| Research Article | ||
Open Vet. J.. 2024; 14(5): 1111-1116 Open Veterinary Journal, (2024), Vol. 14(5): 1111–1116 Research Article Jugular venous thrombosis as a risk factor for exercise-induced pulmonary hemorrhage in thoroughbred racehorsesTurke Shawaf*Department of Clinical Sciences, College of Veterinary Medicine, King Faisal University, Al-Ahsa, Saudi Arabia *Corresponding Author: Turke Shawaf. Department of Clinical Sciences, College of Veterinary Medicine, King Faisal University, Al-Ahsa, Saudi Arabia. Email: tshawaf [at] kfu.edu.sa Submitted: 01/01/2024 Accepted: 04/04/2024 Published: 31/05/2024 © 2024 Open Veterinary Journal
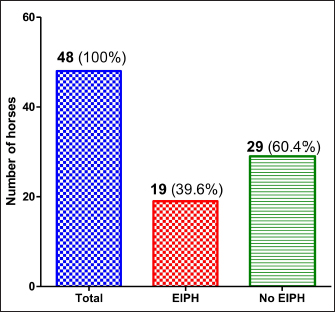
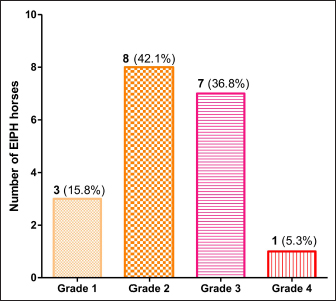
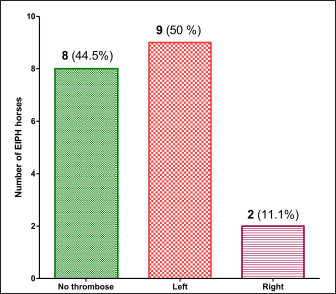
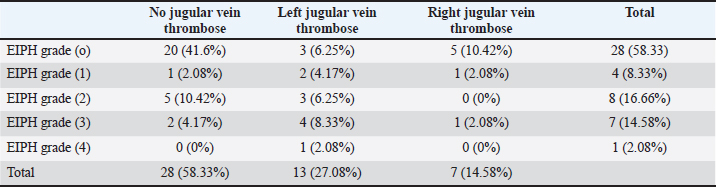
AbstractBackground: Exercise-induced pulmonary hemorrhage (EIPH) is one of the most commonly diagnosed disorders in racehorses. Many EIPH risk factors such as breed, age, high or low environmental temperature, and distance of the race have been studied in racehorses. Aim: The aim of this study was to study the relationship between EIPH and the presence of jugular vein thrombose in racehorses. Methods: Forty-eight thoroughbred racehorses randomly selected from animals with exercise intolerance due to respiratory disorders were enrolled in the present study. Clinical and tracheobronchoscopy examinations were done for EIPH grading. In addition, both jugular veins were examined using ultrasonography for vein thrombosis. Results: It was noted during endoscopy that many cases suffered from laryngeal paralysis, and we were not able to assess the degree of laryngeal paralysis under sedation. About 40% of horses with exercise intolerance suffered from EIPH of varying degrees. Most cases of jugular vein thrombosis were of the chronic type, as local heat and pain were not observed. About 42% of the exercise-intolerant horses had jugular vein thrombose with most jugular vein thrombosis on the left side. Combined jugular veins thrombose and EIPH were found in about 25% of exercise intolerance horses, while 17% showed jugular vein thrombose without EIPH, and 41% showed no EIPH with the absence of jugular vein thrombose. Conclusion: The present study revealed that jugular vein thrombosis may cause disorders-associated damage to the vessels and anatomical structures close to it, such as the trachea causing EIPH. Keywords: EIPH, Endoscopy, Jugular, Horse, Thrombosis. IntroductionExercise-induced pulmonary hemorrhage (EIPH) is one of the most commonly diagnosed disorders in Quarter Horses and Standardbreds (Tarancon et al., 2019; Bertram et al., 2023; Burns et al., 2023). EIPH is a substantial problem for the horse racing industry due to decreased performance, lost training days, necessity for pre-race medication, banning of horses from racing, occasional death, and public perception (Tarancon et al., 2019; Lo Feudo et al., 2021; Rocchigiani et al., 2022). It is known that EIPH occurs mainly as a result of the weakness of capillaries at the level of the pulmonary alveoli (Lo Feudo et al., 2022). In addition, increased pressure on the walls of these capillaries may result from the increase in natural blood pressure under stress and the increase in negative pressure within the thorax cavity during the race, causing a large difference in pressure and leading to capillaries rupture and bleeding (Sullivan and Hinchcliff, 2015; Poole and Erickson, 2016). Several factors such as breed, age, high or low environmental temperature, and distance of the race have been associated with an increased risk of EIPH (Gold et al., 2018; Crispe and Lester, 2019). A variety of causes and pathophysiologic mechanisms have been postulated for EIPH including intravascular pressures, extravascular pressures, and properties of the blood–gas barrier (Rocchigiani et al., 2022). Thoroughbreds breed exhibit a higher predisposition compared to other breeds (Burns et al., 2023; Vinardell et al., 2023). Other studied risk factors for EIPH include animal age (higher with increased age), gender (higher in male), high or low temperature, as well as yearly season (Birks et al., 2003; Hinchcliff et al., 2009). Additionally, distance of the race, accumulated years spent in race as well as ground hardness are considered as risk factors for EIPH (Takahashi et al., 2001). On the other side, some pathological predisposing factors for EIPH have also been identified, including inflammatory airway disease (IAD) (da Silva et al., 2017), equine asthma (Lo Feudo et al., 2021), and