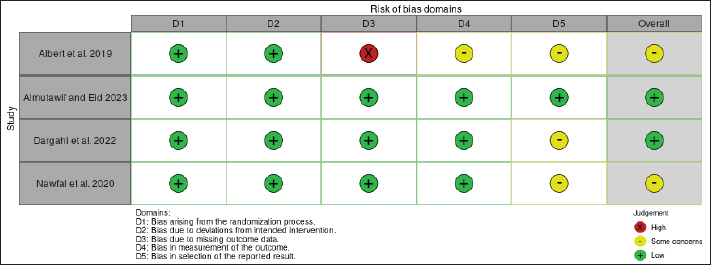
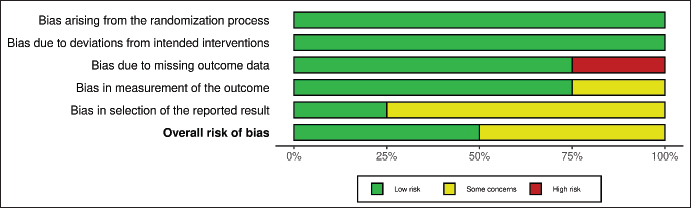
Data selection and extractionInformation was collected from each study using a form and a database specifically created for this study, utilizing a Microsoft Excel spreadsheet. Data extracted included article information (Author, year of publication, study design, country, total number of participants, and outcomes). Methodological quality assessmentThe Cochrane Organization's Risk of Bias 2 tool was employed to evaluate the quality of the study (Sterne et al., 2019). The risk of bias graph and summary plot were generated using the Robvis visualization tool. In addition, the National Institutes of Health quality assessment tool for observational cohort and cross-sectional studies was employed to evaluate the quality of the study (Armijo-Olivo et al., 2012). Data analysisData were systematically extracted and organized using Microsoft Excel 2021. The extracted data are presented in Table 1, showing the author (s), study design, sample size, and outcomes. Ethical approvalNot needed for this study. ResultsStudy selectionInitially, 625 articles were retrieved through the search process. After applying eligibility criteria during the screening process, 547 articles were excluded. The remaining 57 articles underwent a full-text review, and 34 were excluded as they did not fully meet the eligibility criteria. It is essential to highlight that some articles were excluded for multiple reasons. Ultimately, only 23 articles met all the inclusion criteria and were included in the study. Figure 1 represents the PRISMA flowchart summarizing the subsequent data screening procedure. Methodological quality assessment resultsFigures 2 and 3 show the quality assessment results. Data selection and extractionData were systematically extracted and presented in Table 1. Study characteristics and thematic analysis of outcomesThe investigation into AMR in Middle Eastern healthcare settings reveals complexity, as demonstrated by a study at King Faisal Hospital in Saudi Arabia (Kabrah, 2022). In this cross-sectional study of 298 patients with central venous catheters, a substantial challenge emerged in treating intensive care unit infections. Notably, 175 patients exhibited resistance to extended-spectrum beta-lactamases (ESBL) and carbapenem-resistant Gram-negative bacteria (GNB), highlighting the difficulty in managing such infections and the urgent need for effective strategies in critical care settings. Colistin resistance, explored by Nawfal Dagher et al. (2020) through rectal swabs, exposed the prevalence of resistance as all eight clinical strains isolated exhibited resistance to colistin. This finding emphasizes the urgency of understanding diverse resistance mechanisms present in the region. A study by Rahbar et al. (2020) on the investigation into urinary pathogens highlighted the potential of temocillin in treating infections caused by ESBL-producing Escherichia coli and K. pneumoniae, advocating for exploring alternative treatments for common infections in the region. Pediatric populations, as explored by Sahib Abdul-Mohammed et al. (2022), showcased a concerning trend of imipenem resistance. Among identified isolates, A. baumannii, P. aeruginosa, and K. pneumoniae exhibited resistance, with A. baumannii prevalent in both blood and urine samples, underlining the diverse sources of resistant bacteria in pediatric patients. A cross-sectional study by Mostafavi et al. (2021) on community-acquired urinary tract infections emphasized E. coli as the predominant pathogen, with imipenem, meropenem, and amikacin identified as effective choices for severe cases, reinforcing the importance of tailored empirical therapy. Table 1. Study descriptor table.
