| Research Article | ||
Open Vet. J.. 2024; 14(11): 3047-3054 Open Veterinary Journal, (2024), Vol. 14(11): 3047-3054 Research Article Biological markers as an additional method of determining drowningEmina Dervišević1, Nina Čamdžić2, Ermin Mašić3, Muhamed Katica4, Nedim Šuta3, Edina Spahić5, Edina Lazović2 and Aida Bešić4*1Department of Forensic Medicine, Faculty of Medicine, University of Sarajevo, Sarajevo, Bosnia and Herzegovina 2Department of Pathology, Faculty of Medicine, University of Sarajevo, Sarajevo, Bosnia and Herzegovina 3Department of Biology, Faculty of Science, University of Sarajevo, Sarajevo, Bosnia and Herzegovina 4Department of Clinical Sciences Veterinary Medicine, Veterinary faculty, University of Sarajevo, Sarajevo, Bosnia and Herzegovina 5Faculty of Medicine, University of Sarajevo, Sarajevo, Bosnia and Herzegovina *Corresponding Author: Aida Bešić. Department of Clinical Sciences Veterinary Medicine, Veterinary faculty, University of Sarajevo, Sarajevo, Bosnia and Herzegovina. Email: katicaaida1 [at] gmail.com Submitted: 04/09/2024 Accepted: 12/10/2024 Published: 30/11/2024 © 2024 Open Veterinary Journal
AbstractBackground: There is no specified diagnostic procedure that can help in determining the cause of death and the diagnosis of drowning because the pathohistological signs are almost identical and non-specified. Aim: Our study aims to recognize and prove diatom appearance in organs from a forensic aspect in Bosnia and Herzegovina, and to examine which is the more specific method in the diagnosis of drowning, the diatom test or the pathohistological finding. Methods: Rats of the recommended body weight were divided into four groups: G1 (n=8; mechanism of death—asphyxia; cause of death—suffocation, submerged 1 hour after death); G2 (n=8: mechanism of death-asphyxia; cause of death-suffocation, immersed 72 hours after death); G3 (n=8: mechanism of death-asphyxia; cause of death-drowning, autopsy immediately after death), and G4 (n=8: mechanism of death-asphyxia; cause of death-drowning, post mortem 24 hours after death). Results: During the diatom analysis, four species of diatoms, Diatoma vulgaris, Melosira varians, Epithemia adnata, and Cymbella sp, were successfully recovered from the stomach. Microscopic analysis did not detect diatoms in the kidneys and brains of rats, while the pathohistological changes were relatively uniform. Conclusion: Our results propose that the diatom test is a sustainable tool for supporting the diagnosis of drowning in the forensic pathology analysis of the cause of death. This experimental study is a starting point toward the optimization of tests and sampling in cases of unexplained etiology. Keywords: Diatom, Forensic, Microscopic, Organs, Postmortem. IntroductionAn unexplained death with a suspicious outcome that is sudden and/or violent must be the subject of a detailed investigation, under the jurisdiction of the Prosecutor’s Office of every legal state. Although the process of drowning is described in detail in the literature, drowning is still an unexplained topic and one of the hardest diagnoses in forensic medicine practice, which requires reliable information about the investigation, such as the scene of the event, a witness report (Saukko and Knight, 2004; Lunetta and Modell, 2005; Piette and De Letter, 2006; Fucci et al., 2017), and of course the autopsy as the gold standard for determining the cause of death. Optimizing the “Diatom test” method—above all requires the development of workable capacity and an integrity knowledge of the taxonomy of diatoms. Despite the multidisciplinary application of methods during death investigation, the use of diatoms can be good support, with the awareness of certain limitations, respectable. Diatoms are types of phytoplankton, photoautotrophic microscopic algae that most often live in freshwater ecosystems and as such remain in biological tissues for a long time. They are easily detached from the tissue /organs