| Original Article | ||
Open Vet. J.. 2020; 10(3): 340-346 doi: 10.4314/ovj.v10i3.13 Open Veterinary Journal, (2020), Vol. 10(3): 340–346 Original Research http://dx.doi.org/10.4314/ovj.v10i3.13 Feline aortic thromboembolism: Presentation, diagnosis, and treatment outcomes of 15 catsMarwa H. Hassan, Ashraf M. Abu-Seida*, Faisal A. Torad and Elham A. HassanDepartment of Surgery, Anesthesiology and Radiology, Faculty of Veterinary Medicine, Cairo University, Giza, Egypt *Corresponding Author: Ashraf M. Abu-Seida. Department of Surgery, Anesthesiology & Radiology, Faculty of Veterinary Medicine, Cairo University, Giza, Egypt. Email: ashrafseida [at] cu.edu.eg Submitted: 28/06/2020 Accepted: 18/09/2020 Published: 29/09/2020 © 2020 Open Veterinary Journal
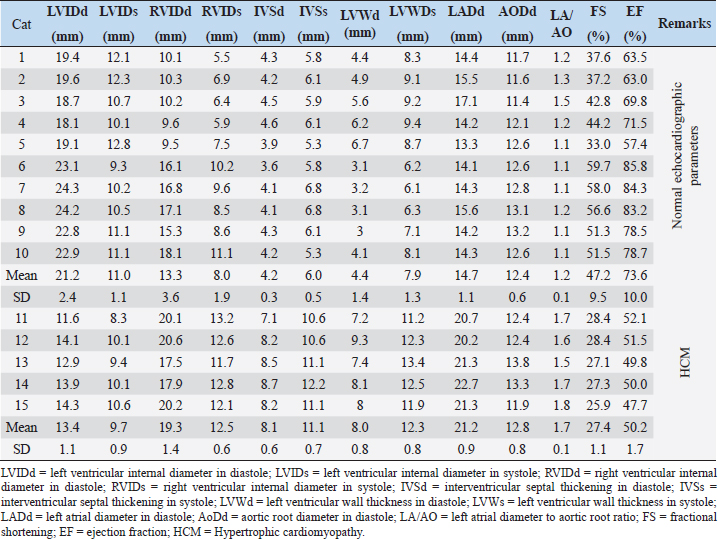
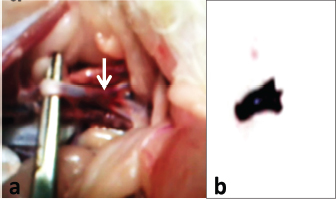
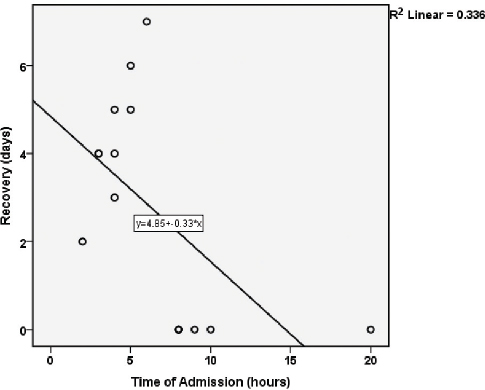
AbstractBackground: Feline aortic thromboembolism (FATE) is a fatal disease where a blood clot gets lodged into the aortic trifurcation. Aim: This study describes the diagnosis and treatment outcome of FATE in 15 clinical cases. Methods: Fifteen cats with a sudden onset of hind limb paresis/paralysis, vocalization, and pain were admitted to the surgery clinic. A full case history was obtained and clinical, orthopedic, neurologic, radiographic, electrocardiographic, and echocardiographic examinations were performed for each cat. The treatment protocol included daily administration of multiple anticoagulant drugs with different mode of actions and meloxicam for 7 successive days. Prophylactic anticoagulant therapy (clopidogrel and acetylsalicylic acid) was continued for 6 months. All data were statistically analyzed and the correlation between time of admission and treatment outcome was tested using Pearson’s correlation coefficient. Results: The case history and clinical, orthopedic, and neurologic examinations revealed a sudden onset of hind limb paralysis (n=12) or paresis (n=3) associated with vocalization and pain, absence of trauma, cold and pale paws of hind limbs (n=13, 86.7%) or cyanosed hind paws (n=2, 13.3%), absence of femoral pulsation, shallow and rapid open-mouth respiration (61 ± 8 breaths/minutes), hypothermia (37.9°C ± 0.6°C) and tachycardia (155 ± 12 beats/minutes), with a muffled heart sound in four cats (26.7%). Radiography revealed no abnormalities in the hind limbs, pelvis, and spines, cardiomegaly in five cats (33.3%), mild pleural effusion and vascular pattern of the lung in six cats (40%), and Valentine’s heart shape in four cats (26.7%). Electrocardiography (ECG) revealed an R-wave< 0.9 mV, prolongation of QRS interval in five cats (33.3%), and conduction disturbance in four cats (26.7%). Echocardiography was consistent with hypertrophic cardiomyopathy (HCM) in five cats (33.3%). A statistically significant (p =0.023) strong negative correlation (r =−0.6) was reported between time of admission and subsequent early treatment and recovery from clinical signs. The treatment was successful in nine cats (60%), while four cats (26.7) were euthanized and two cats (13.3%) were subjected to hind limb amputation, at the owners’ requests. Conclusion: Clinical signs, radiography, ECG, and echocardiography are valuable for diagnosis of FATE. The outcome of the multiple anticoagulants therapy depends mainly upon early diagnosis and treatment within the first 6 hours from the onset of clinical signs. Keywords: Anticoagulant, Aortic thromboembolism, Cardiomyopathy, Echocardiography, Paralysis. IntroductionFeline aortic thromboembolism (FATE) or saddle thrombus