A retrospective study by Hammour et al. (2023) identified A. baumannii, K. pneumoniae, and P. aeruginosa as the most prevalent carbapenem-resistant bacteria, necessitating targeted interventions to address antibiotic resistance in the population. A study by Hafiz et al. (2023) assessment of K. pneumoniae bacteremia in Saudi Arabia revealed the impact at the patient and community levels, emphasizing the broader implications of multidrug-resistant infections. Research by Gordon et al. (2019) on Staphylococcus aureus bacteremia in children insisted on the association between Methicillin-resistant Staphylococcus aureus (MRSA) and increased long-term mortality in healthcare-associated cases. Biofilm formation in endotracheal tubes, as studied by Dargahi et al. (2022), revealed the prevalence of biofilm-producing Gram-positive bacteria (GPB), with colistin and linezolid identified as effective antibiotics against resistant GNB and GPB isolates. In a detention center, Alzahrani et al. (2021) found high rates of MRSA colonization among residents and employees, attributing it to poor personal hygiene and inadequate infection control measures. A cross-sectional study by Akhavizadegan et al. (2021) on antibiotic resistance in uropathogens indicated higher resistance rates in inpatient samples, emphasizing the importance of tailored treatment strategies. Araj et al.'s (2020) findings on Ceftolozane/Tazobactam (C/T) revealed high activity against ESBL-producing E. coli and K. pneumoniae, indicating its potential as a minimally toxic and resistance-reducing alternative treatment. These results underscore the pressing need for coordinated efforts to address AMR in the Middle East, adopting a One Health perspective to tackle this critical public health challenge. In the quantitative analysis of mortality outcomes across the included studies, varying mortality rates were observed, as shown in Table 1. Albert et al. (2019) reported a mortality rate of 6.56%, with 4 out of 61 patients succumbing to the antibiotic therapy. Similarly, Gordon et al. (2019) reported a mortality rate of 17.56%. Hafiz et al. (2023) reported the highest mortality rate among the studies, with 48 deaths out of 148 patients, yielding a mortality rate of 32.43%. Lillie et al. (2019) reported a mortality rate of 23.40%. DiscussionThis study of AMR from a One Health perspective in the Middle East reveals a complex landscape marked by resistance patterns in various clinical settings. The comprehensive exploration of diverse studies emphasizes the urgent need for coordinated efforts to address this region's multifaceted challenge of AMR. The prevalence of resistance observed in critical care units, as demonstrated by Kabrah (2022) is a stark reminder of the urgent need for tailored treatment strategies in these high-stakes environments. This finding emphasizes the critical role of targeted interventions in managing infections within intensive care units. Moreover, the widespread resistance, exemplified by colistin-resistant isolates (Nawfal Dagher et al., 2020), raises significant concerns about the efficacy of current therapeutic approaches. Colistin resistance, often considered a last-resort antibiotic, highlights the challenges in treating infections caused by multidrug-resistant strains. The potential implications for patient outcomes and the broader healthcare system further emphasize the urgency to address these challenges.
Fig. 1. PRISMA flow diagram showing results of the study selection (Page et al., 2021). Comparing our findings with existing literature brings to light the distinctive patterns of resistance observed in the Middle East. The noteworthy carbapenem resistance rates across various bacteria, as evidenced by Hammour et al. (2023), set the region apart globally. This highlights the necessity for tailored strategies, acknowledging the unique challenges and contributing factors specific to the Middle East. Furthermore, the community-level impact of multidrug-resistant infections, exemplified in K. pneumoniae bacteremia (Hafiz et al., 2023), emphasizes the need for comprehensive interventions beyond individual patient care. The authors’ assessment of K. pneumoniae bacteremia aligns with broader literature emphasizing the community-level impact of multidrug-resistant infections. A study by Nordmann et al. (2009) further emphasizes the wider societal implications, urging a comprehensive response to curb the spread of resistance. Gordon et al.'s (2019) study on S. aureus bacteremia aligns with research by Quezada et al. (2013) emphasizing the long-term mortality associated with MRSA in healthcare-associated cases. The study by Dargahi et al. (2022) on biofilm formation aligns with a survey by Fadl (2018), highlighting the prevalence of biofilm-producing GPB and identifying effective antibiotics against resistant isolates. Akhavizadegan et al. (2021) study on antibiotic resistance in uropathogens aligns with a study by Kot (2019), indicating higher resistance rates in inpatient samples and emphasizing the importance of tailored treatment strategies. Findings by Araj et al. (2020) on C/T align with Giacobbe et al. (2018), suggesting its potential as an alternative treatment with minimized toxicity and bacterial resistance.