recurrent capillary stress in racehorses. One proposed explanation for the link between inflammation and EIPH suggests that inflammation leads to airway obstruction (da Silva et al., 2017; Lopez Sanchez et al., 2020). It has also been noted that some diseases associated with high blood pressure such as laryngeal paralysis or dorsal displacement of the soft palate or diseases that reduce the amount of air entering the respiratory tract under exercise may increase the risk for the development of EIPH (Poole and Erickson, 2016; Crispe and Lester, 2019). Intravenous administration of drugs and fluids in horses is often used in the treatment of different field conditions (Gardner et al., 1991; Dias and de Lacerda Neto, 2013). Thrombophlebitis most commonly affects the jugular veins in horses because they are the most commonly used site to access venous circulation. Jugular vein catheterizations and intravenous injections are often performed in horses both within hospital and field settings, and they may represent the most important predisposing factor for thrombophlebitis in the horse (Gardner et al., 1991; Dias and de Lacerda Neto, 2013). Jugular vein thrombosis in racehorses is one of the most commonly detected, undesirable iatrogenic complications, particularly during intensive care. Symptoms of thrombosis vary according to the size and nature of the thrombose in addition to the age of thrombose to develop (Dolente et al., 2005; Russell et al., 2010). In most horses, affected horses notice a decrease in performance, and depression with objective signs at the site of the thrombose such as local swelling, neck stiffness, pain, and a cord-like jugular vein (Moreau and Lavoie, 2009). As the jugular vein extends parallel to the airway and the nerves supplying the larynx (recurrent laryngeal nerve) (Cercone et al., 2019) in the horse, it is possible that a thrombose in the jugular vein may cause mechanical pressure on the airways and affect the flow or mechanical presser on recurrent laryngeal nerve particularly during exercise (Steel et al., 2021; Burns et al., 2023). However, jugular vein thromboembolism and its effect on respiratory disorders as a risk factor that increases the severity of bleeding in racehorses has not been studied. In the present study, we assume that there is a relationship between horses suffering from EIPH and the presence of a pathological thrombose in the jugular vein. Therefore, the objectives of this study were to study the relationship between EIPH and the presence of jugular vein thrombose in racehorses. Material and MethodsAnimals and clinical examinationForty-eight thoroughbred racehorses (17 geldings, 11 males and 20 females) with median age (6 years, range 3–11) and mean ± standard deviation of bodyweight (448.5 ± 75.5 kg), were enrolled in the study. All horses were randomly selected from exercise intolerance horses brought to the Veterinary Teaching Hospital, College of Veterinary Medicine, King Faisal University. All horses in the present study are used for distance races between 1,200 and −2,000 meters, and these cases were collected during the racing season between October 2022 and May 2023. For all horses, detailed history and general examination were done. Only horses that suffered from exercise intolerance in the last 2 weeks, with respiratory symptoms such as noisy sounds, nasal bleeding regarding or chronic coughing, were included in the study. Exercise intolerance horses that came to the veterinary hospital, and with high fever or musculoskeletal disorders, which may be the cause of decreased performance, were excluded from this study. All horses did an exercise similar to racing on the morning of the examination day, and then they were brought to the veterinary hospital for examinations. EndoscopyAfter completing the clinical examination, upper and lower airway endoscopy was performed on all of the horses. For the Tracheobronchoscopy examination, the horses were placed in an examination stand and were intravenously sedated with Xylazine (Xylazine ® 0.5 mg/kg i.v). The Tracheobronchoscopy examinations were performed using a flexible 3 m videoendoscope (EVIS Olympus, OLYMPUS AUSTRIA GmbH., Vienna). A flexible videoendoscope was passed through the left nasal passage, and the upper and lower airway tract of the respiratory system was visualized. Tracheobronchoscopy was performed to verify whether EIPH had occurred. The grading of EIPH horses using an endoscope was recorded within the present study according to (Leguillette et al., 2016) with the following criteria: Grade 0: No blood is observable in the airways; Grade 1: Small flecks of blood or short, thin streams of blood are visible on the wall of trachea; Grade 2: Two short streams of blood or long stream are visible, covering about one-third of the trachea; Grade 3: Several long streams of blood covering more than one-third of the trachea are visible; Grade 4: Many streams of blood covering more than 90% of the surface of the trachea are visible. Jugular vein examinationAfter the bronchoscopy procedure, ultrasonography for jugular vein in each side was performed (ALOKA, Hitachi Aloka Medical, Ltd. Tokyo, Japan). Hair was shaved from the upper half of the jugular vein and the jugular grooves were cleaned with 90% ethanol. To ensure adequate contact with the transducer, a coupling gel was applied. Jugular vein thrombose were performed using a 5 MHz linear transducer B mode. The regularity and presence of blood flow, individual characteristics of segments of the thrombi, and preoperative vascular evaluation were evaluated in transverse and longitudinal sections from the cranial to the caudal part of the jugular vein. The thrombi were presented as a hypoechoic mass within the blood vessel in all animals, as described by (Reef, 2010). The presence of blood flow, length and characteristics of the thrombose, and venous compressibility under the ultrasound transducer pressure were assessed. A jugular vein thrombose is identified and observed by the presence of irregularly shaped hyperechoic luminal mass with homogenous echogenicity and wall thickening and or, less frequently, inhomogeneous texture with scattered hyper- and/or hypo-echoic spots. A jugular vein thrombose was considered present if the blood clot blocked more than 50% of the lumen of the jugular vein. Ethical approvalAll experimental procedures used in this study were approved by the Ethics Committee at King Faisal University, Saudi Arabia (Permission number KFU-REC / 2022—10—01). All applicable international, national, and institutional (King Faisal University) guidelines for the care and use of animals were followed. ResultsA general physical examination was conducted on the exercise intolerance horses that were enrolled in this study with respiratory disorders. Horses suffering from other disorders like lameness or any injuries resulting in exercise intolerance were excluded from the study. While performing the respiratory endoscope to determine the degree of EIPH, it was noted that many cases suffered from laryngeal paralysis in different degrees. We were not able to assess the degree of laryngeal paralysis due to the state of sedation that was given to the horses before the endoscopy. The present study indicates that about 40% of these horses suffered from EIPH of varying degrees (Fig. 1). Most of the horses that suffered from EIPH had a grade two (42.1%) and grade three (36.8%) of bleeding, while only one case was recorded with grade four of bleeding (5.3%) (Fig. 2). Based on comparison between horses affected with EIPH and the presence of jugular vein thrombose using ultrasound, it found that about 60% of the horses had jugular vein thrombose in one side, while only one horse (2.08%) had bilateral jugular vein thrombose. The jugular vein thrombose was in most cases (nine cases) on the left side, while only two cases had thrombose in the right jugular vein (Fig. 3). In most cases found that the suture of the jugular vein in affected horses was visibly distended without performing tourniquet. Jugular vein palpation showed stiffening with tubular, firm, and sensitive aspects that did not decline to the compression due to the presence of thrombus. Ultrasonography performed in the induction showed thrombus with heterogeneous aspect, with lower echogenicity compared to the blood and surrounding tissues, totally obstructing the vascular lumen. Most cases of jugular vein thrombosis were of the chronic type, as local heat and pain were not observed during preparing the site for the ultrasound. Table (1) showed that about 41% of exercise intolerance horses in the present study had no EIPH with the absence of jugular vein thrombose, while about 17% of horses with no bleeding had jugular vein thrombose. On the other hand, it was found that about 58% of the horses in this study did not have jugular vein thrombosis. Interestingly, about 25% of the studied animals had both jugular vein thrombose and EIPH. In addition, it was observed also that the number of horses with left jugular vein thrombosis was approximately two times higher in comparison to the right side.