is a catastrophic lesion where a blood clot gets embolised and lodged into the aortic trifurcation (Borgeat et al., 2014). It is a fatal disease that may progress very quickly as a cat can go from being healthy to be in severe distress within few minutes (Brent et al., 2006). FATE is mostly reported in male cats with no breed predisposition (Chuang et al., 2001; Ferasin, 2009). The exact etiology of FATE is unknown. It may occur as a complication of feline hypertrophic cardiomyopathy (HCM). Approximately 12%–21% of cats with HCM may develop FATE (Fox, 1999; Hogan et al., 1999; Fuentes, 2012). Other diseases associated with FATE may include pulmonary neoplasia and thyroid disease (Laste and Harpster, 1995; Ladurner et al., 2005; Mackman, 2008). The potential pathogenesis of FATE is thought to be started by cardiac disease that causes abnormal blood turbulence, leading to agitation of blood and consequently micro-clot formation in the left atrium. These micro-clots grow into large clots and either the whole blood clot or part of it can be ejected from the heart and lodged in the aortic trifurcation (Pion and Kittleson, 2008; Nakamura et al., 2017). The typical symptoms of FATE are acute onset of severe pain, vocalization, pulselessness, pallor, unilateral or bilateral hind limbs paralysis, poikilothermy, and sometimes dyspnea or tachypnea (Laste and Harpster, 1995; Fox, 1999; Chuang et al., 2001). The survival rates of cats with unilateral occlusion (70%–93%) are better than that with bilateral occlusion (15%–35%) (Ramsey et al., 1996; Pion and Kittleson, 2008). The targets of treatment of FATE are enhancement of thromboembolism dissolution, inhibition of the local thrombus, and prevention of embolization of the thrombi (Rush et al., 2002). Therefore, anticoagulants such as heparin and warfarin play a crucial role in the treatment of FATE with a success rate of 37%–39% (Schoeman, 1999; Smith et al., 2003). Exogenous thrombolytic agents such as streptokinase or tissue plasminogen activator may have a success rate of 0%–33% (Speakman et al., 1983). This study describes the diagnosis and treatment of FATE in 15 cats, with special reference to the correlation of time of admission and treatment outcome in a cohort of cats. Materials and MethodsAnimalsFifteen adult cats with a sudden onset of hind limb paresis/paralysis associated with pain and vocalization were admitted to the surgery clinic at the Department of Surgery, Anesthesiology and Radiology, Faculty of Veterinary Medicine, Cairo University, Egypt, between January 2017 and December 2019. The authors followed all institutional and international guidelines for animal care and use during this study. DiagnosisA complete case history was collected for all cats, including the exact time of onset of clinical signs, history of trauma, previous episodes or previous treatment, and presence or absence of systemic diseases. Clinical, orthopedic, and neurologic examinations were carried out in all cats. Radiography of the spines, pelvis, hind limbs, and thorax was carried out in all cats using an X-ray machine (Fisher, Germany). The radiographic setting factors were 45–50 kVp and 10 mA. Six limb leads electrocardiography (ECG) was recorded for each cat using a single channel ECG machine (Yasen, ECG 901A, China). All cats were gently restrained in a right lateral recumbency with the limbs positioned in a perpendicular position to the longitudinal axis of the body. Self-adhesive patch electrodes were attached to the palmar and plantar aspects of the fore limb and hind limb paws, respectively. The