Fig. 2. Traffic lights plot of the risk of bias assessment.
Fig. 3. Risk of bias summary plot. Mostafavi et al. (2021) study on community-acquired urinary tract infections aligns with a study by Kallen et al. (2006), emphasizing the importance of tailored empirical therapy. The identification of E. coli as the predominant pathogen and the effectiveness of imipenem, meropenem, and amikacin in severe cases aligns with global trends outlined by Giamarellos-Bourboulis et al. (1997). Hammour et al.'s (2023) study on carbapenem-resistant bacteria echoes the global concern highlighted by Gupta et al. (2011). The socio-economic, cultural, and healthcare system dynamics specific to the Middle East may play pivotal roles in shaping observed resistance trends. Understanding these variation factors becomes paramount as we seek to develop effective interventions tailored to the unique challenges presented by the region. Adopting a One Health perspective is critical in addressing the multifaceted challenge of AMR in the Middle East. When analyzing the observed resistance patterns, human, animal, and environmental health interconnectedness becomes evident. Integrating efforts across these domains will be essential for developing comprehensive and sustainable strategies to mitigate resistance effectively. Recognizing the interplay between different health sectors emphasizes the need for collaborative, cross-disciplinary approaches to combat the growing threat of resistance. ConclusionThis study explores AMR in the Middle East from a One Health perspective. The synthesis of findings paints a vivid picture of resistance challenges across diverse clinical settings. Resistance prevalence in critical care units underscores the need for tailored treatment in intensive care. The emergence of colistin resistance and diverse strains underscores the urgency in understanding and addressing resistance mechanisms. Temocillin's potential and alternative interventions highlight the need to explore strategies against common infections. Pediatric resistance trends emphasize the need for targeted interventions. The prevalence of carbapenem-resistant bacteria and the impact of multidrug-resistant infections underscore the urgent need for coordinated efforts. The association of MRSAwith increased long-term mortality and biofilm-producing bacteria prevalence adds complexity to managing infections. High colonization rates in detention centers highlight societal implications and the role of hygiene and infection control. Given these comprehensive findings, a coordinated, One Health approach is imperative to address the complex challenge of AMR in the Middle East. Conflict of interestThe author declares that there is no conflict of interest. FundingNot applicable. Data availabilityAll used data were presented in the manuscript. ReferenceAdisasmito, W.B., Almuhairi, S., Behravesh, C.B., Bilivogui, P., Bukachi, S.A., Casas, N. and Zhou, L. 2022. One Health: a new definition for a sustainable and healthy future. PLoS. Pathog. 18, e1010537. Akhavizadegan, H., Hosamirudsari, H., Pirroti, H. and Akbarpour, S. 2021. Antibiotic resistance: a comparison between inpatient and outpatient uropathogens. East. Mediterr. Health. J. 27, 124–130. Al Benwan, K. and Jamal, W. 2022. Etiology and antibiotic susceptibility patterns of urinary tract infections in children in a General Hospital in Kuwait: a 5-year retrospective study. Med. Princ. Pract. 