Fig. 1. Exercise intolerance horses classified based on the presence of EIPH.
Fig. 2. The number and percentage of horses with EIPH’s degree in horses suffering from exercise intolerance.
Fig. 3. The number and percentage of horses suffering from EIPH based on the presence of jugular vein thrombosis. Table 1. The association between the presence and degree of EIPH and the presence of jugular vein thrombose in horses affected with exercise intolerance.
DiscussionTo the best of our knowledge, studies on the association between jugular venous thrombosis and EIPH in Thoroughbred racehorses are rare. Many risk factors that contribute to the formation of pulmonary hemorrhage in racehorses were investigated with the thoroughbred breed being one of the most susceptible breeds to EIPH ( Tarancon et al., 2019; Lo Feudo et al., 2021; Rocchigiani et al., 2022). The age factor, the period of use of the horse in races, the temperature, and annual season (Birks and others 2003; Hinchcliff and others 2009), in addition to some diseases associated with high blood pressure or decreased respiratory performance during the race, were confirmed as risk factors (da Silva et al., 2017; Lo Feudo et al., 2022). The increase in the rate of EIPH in horses in this study (39% of exercise intolerance horses), which was conducted in the desert environment of the Kingdom of Saudi Arabia, could be related to risk factors that induce bleeding like dust and high temperatures during races more than in other regions of the world (Poole and Erickson, 2016). Most EIPH grades in the current study were between two and three (about 79%), which may explain the fact that light bleeding is unnoticed by breeders and requires bronchoalveolar lavage fluid (BALF) cytology technique to identify it (Cascardo et al., 2022; Bertram et al., 2023), while in cases of severe bleeding, horses may have been excluded earlier from participating in the races (Tarancon et al., 2019; Lo Feudo et al., 2022). Racehorses are exposed to venous thrombosis problems more than other horse breeds as a result of receiving large quantities of medications and saline serums intravenously when prepared for competitions (Dolente et al., 2005; Dias and de Lacerda Neto, 2013). In the current study, EIPH was found to be the main cause of exercise intolerance in racehorses by approximately 40%, which is similar to previous reports (Leguillette et al., 2016; Ellis et al., 2022). Similar results to the current study regarding the degree of EIPH were previously reported by (Leguillette et al., 2016; Júnior et al., 2021), with most of the horses suffering from second to third-degree of EIPH. A relationship between respiratory distress and injuries to the jugular vein has been reported in humans previously (Knoblanche, 1979; Bitar et al., 2003; Gattas et al., 2007; Archibald et al., 2010;), while in veterinary medicine no link between respiratory disorders and jugular vein disorders has been reported before. In agreement with our observation, Burns et al. (2023) reported an association between laryngeal hemiplegia and EIPH in racehorses. In the current study, we were not able to accurately assess the state of paralysis in the larynx due to the sedation that was given to the horse for the bronchoscopy. The results of the current study regarding the increased probability of EIPH in horses that have left jugular vein thrombosis more than in the right side could be explained by the influence of the left recurrent laryngeal