six standard limb leads I, II, III, aVR, aVL, and aVF were recorded at paper settings of 10 mm/mV and 50 mm/seconds with filter band settings of 0.05–150 Hz. Echocardiography was carried out after hair shaving and application of ultrasound coupling gel. Right parasternal views (long and short axis) were performed using a 5–9 MHz microconvex probe attached to ultrasound machine (EDAN-DUS 60, China) TreatmentThe treatment protocols included the administration of Heparin sodium (Heparin®, CID Co., Egypt) at a dose of 300 IU/kg given SC twice daily, Clexane (Enoxaparin®, 2,000 IU/0.2 ml, Aventis Pharm, Egypt) at a dose of 1 mg/kg given SC q12h, and Cerebrolysin (Cerebrolysin®, EVA Pharma, Egypt) at a dose of 2 mg /kg given IM once daily for 6 successive days. Acetylsalicylic acid (Baby Aspirin, 81 mg tab®, Nile Co., Egypt) was also given orally at a dosage of 10 mg/kg q36h. The cats were also given Meloxicam (Meloxicam®, Amirya Co., Alexandria, Egypt) at a dose of 0.1 mg/kg given SC once daily. Physiotherapy including hind limbs massage and gentle passive movement was advised for 30 minutes three times daily for 1 week. One week following admission, a prophylactic anticoagulant oral therapy, including Clopidogrel (Thrombo® 18.75 mg, EPICO, Egypt) was given at a dosage of 2–3 mg/kg once daily and acetylsalicylic acid once q36h for 6 months. Cats with HCM were put under conservative medicinal therapy to control signs of cardiac failure, including once daily oral administrations of Digoxin (Lanoxin®, GlaxoSmithKline, Egypt) at a dose of 0.01 mg/kg q48h, Furosemide (Lasix®, Alexandria Co., Egypt) at a dose of 1 mg/kg, and Enalapril (Ezapril®, Multi Pharma; Egypt) at a dose of 0.25 mg/kg whenever needed. All cats were treated on outpatient basis. The cat was considered as survived when they recovered and the functioning of their hind limbs returned. The cats unresponsive to treatment were either euthanized or underwent hind limb amputation according to their owners, requests. Autopsy of the euthanized cats was carried out to confirm the diagnosis. Statistical analysisAll data were collected and presented as mean ± standard deviation. Response of cats following medicinal therapy in relation to the time of admission was recorded for each cat. The correlation between time of admission and treatment outcome was tested using Pearson’s correlation coefficient. The r ≥ 0.5 was considered as strongly correlated and r < 0.5 was poorly correlated. Data were considered statistically significant when p < 0.05. The analysis of data was carried out by the Statistical Package for the Social Sciences (SPSS) software 21 (IMP SPSS Inc, Chicago, IL). Ethical approvalAll international and institutional guidelines for animal use and care were followed. ResultsBased on clinical, orthopedic, neurologic, radiographic, electrocardiographic, and echocardiographic examinations, aortic thromboembolism was diagnosed in all cats. HCM was confirmed in 5 out of 15 cats and no other systemic diseases were reported. The diseased animals included six Persian, five Siamese, and four domestic shorthair cats. These cats were of different ages (4.3 ± 2.1 years), both sexes (10 male and 5 female), and different weights (3.4 ± 0.8 kg). The cats were admitted with sudden hind limb paralysis (n=12, 80%) or paresis (n=3, 20%). The diseased cats exhibited either bilateral (n=11, 73.3%) or unilateral (n=4, 26.7%) aortic thromboembolism. In bilateral aortic thromboembolism, both hind limbs were equally affected without involvement of the forelimbs. All cats had controlled urination. Cold and