31, 562–569. Albert, M.J., Bulach, D., Alfouzan, W., Izumiya, H., Carter, G., Alobaid, K., Alatar, F., Sheikh, A.R. and Poirel, L. 2019. Non-typhoidal Salmonella bloodstream infection in Kuwait: clinical and microbiological characteristics. PLoS. Negl. Trop. Dis. 13, e0007293. Almutawif, Y.A. and Eid, H.M.A. 2023. Prevalence and antimicrobial susceptibility pattern of bacterial uropathogens among adult patients in Madinah, Saudi Arabia. BMC. Infect. Dis. 23, 582. Al-Tawfiq, J.A., Rabaan, A.A., Saunar, J.V. and Bazzi, A.M. 2020. Antimicrobial resistance of gram-negative bacteria: a six-year longitudinal study in a hospital in Saudi Arabia. J. Infect. Public. Health. 13, 737–745. Alzahrani, K.J., Eed, E.M., Alsharif, K.F., Almehmadi, M.M., Alotaibi, S.F., Al-Ghamdi, F.A., Almuwalld, A.A., Alamri, S.H. and Saber, T. 2021. Prevalence of community-acquired methicillin-resistant Staphylococcus aureus in Taif social correctional center, Saudi Arabia. J. Infect. Dev. Ctries. 15, 1861–1867. Arafa, S.H., Alshehri, W.A., Organji, S.R., Elbanna, K., Obaid, N.A., Aldosari, M.S., Asiri, F.H., Ahmad, I. and Abulreesh, H.H. 2022. Antimicrobial resistance, virulence factor-encoding genes, and biofilm-forming ability of community-associated uropathogenic Escherichia coli in Western Saudi Arabia. Pol. J. Microbiol. 71, 325–339. Araj, G.F., Berjawi, D.M., Musharrafieh, U. and El Beayni, N.K. 2020. The activity of ceftolozane/tazobactam against commonly encountered antimicrobial-resistant Gram-negative bacteria in Lebanon. J. Infect. Dev. Ctries. 14(6), 559–564. Armijo-Olivo, S., Stiles, C.R., Hagen, N.A., Biondo, P.D. and Cummings, G.G. 2012. Assessment of study quality for systematic reviews: a comparison of the cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J. Eval. Clin. Pract. 18, 12–18. Dargahi, Z., Hamad, A.A., Sheikh, A.F., Ahmad Khosravi, N., Samei, F.S., Motahar, M., Mehr, F.J., Abbasi, F., Meghdadi, H., Bakhtiyariniya, P., Heydari, R., Moradi, M. and Asareh Zadegan, D. A. 2022. The biofilm formation and antibiotic resistance of bacterial profile from endotracheal tube of patients admitted to intensive care unit in southwest Iran. PLoS One 17, e0277329. Fadl, A.E.W. 2018. Antibacterial and antibiofilm effects of bee venom from (Apis mellifera) on multidrug-resistant bacteria (MDRB). Al-Azhar J. Pharm. Sci. 58, 60–80. Giacobbe, D.R., Bassetti, M., De Rosa, F.G., Del Bono, V., Grossi, P.A., Menichetti, F. and ISGRI-SITA (Italian Study Group on Resistant Infections of the Società Italiana Terapia Antinfettiva). 2018. Ceftolozane/tazobactam: place in therapy. Exp. Rev. Anti-infect. Ther. 16, 307–320. Giamarellos-Bourboulis, E.J., Grecka, P. and Giamarellou, H. 1997. Comparative in vitro interactions of ceftazidime, meropenem, and imipenem with amikacin on multiresistant Pseudomonas aeruginosa. Diag. Microbiol. Infect. Dis. 29, 81–86. Gordon, O., Cohen, M.J., Gross, I., Amit, S., Averbuch, D., Engelhard, D., Milstone, A.M. and Moses, A.E. 2019. Staphylococcus aureus bacteremia in children: antibiotic resistance and mortality. Pediatr. Infect. Dis. J. 38, 459–463. Gupta, N., Limbago, B.M., Patel, J.B. and Kallen, A.J. 2011. Carbapenem-resistant Enterobacteriaceae: epidemiology and prevention. Clin. Infect. Dis. 53, 