nerve, which affects the function of the larynx during racing, increasing the chance of pulmonary hemorrhage (Chalmers et al., 2012; Burns et al., 2023). The association between jugular vein thrombosis and increased EIPH in this study can be a result of direct compression on the airways in the level of jugular vein thrombose causing an imbalance in the flow of air through the trachea during the race, decreasing the quantity of air during inspiration and leading to EIPH (Mazan, 2022). In conclusion, it is necessary to focus on the risk factors that predispose to the development of EIPH in racehorses, especially in competition in desert environmental countries. It should also be highlighted that jugular vein thrombosis may cause disorders-associated damage to the vessels and anatomical structures close to it, such as the trachea and esophagus. Emphasis must also be placed on the expected effect of jugular vein thrombosis on recurrent laryngeal neuropathy and its relationship to pulmonary hemorrhage. AcknowledgementsThe author would like to thank the authorities of the Veterinary Teaching Hospital, College of Veterinary Medicine, King Faisal University (Al-Hasa, Saudi Arabia) for their kind cooperation in conducting this valuable study. Many thanks to Mohamed Al-Salman from Veterinary Teaching Hospital, College of Veterinary Medicine, King Faisal University, KSA) for arranging the endoscopy procedures. Conflict of interestThe author declares that there is no conflict of interest. FundingNone. Data availabilityAll data are provided in the manuscript. ReferencesArchibald, D.J., Carlson, M.L. and Kasperbauer, J.L., 2010. Respiratory distress requiring surgical intervention following traumatic central internal jugular vein cannulation: review of 2 cases. Laryngoscope. 120(Suppl. 4), S127. Bertram, C.A., Marzahl, C., Bartel, A., Stayt, J., Bonsembiante, F., Beeler-Marfisi, J., Barton, A.K., Brocca, G., Gelain, M.E., Glasel, A., Preez, K.D., Weiler, K., Weissenbacher-Lang, C., Breininger, K., Aubreville, M., Maier, A., Klopfleisch, R. and Hill, J., 2023. Cytologic scoring of equine exercise-induced pulmonary hemorrhage: performance of human experts and a deep learning-based algorithm. Vet. Pathol. 60, 75–85. Birks, E.K., Durando, M.M. and McBride, S., 2003. Exercise-induced pulmonary hemorrhage. Vet. Clin. North Am. Equine Pract. 19, 87–100. Bitar, F.F., Obeid, M., Dabbous, I., Hayek, P., Akel, S. and Mroueh, S., 2003. Acute respiratory distress associated with external jugular vein catheterization in the newborn. Pediatr. Pulmonol. 36, 549–550. Burns, J.J., MacMillan, K.M. and John, E., 2023. Prevalence of exercise-induced pulmonary hemorrhage, tracheal mucus and recurrent laryngeal neuropathy in competitive draft pulling horses. J. Equine Vet. Sci. 129, 104895. Cascardo, B., Bernardes, C., de Souza, G.N., Silva, K.M., Pires, N.R., de Alencar, N.X. and Lessa, D.A.B., 2022. Diagnostic value of tracheal wash cytology for monitoring exercise-induced pulmonary hemorrhage in thoroughbred racehorses. J. Equine Vet. Sci. 118, 104128. Cercone, M., Hokanson, C.M., Olsen, E., Ducharme, N.G., Mitchell, L.M., Piercy, R.J. and Cheetham, J., 2019. Asymmetric recurrent laryngeal nerve conduction velocities and dorsal cricoarytenoid muscle electromyographic characteristics in clinically normal horses. Sci. Rep. 9, 2713. Chalmers, H.J., Yeager, A.E., Cheetham, J. and Ducharme, N., 2012. Diagnostic sensitivity of subjective and quantitative laryngeal ultrasonography for recurrent laryngeal neuropathy in horses. Vet. Radiol. Ultrasound. 