pale paws of both hind limbs were reported in 13 cats (86.7%), while 2 cats (13.3 %) had cyanosed hind paws. The absence of femoral pulsation was recorded in all affected limbs. Shallow and rapid open-mouth respiration (61 ± 8 breaths/minutes) was recorded in 13 cats (86.7%), while normal respiration was seen in 2 cats (13.3%). Rectal temperature was slightly reduced (37.9°C ± 0.6°C) in all cats. Thoracic auscultation revealed tachycardia (155 ± 12 beats/minutes) with muffled heart sound in 4 cats (26.7%). Nine cats (60%) were presented within the first 6 hours after the onset of clinical signs, five cats (33.3 %) were presented within 6–24 hours and one cat (6.7%) was admitted 1 week following the onset of signs. Out of the nine cats presented within the first 6 hours after the onset of clinical signs, five cats (33.3%) had 6 months to 1-year history of HCM. No other systemic disease was reported in any of the examined cats. Cats admitted within the first 6 hours from the onset of clinical signs showed dragging of both hind limbs while walking. The response to painful stimuli such as skin pricks or forceps clamping was very sluggish or almost absent along the hind limbs, starting from the paws till the level of hip joints. In cats admitted within 6–24 hours from the onset of the episode, the hind limbs were relaxed with no response to pain elicited by forceps clamping. In one cat that was admitted after 1 week from episode, the mucous membranes were pale with delayed capillary refilling time (>3 seconds) and the hind limbs were atrophied and the paws were cyanotic. Upon radiographic examination of the hind limbs, pelvis, and spines, no abnormalities were detected within the musculoskeletal system. Lateral thoracic radiography revealed cardiomegaly in five cats (33.3%) and mild pleural effusion and vascular pattern of the lung in six cats (40%). Ventrodorsal thoracic radiographs revealed a characteristic Valentine’s heart shape in four cats (26.7%) (Fig. 1). ECG revealed an R-wave< 0.9 mV with prolongation of QRS interval in five cats (33.3%) and conduction disturbance (third-degree atrio-ventricular block) in four cats (26.7%). Echocardiographic examination was consistent with HCM in five cats (33.3%) and normal in 10 cats (66.7%), as shown in Table 1. Combined anticoagulant therapy of the cats admitted within 6 hours from the onset of clinical signs (n=9, 60%) resulted in mild improvement in the function of their hind limbs and improved response to painful stimuli within the first 3 days. The cats completely regained the function of their hind limbs within 1 week. No thromboembolic event was noted in all survived cats during a 6-months follow-up. Anticoagulant therapy for 7 days could not improve the cats admitted within 6–24 hours or after 1 week of the episode (n=6, 40%). These cats were either euthanized (n=4, 26.7%) or underwent hind limb amputation (n=2, 13.3%), according to their owners’ request. At the owners’ requests, four cats (26.7%) with bilateral aortic thromboembolism and unresponsive to treatment were euthanized. Autopsy of the euthanized cat confirmed the presence of blood clot completely occluding the terminal aorta at the level of aortic trifurcation (Fig. 2), while two cats (13.3%) with unilateral aortic thromboembolism and unresponsive to treatment were subjected to hind limb amputation, at the owners’ requests (Fig. 3). A statistically significant (p =0.023) strong negative correlation (r =−0.6) was reported between time of admission and subsequent early treatment and recovery from the clinical signs (Fig. 4).