60–67. Hafiz, T.A., Alanazi, S., Alghamdi, S.S., Mubaraki, M.A., Aljabr, W., Madkhali, N., Alharbi, S.R., Binkhamis, K. and Alotaibi, F. 2023. Klebsiella pneumoniae bacteraemia epidemiology: resistance profiles and clinical outcome of King Fahad Medical City isolates, Riyadh, Saudi Arabia. BMC. Infect. Dis. 23, 579. Hammour, K.A., Abu-Farha, R., Itani, R., Karout, S., Allan, A., Manaseer, Q. and Hammour, W.A. 2023. The prevalence of carbapenem resistance Gram-negative pathogens in a Tertiary Teaching Hospital in Jordan. BMC. Infect. Dis. 23, 634. Islam, M.M., Farag, E., Hassan, M.M., Enan, K.A., Mohammad Sabeel, K.V., Alhaddad, M.M., Smatti, M.K., Al-Marri, A.M., Al-Zeyara, A.A., Al-Romaihi, H., Yassine, H.M., Sultan, A.A., Bansal, D. and Mkhize-Kwitshana, Z. 2022. Diversity of bacterial pathogens and their antimicrobial resistance profile among commensal rodents in Qatar. Vet. Res. Commun. 46, 487–498. Kabrah, A. 2022. Extended-spectrum beta-lactamase and carbapenem-resistant Gram-negative pathogens in Makkah, Saudi Arabia. Ethiop. J. Health. Sci. 32, 1221–1230. Kallen, A.J., Welch, H.G. and Sirovich, B.E. 2006. Current antibiotic therapy for isolated urinary tract infections in women. Arch. Int. Med. 166, 635–639. Kot, B. 2019. Antibiotic resistance among uropathogenic. Polish. J. Microbiol. 68, 403–415. Lillie, P.J., Johnson, G., Ivan, M., Barlow, G.D. and Moss, P.J. 2019. Escherichia coli bloodstream infection outcomes and preventability: a six-month prospective observational study. J. Hosp. Infect. 103, 128–133. Merhi, G., Amayri, S., Bitar, I., Araj, G.F. and Tokajian, S. 2023. Whole genome-based characterization of multidrug resistant Enterobacter and Klebsiella aerogenes isolates from Lebanon. Microbiol. Spectr. 11, e0291722. Mostafavi, S.N., Rostami, S., Rezaee Nejad, Y., Ataei, B., Mobasherizadeh, S., Cheraghi, A., Haghighipour, S., Nouri, S., Pourdad, A., Ataabadi, P., Almasi, N., Heidary, L., Naderi, K. and Kelishadi, R. 2021. Antimicrobial resistance in hospitalized patients with community-acquired urinary tract infection in Isfahan, Iran. Arch. Iran. Med. 24, 187–192. Nawfal Dagher, T., Al-Bayssari, C., Chabou, S., Baron, S., Hadjadj, L., Diene, S.M., Azar, E. and Rolain, J.M. 2020. Intestinal carriage of colistin-resistant Enterobacteriaceae at Saint Georges Hospital in Lebanon. J. Glob. Antimicrob. Resist. 21, 386–390. Nordmann, P., Cuzon, G. and Naas, T. 2009. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet. Infect. Dis. 9, 228–236. Page, M.J., McKenzie, J.E., Bossuyt, P.M., Boutron, I., Hoffmann, T.C. and Mulrow, C.D. 2021. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, 71. Qasemi, A., Rahimi, F. and Katouli, M. 2022. Clonal groups of extended-spectrum β-lactamase and biofilm-producing uropathogenic Escherichia coli in Iran. Pathog. Glob. Health. 116, 485–497. Quezada Joaquin, N.M., Diekema, D.J., Perencevich, E.N., Bailey, G., Winokur, P.L. and Schweizer, M.L. 2013. Long-term risk for readmission, methicillin-resistant Staphylococcus aureus (MRSA) infection, and death among MRSA-colonized veterans. Antimicrob. Agents. Chemother. 57, 1169–1172. Rahbar, M., Van de Velde, S., Eslami, P. and Mardani, M. 2020. Activity of temocillin and comparators against urinary Escherichia coli and Klebsiella pneumoniae from Iran. Eur. J. Clin. Microbiol. Infect. Dis. 39, 1793–1796. Rahimzadeh, M., Shahbazi, S., Sabzi, S., Habibi, M. and Asadi Karam, M.R. 2023. Antibiotic resistance and genetic diversity among Pseudomonas aeruginosa isolated from urinary tract infections in Iran. Future. Microbiol. 