using acidic digestive extractions (Lunetta and Modell, 2005; Fucci et al., 2017; Carballeira et al., 2018; Kumar et al., 2023). The main intention of diatom examination in forensics is to distinguish death by immersion from postmortem immersion of bodies in water when the cause of death is not drowning (Fucci et al., 2017; Kumar et al., 2023). The World Health Organization defines drowning as the process of experiencing respiratory damage due to submersion/immersion in a liquid (Lockyer, 2021) with accompanying sediment components and microorganisms. Such liquid enters the mouth and nose, passes through the trachea, reaches the lungs, and then through the alveoli into the bloodstream, where it is transported by circulation to other organs and deposited in their capillaries (Lunetta et al., 1998). There are no specific diagnostic procedures that can help in determining the cause of death and the diagnosis of drowning because the pathohistological signs are almost identical and non-specified. Macroscopically, they can be diagnosed with pulmonary edema, as well as with the presence of sludge and sediment particles in the lungs, or bronchioles. The detection of diatoms in other organs is currently considered an important “biological marker” for the diagnosis of drowning in human forensic pathology (Fucci et al., 2017; Piegari et al., 2019). “Diatom test” is based on the assumption that the victim must be alive to aspirate water with diatoms, which later circulate to other organs. The implementation of the “Diatom test” method or the diatom test method can be a very good and useful method of presenting the true cause of drowning and the final diagnosis of the drowned person (Lunetta et al., 1998; Piette and De Letter, 2006; Fucci et al., 2017; Carballeira et al., 2018; Piegari et al., 2019; Lockyer, 2021; Kumar et al., 2023; Tsuneya et al., 2023). However, although the diatom test is a useful forensic tool, as such it has its limitations and potential sources of error that can affect its reliability and accuracy. It is a priority to consider these limitations when interpreting test results and to use the test in conjunction with other evidence (Lindeque and Bornman, 2016). The goal of our study is to recognize and prove the presence of diatoms in target organs from a forensic aspect in Bosnia and Herzegovina, as a support to macroscopic and microscopic diagnosis of drowning. Materials and MethodsExperimental animalsThirty-two adult albino Wistar rats of the recommended body weight were divided into four groups, as follows:
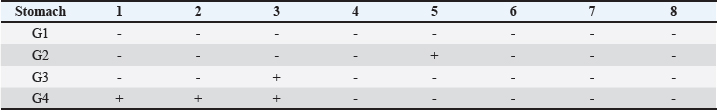
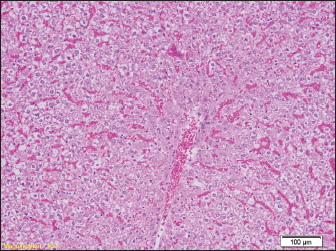
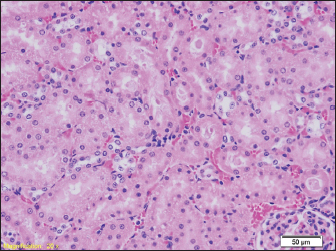
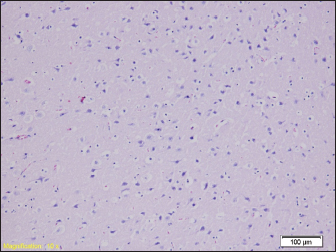
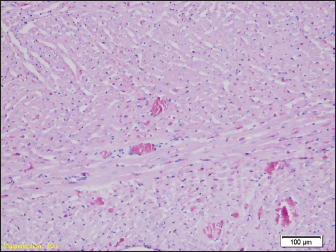
The diatom test protocol was carried out in accordance with the available guidelines for the analysis of diatoms for the assessment of the ecological state of waters from the Bosna River. Water samples and laboratory processing of algaeFor this research, a water sample and microscopic algae were taken at the confluence of the Željeznica River and the Bosna River, from the coastal part and coordinates: 43°50’28’’. N and 18°17’10’’ E at 490 m.a.s.l. No precipitation was recorded during water sampling. The water color during sampling was green, and the place from which the water and microscopic algae were sampled was partially shaded. At the place where the water sampling was done, Alnetea glutinosae flood forest vegetation dominated. Samples were collected using plastic buckets/containers. Before sampling the microscopic algae, the physical and chemical parameters of the water were measured, and with the portable multimeter Orion Star A329, the pH value of the water was measured, which was 7.35. The identification of diatoms was argued according to Cantonati and Lange-Bertalot (2011), and the nomenclature of the identified diatom species was adapted according to the online database AlgaeBase (Guiry and Guiry 