53, 660–666. Crispe, E.J. and Lester, G.D., 2019. Exercise-induced pulmonary hemorrhage: is it important and can it be prevented? Vet. Clin. North Am. Equine Pract. 35, 339–350. da Silva, K.M., Otaka, J.N.P., Goncalves, C.A.P., Silva, E.G.A., de Alencar, N.X. and Lessa, D.A.B., 2017. Association between exercise-induced pulmonary hemorrhage and inflammatory airway disease in polo ponies. J. Equine Sci. 28, 55–59. Dias, D.P. and de Lacerda Neto, J.C., 2013. Jugular thrombophlebitis in horses: a review of fibrinolysis, thrombus formation, and clinical management. Can. Vet. J. 54, 65–71. Dolente, B.A., Beech, J., Lindborg, S. and Smith, G., 2005. Evaluation of risk factors for development of catheter-associated jugular thrombophlebitis in horses: 50 cases (1993-1998). J. Am. Vet. Med. Assoc. 227, 1134–1141. Ellis, K.L., Contino, E.K. and Nout-Lomas, Y.S., 2022. Poor performance in the horse: diagnosing the non-orthopaedic causes. Equine Vet. Edu. 35, 208–224. Gardner, S.Y., Reef, V.B. and Spencer, P.A., 1991. Ultrasonographic evaluation of horses with thrombophlebitis of the jugular vein: 46 cases (1985-1988). J. Am. Vet. Med. Assoc. 199, 370–373. Gattas, N., Solt, I., Loberant, N., Hazani, E. and Rimon, D., 2007. [Parathyroid cyst associated with acute respiratory failure and jugular vein thrombosis]. Harefuah. 146, 599–601. Gold, J.R., Knowles, D.P., Coffey, T. and Bayly, W.M., 2018. Exercise-induced pulmonary hemorrhage in barrel racing horses in the Pacific Northwest region of the United States. J. Vet. Intern. Med. 32, 839–845. Hinchcliff, K.W., Morley, P.S. and Guthrie, A.J., 2009. Efficacy of furosemide for prevention of exercise-induced pulmonary hemorrhage in thoroughbred racehorses. J. Am. Vet. Med. Assoc. 235, 76–82. Júnior, A., Silva, L. and Oliveira, T., 2021. Relation between exercise-induced pulmonary hemorrhage and findings in upper airway and trachea in Thoroughbred racehorses. Revista Acadêmica Ciência Anima. 19, 1–7. Knoblanche, G.E., 1979. Respiratory obstruction due to haematoma following internal jugular vein cannulation. Anaesth. Intensive Care. 7, 286. Leguillette, R., Steinmann, M., Bond, S.L. and Stanton, B., 2016. Tracheobronchoscopic assessment of exercise-induced pulmonary hemorrhage and airway inflammation in barrel racing horses. J. Vet. Intern. Med. 30, 1327–1332. Lo Feudo, C.M., Stucchi, L., Alberti, E., Stancari, G., Conturba, B., Zucca, E. and Ferrucci, F., 2021. The role of thoracic ultrasonography and airway endoscopy in the diagnosis of equine asthma and exercise-induced pulmonary hemorrhage. Vet Sci. 8(11), 276. Lo Feudo, C.M., Stucchi, L., Stancari, G., Alberti, E., Conturba, B., Zucca, E. and Ferrucci, F., 2022. Associations between exercise-induced pulmonary hemorrhage (EIPH) and fitness parameters measured by incremental treadmill test in standardbred racehorses. Animals (Basel). 12(4), 449. Lopez Sanchez, C.M., Kogan, C., Gold, J.R., Sellon, D.C. and Bayly, W.M., 2020. Relationship between tracheobronchoscopic score and bronchoalveolar lavage red blood cell numbers in the diagnosis of exercise-induced pulmonary hemorrhage in horses. J. Vet. Intern. Med. 34, 322–329. Mazan, M., 2022. Equine exercise physiology-challenges to the respiratory system. Anim. Front. 12, 15–24. Moreau, P. and Lavoie, J.P., 2009. Evaluation of athletic performance in horses with jugular vein thrombophlebitis: 91 cases (1988-2005). J. Am. Vet. Med. Assoc. 