Fig. 1. An 8-year-old Siamese cat with FATE and HCM: Ventrodorsal thoracic radiograph showing severe cardiomegaly and a characteristic Valentine’s heart shape. DiscussionFATE is a very serious disease which is life threatening and there is great interest and value of time from presentation to survival. In the present study, early admission and intervention of cats with FATE were very crucial for successful treatment outcomes. The first 6 hours from the onset of the episode are very critical for survival. Table 1. Detailed echocardiographic findings of 15 cats diagnosed with FATE.
Fig. 2. FATE in a 4-year-old Persian cat: (a) Post-mortem examination of a cat with FATE showing a blood clot lodged in the aortic trifurcation. (b) The removed blood clot showing trifurcations. With regard to the etiology of FATE, it may be a complication of HCM. In the present study, 30% of cats with FATE had HCM. This is in agreement with previous studies that recorded FATE in 12%–21% of cats with HCM (Fox, 1999; Hogan et al., 1999; Fuentes, 2012). In this study, the male cats were more commonly affected with FATE than females. Also, three breeds of cats were recorded in this study with no breed predisposition. Similar findings were reported by earlier studies (Chuang et al., 2001; Ferasin, 2009). The characteristic sudden clinical signs associated with FATE should be considered in differentiating FATE from other orthopedic conditions. The cold and pale paws as well as weak or absence of femoral pulsation are characteristic clinical signs associated with FATE. Also, a controlled urination is helpful in exclusion of spinal neurological injuries. All of the clinical symptoms could be attributed to the lodgment of a blood clot into the aortic trifurcation and stoppage of arterial supply and damage of the affected hind limbs. Thoracic radiographs of five cats with FATE revealed characteristic changes in the cardiac size and shape. Similar findings were previously recorded, particularly in the late stages of HCM (Trehiou-Sechi et al., 2012). Therefore, the authors recommend thoracic radiography during diagnosis of FATE. Also, it was noted that the cats with HCM were admitted within 6 hours from the onset of clinical signs because the owners had increased knowledge about what signs and risk to watch for.
Fig. 3. A 3-year-old Persian cat with unilateral aortic thromboembolism showing unilateral hind limb gangrene.
Fig. 4. The correlation between time of admission and treatment outcome of cats with FATE: Scatter plot demonstrating the correlation between time of admission and subsequent early treatment (h) of cats with aortic thromboembolism and recovery from clinical signs (days) (r=−o.6; p=0.023; y=4.85+−0.33*x). The electrocardiographic findings, including tall R-wave, prolonged QRS interval, and third-degree atrio-ventricular block, indicated feline HCM (Moore et al., 2007). In previous studies, echocardiographic diagnosis of HCM in 10 cats favored the correlation between HCM and FATE (Pion and Kittleson, 2008; Nakamura et al., 2017). Similarly, HCM was recorded in 30% of cats with FATE studied here. Although surgical embolectomy appears to be the most logical therapeutic approach in managing thromboembolism, it was a difficult option in cats with FATE due to the small-sized blood vessels and the anesthetic risk encountered in cardiac patients (Brent et al., 2006). Massive administration of anticoagulant drugs as quickly as possible was crucial in preventing the irreversible damage of the limbs. Heparin was mainly used for the prevention of extension of the existing thrombus and prevention of further clot formation. Heparin does not breakdown the already formed blood clots, but it enhances the normal body’s natural thrombolytic mechanisms (Uppe et al., 2013). Clexane is a low molecular weight heparin used for treatment and