18, 1171–1183. Sahib Abdul-Mohammed, H., Kamal, M.A. and Mohsen, A.Z. 2022. Imipenem resistance in Gram-negative bacteria in the Central Pediatric Teaching Hospital in Baghdad, Iraq. Arch. Razi. Inst. 77, 123–128. Schwabe, C.W. 1964. Veterinary medicine and human health. Baltimore, MD: The Williams &Wilkins Company. Sheikh, R.Y., Murdeshwar, S., Maheshwari, T.K. and Chacko, S. 2022. Microbiological spectrum and antibiogram of urinary tract infection in a Tertiary Care Center from the Kingdom of Bahrain. Saudi. J. Kidney. Dis. Transpl. 33, S53–S60. Sterne, J.A.C., Savović, J., Page, M.J., Elbers, R.G., Blencowe, N.S. and Boutron, I. 2019. RoB 2: a revised tool for assessing the risk of bias in randomized trials. BMJ 366, l4898. Tadesse, B.T., Ashley, E.A., Ongarello, S., Havumaki, J., Wijegoonewardena, M., González, I.J. and Dittrich, S., 2017. Antimicrobial resistance in Africa: a systematic review. BMC. Infect. Dis. 17, 1–17. | ||
| How to Cite this Article |
| Pubmed Style Alkheraije KA, . Antimicrobial resistance from one health perspective in the Middle East: A systematic review. Open Vet J. 2024; 14((1) (Zagazig Veterinary Conference)): 577-585. doi:10.5455/OVJ.2024.v14.i1.53 Web Style Alkheraije KA, . Antimicrobial resistance from one health perspective in the Middle East: A systematic review. https://www.openveterinaryjournal.com/?mno=188605 [Access: May 09, 2024]. doi:10.5455/OVJ.2024.v14.i1.53 AMA (American Medical Association) Style Alkheraije KA, . Antimicrobial resistance from one health perspective in the Middle East: A systematic review. Open Vet J. 2024; 14((1) (Zagazig Veterinary Conference)): 577-585. doi:10.5455/OVJ.2024.v14.i1.53 Vancouver/ICMJE Style Alkheraije KA, . Antimicrobial resistance from one health perspective in the Middle East: A systematic review. Open Vet J. (2024), [cited May 09, 2024]; 14((1) (Zagazig Veterinary Conference)): 577-585. doi:10.5455/OVJ.2024.v14.i1.53 Harvard Style Alkheraije, K. A. & (2024) Antimicrobial resistance from one health perspective in the Middle East: A systematic review. Open Vet J, 14 ((1) (Zagazig Veterinary Conference)), 577-585. doi:10.5455/OVJ.2024.v14.i1.53 Turabian Style Alkheraije, Khalid A., and . 2024. Antimicrobial resistance from one health perspective in the Middle East: A systematic review. Open Veterinary Journal, 14 ((1) (Zagazig Veterinary Conference)), 577-585. doi:10.5455/OVJ.2024.v14.i1.53 Chicago Style Alkheraije, Khalid A., and . "Antimicrobial resistance from one health perspective in the Middle East: A systematic review." Open Veterinary Journal 14 (2024), 577-585. doi:10.5455/OVJ.2024.v14.i1.53 MLA (The Modern Language Association) Style Alkheraije, Khalid A., and . "Antimicrobial resistance from one health perspective in the Middle East: A systematic review." Open Veterinary Journal 14.(1) (Zagazig Veterinary Conference) (2024), 577-585. Print. doi:10.5455/OVJ.2024.v14.i1.53 APA (American Psychological Association) Style Alkheraije, K. A. & (2024) Antimicrobial resistance from one health perspective in the Middle East: A systematic review. Open Veterinary Journal, 14 ((1) (Zagazig Veterinary Conference)), 577-585. doi:10.5455/OVJ.2024.v14.i1.53 |