235, 1073–1078. Poole, D.C. and Erickson, H.H., 2016. Exercise-induced pulmonary hemorrhage: where are we now? Vet. Med. (Auckl). 7, 133–148. Reef, M.C.M., 2010. Thrombophlebitis, In: Bowen, M.C.M. (Ed.), Cardiology of the horse. Saunders Elsevier, pp: 272–274. Rocchigiani, G., Verin, R., Uzal, F.A., Singer, E.R., Pregel, P., Ressel, L. and Ricci, E., 2022. Pulmonary bleeding in racehorses: a gross, histologic, and ultrastructural comparison of exercise-induced pulmonary hemorrhage and exercise-associated fatal pulmonary hemorrhage. Vet. Pathol. 59, 973–982. Russell, T.M., Kearney, C. and Pollock, P.J., 2010. Surgical treatment of septic jugular thrombophlebitis in nine horses. Vet. Surg. 39, 627–630. Steel, C.M., Walmsley, E.A., Anderson, G.A., Coles, C.A., Ahern, B. and White, J.D., 2021. Immunohistochemical analysis of laryngeal muscle of horses clinically affected with recurrent laryngeal neuropathy. Equine Vet. J. 53, 710–717. Sullivan, S. and Hinchcliff, K., 2015. Update on exercise-induced pulmonary hemorrhage. Vet. Clin. North Am. Equine Pract. 31, 187–198. Takahashi, T., Hiraga, A., Ohmura, H., Kai, M. and Jones, J.H., 2001. Frequency of and risk factors for epistaxis associated with exercise-induced pulmonary hemorrhage in horses: 251,609 race starts (1992-1997). J. Am. Vet. Med. Assoc. 218, 1462–1464. Tarancon, I., Armengou, L., Melendez-Lazo, A., Pastor, J., Rios, J. and Jose-Cunilleras, E., 2019. Prevalence of exercise-induced pulmonary hemorrhage in competing endurance horses. J. Am. Vet. Med. Assoc. 255, 710–715. Vinardell, T., David, F., Galezowski, A.M., Ali, M., Qasim, M., Massie, S.L., McCrae, P., Filho, S. and Leguillette, R., 2023. Free swimming and exercise-induced pulmonary hemorrhage in endurance horses: a preliminary study. J. Equine Vet. Sci. 120, 104182. | ||
| How to Cite this Article |
| Pubmed Style Turke Shawaf. Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses. Open Vet. J.. 2024; 14(5): 1111-1116. doi:10.5455/OVJ.2024.v14.i5.4 Web Style Turke Shawaf. Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses. https://www.openveterinaryjournal.com/?mno=183464 [Access: January 25, 2026]. doi:10.5455/OVJ.2024.v14.i5.4 AMA (American Medical Association) Style Turke Shawaf. Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses. Open Vet. J.. 2024; 14(5): 1111-1116. doi:10.5455/OVJ.2024.v14.i5.4 Vancouver/ICMJE Style Turke Shawaf. Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses. Open Vet. J.. (2024), [cited January 25, 2026]; 14(5): 1111-1116. doi:10.5455/OVJ.2024.v14.i5.4 Harvard Style Turke Shawaf (2024) Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses. Open Vet. J., 14 (5), 1111-1116. doi:10.5455/OVJ.2024.v14.i5.4 Turabian Style Turke Shawaf. 2024. Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses. Open Veterinary Journal, 14 (5), 1111-1116. doi:10.5455/OVJ.2024.v14.i5.4 Chicago Style Turke Shawaf. "Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses." Open Veterinary Journal 14 (2024), 1111-1116. doi:10.5455/OVJ.2024.v14.i5.4 MLA (The Modern Language Association) Style Turke Shawaf. "Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses." Open Veterinary Journal 14.5 (2024), 1111-1116. Print. doi:10.5455/OVJ.2024.v14.i5.4 APA (American Psychological Association) Style Turke Shawaf (2024) Jugular venous thrombosis as a risk factor for Exercise-induced pulmonary hemorrhage in Thoroughbred racehorses. Open Veterinary Journal, 14 (5), 1111-1116. doi:10.5455/OVJ.2024.v14.i5.4 |