prevention of deep vein thrombosis. It binds to and accelerates the anti-thrombin III (Van De Wiele et al., 2010). In addition, cerebrolysin is a natural neuropeptide having several neurotrophic effects, such as stimulation of new neuron growth, maintenance of neuron, and slows down the neural damage (Whigham et al., 1998). Early (within first 6 hours) and massive administration of anticoagulant drugs with different mode of actions resulted in rapid improvement in clinical signs and lysis of the small, recently formed, thrombus before being organized. On the other hand, delayed treatment (after 6 hours) resulted in poor prognosis. This poor prognosis may be attributed to the lodgment and adhesion of the organized thrombus within the blood vessel, as well as the ischemia and irreversible damage of the hind limbs. Like many studies, the main limitation of this study is the small population of 15 cats. Therefore, we could not study the exact effect of the age, sex, and breed of the cats studied on the survival rate. ConclusionClinical signs, radiography, ECG, and echocardiography are valuable for diagnosis of FATE. Time of admission has a detrimental influence on the survival of cats with FATE. Early admission, diagnosis, and treatment with multiple anticoagulant drugs within the first 6 hours from the onset of clinical signs have a favorable survival rate of cats with FATE. Conflict of interestThe authors declare no conflict of interests Authors’ contributionsAll authors were involved in the diagnosis and treatment of the cases. All authors prepared the manuscript and approved the final version of the manuscript. ReferencesBorgeat, K., Wright, J., Garrod, O., Payne, J.R. and Fuentes, V.L. 2014. Arterial thromboembolism in 250 cats in general practice: 2004–2012. J. Vet. Int. Med. 28, 102–108. Brent, R.S., Kittleson, M.D. and Kyles, A.E. 2006. Use of rheolytic thrombectomy in the treatment of feline distal aortic thromboembolism. J. Vet. Int. Med. 20, 290–296. Chuang, Y.J., Swanson, R., Raja, S.M. and Olson, S.T. 2001. Heparin enhances the specificity of antithrombin for thrombin and factor Xa independent of the reactive center loop sequence. Evidence for an exosite determinant of factor Xa specificity in heparin-activated antithrombin. J. Biol. Chem. 18, 14961–14971. Ferasin, L. 2009. Feline myocardial disease.classification, Pathophysiology and clinical presentation. J. Fel. Med. Surg. 11, 3–13. Fox, P.R. 1999. Feline cardiomyopathies. In Textbook of canine and feline cardiology. Eds., Sisson, D. and Moise, N.S. Philadelphia, PA: WB Saunders, pp: 621–678. Fuentes, V.L. 2012. Arterial thromboembolism risks, realities and a rational first-line approach. J. Fel. Med. Surg. 14, 459–470. Hogan, D.F., Dhaliwal, R.S., Sisson, D.D. and Kitchell, B.E. 1999. Paraneoplastic thrombocytosis-induced systemic thromboembolism in a cat. J. Am. Anim. Hosp. Assoc. 6, 483–486. Ladurner, G., Kalvach, P. and Moessler, H. 2005. Neuroprotective treatment with cerebrolysin in patients with acute stroke: a randomised controlled trial. J. Neural. Transm. 112, 415–428. Laste, N.J. and Harpster, K. 1995. A retrospective study of 100 cases of feline distal aortic thromboembolism: 1977–1993. J. Am. Anim. Hosp. Assoc. 31, 492–500. Mackman, N. 2008. Triggers, targets and treatments for thrombosis. Nature 7181, 914–918. Moore, K.E., Morris, N., Dhupa, N., Murtaugh, R.J. and Rush, J.E. 2007. Retrospective study of streptokinase administration in 46 cats with arterial thromboembolism. J. Vet. Emerg. Crit. Care 10, 245–257. Nakamura, M., Yamada, N. and Ito, M. 2017. Novel anticoagulant therapy of venous thromboembolism: Current status and future directions. Ann. Vasc. Dis. 2, 92–98. Pion, P.D. and Kittleson, M.D. 2008. Therapy for feline aortic thromboembolism. In Kirk’s current veterinary therapy. Ed., Kirk, R.W. Philadelphia, PA: WB Saunders, pp: 295–302. Ramsey, C.C., Riepe, R.D., Macintire, D.K. and Burney, D.P. Streptokinase a practical clot buster? Proceeding of the 5th International Veterinary Emergency and Critical Care Symposium; San Antonio, TX, 1996, pp 225–228. Rush, J.E., Freeman, L., Fenollosa, N.K. and Brown, D.J. 2002. Population and survival characteristics of cats with hypertrophic cardiomyopathy: 260 cases (1990–1999). J. Am. Vet. Med. Assoc. 2, 202–207. Schoeman, J.P. 1999. Feline distal aortic thromboembolism: a review of 44 cases (1990–1998). J. Fel. Med. Surg. 1, 221–231. Smith, S.A., Tobias, A.H., Jacob, K.A., Fine, D.M. and Grumbles, P.L. 2003. Arterial thromboembolism in cats: Acute crisis in 127 cases (1992–2001) and longtermmanagement with low-dose aspirin in 24 cases. J. Vet. Intern. Med. 17, 73–83. Speakman, C., Pechman, R.D., and D’Andrea, G.H. 1983. Aorticthrombosis and unilateral hydronephrosis associated with leiomyosarcoma in a cat. J. Am. Vet. Med. Assoc. 182, 62–63. Trehiou-Sechi, E., Tissier, R., Gouni, V., Misbach, C., Petit, A.M., Balouka, D., Sampedrano, C.C., Castaignet, M., Pouchelon, J.L. and Chetboul, V. 2012. Comparative echocardio- graphic and clinical features of hypertrophic cardiomyopathy in 5 breeds of cats: a retrospective analysis of 344 cases (2001-2011). J. Vet. Intern. Med. 26, 532–541. Uppe, P., Jeyaraja, K. and Sumathi, D. 2013. Dilated cardiomyopathy in cats—a case report. Vet. World 4, 226–227.Van De Wiele, C.M., Hogan, D.F., Green, H.W. and Sederquist, K.D. 2010. Antithrombotic effect of enoxaparin in clinically healthy cats: a venous stasis model. J. Vet. Intern. Med. 24, 185–191. Whigham, H.M., Ellison, G.W. and Graham, J. 1998. Aortic foreign body resulting in ischemic neuromyopathy and development of collateral circulation in a cat. J. Am. Vet. Med. Assoc. 6, 829–832. | ||
| How to Cite this Article |
| Pubmed Style Hassan MH, Abu-seida AM, Torad FA, Hassan EA. Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats. Open Vet. J.. 2020; 10(3): 340-346. doi:10.4314/ovj.v10i3.13 Web Style Hassan MH, Abu-seida AM, Torad FA, Hassan EA. Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats. https://www.openveterinaryjournal.com/?mno=119846 [Access: January 25, 2026]. doi:10.4314/ovj.v10i3.13 AMA (American Medical Association) Style Hassan MH, Abu-seida AM, Torad FA, Hassan EA. Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats. Open Vet. J.. 2020; 10(3): 340-346. doi:10.4314/ovj.v10i3.13 Vancouver/ICMJE Style Hassan MH, Abu-seida AM, Torad FA, Hassan EA. Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats. Open Vet. J.. (2020), [cited January 25, 2026]; 10(3): 340-346. doi:10.4314/ovj.v10i3.13 Harvard Style Hassan, M. H., Abu-seida, . A. M., Torad, . F. A. & Hassan, . E. A. (2020) Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats. Open Vet. J., 10 (3), 340-346. doi:10.4314/ovj.v10i3.13 Turabian Style Hassan, Marwa H., Ashraf M. Abu-seida, Faisal A. Torad, and Elham A. Hassan. 2020. Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats. Open Veterinary Journal, 10 (3), 340-346. doi:10.4314/ovj.v10i3.13 Chicago Style Hassan, Marwa H., Ashraf M. Abu-seida, Faisal A. Torad, and Elham A. Hassan. "Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats." Open Veterinary Journal 10 (2020), 340-346. doi:10.4314/ovj.v10i3.13 MLA (The Modern Language Association) Style Hassan, Marwa H., Ashraf M. Abu-seida, Faisal A. Torad, and Elham A. Hassan. "Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats." Open Veterinary Journal 10.3 (2020), 340-346. Print. doi:10.4314/ovj.v10i3.13 APA (American Psychological Association) Style Hassan, M. H., Abu-seida, . A. M., Torad, . F. A. & Hassan, . E. A. (2020) Feline aortic thromboembolism: Presentation, diagnosis and treatment outcomes of 15 cats. Open Veterinary Journal, 10 (3), 340-346. doi:10.4314/ovj.v10i3.13 |