2020). Ethics approvalThis study was conducted at the University of Sarajevo (Veterinary faculty, Faculty of Medicine and Faculty of Science) Bosnia and Herzegovina, and was approved by the local ethics commission of the Ethics Committee of the Medical Faculty of the University of Sarajevo, Bosnia and Herzegovina (02-3-4-AK-6589/23). ResultsTwo types of analysis were performed, microscopic—for the presence of diatoms and pathohistological. Analysis of diatomsSample-stomach of rats With microscopic analysis was detected the diatoms appeared in the stomachs of rats. Diatoms were detected in groups G2, G3, and G4, but were not detected in G1. The number of taxa in the analyzed suspension in samples belonging to groups G2, G3, and G4 was low. The values ranged mostly from 1 to 8 taxa. Only one taxon (Diatoma vulgaris) was found within G2 (U5), while only one taxon (Melosira varians) was also found within G3 (U3). Eight taxa were found within group G4, namely: Epithemia adnata (U1), Nitzschia palea, Encyonema ventricosa, Gomphonema minutum, Cocconeis pediculus, Encyonema minutum, Navicula lanceolata, Ulnaria ulna (U2), and Cyambella sp. (U3). The results are presented in Table 1. Photomicrographs (LM) of diatoms found in the stomach of rats within the investigated groups are presented in Figures 1–4. Sample-stomach of ratsMicroscopic analysis did not detect diatoms in the kidneys of rats. Pathohistological examination of organs in drowningIn the liver samples of all groups of rats, relatively uniform changes are observed, which in each sample include a certain degree of congestion, with overcrowding of the centrolobular veins, but also the veins of the portal spaces, as well as the dilation of the sinusoids filled with erythrocytes, while the hepatocytes in places show signs of fluffy degeneration (Figs. 5 and 6.) Table 1. Comparative presentation of the presence of diatoms in the investigated samples in the stomach.
Fig. 1. Diatoma vulgaris (G-B5).
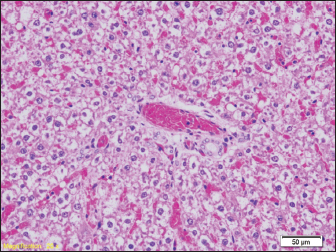
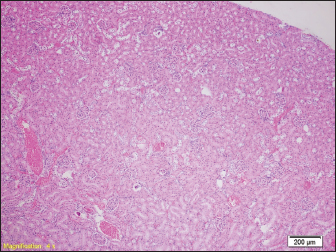
Fig. 2. Melosira varians (G-C3). Signs of hydropic and vacuolar degeneration can be seen in the kidney samples of all groups of rats, and signs of acute tubular necrosis can be seen in one of the samples (group G2) (Figs. 7 and 8). Brain tissue samples of all groups of rats show a lower or higher degree of edema (Fig. 9). No significant pathological changes were found in the heart muscle tissue samples in terms of necrosis, hypertrophy, atrophy, and so on. Congestion of blood vessels was observed (Fig. 10). DiscussionDetermining drowning is a challenge in both human and veterinary forensic medicine. It is a fact that two basic methods of examining drowned persons are used in forensic medical practice, the macroscopic examination by the autopsy and the microscopic examination by the pathologist, but the implementation of the Diatom test and the detection of diatoms in other organs is currently considered an important “biological marker” for the diagnosis of drowning in forensic pathology (Fucci et al., 2017; Piegari et al., 2019). Guided by the successfully applied diatom test, most often on the lungs, we decided to point out that in addition to the lungs, diatoms can reach other organs through circulation, such as the stomach, from which we successfully identified four types of diatoms: Diatoma vulgaris, Melosira varians, Epithemia adnate, and Cymbella sp. (Fig. 2). Microscopic analysis did not detect diatoms in the kidneys and brains of rats. Some studies mention that diatoms can still be found in the kidneys (Coelho et al., 2016; Shen et al., 2019; Demirci et al., 2020; Tsuneya et al., 2023). Our results do not correspond to the previously mentioned statements, and a possible reason for this is the short period of distribution of diatoms before the autopsy was performed. In contrast to our results, diatoms were found in the kidney and liver material of all animals in the study by Piegari et al., 2019. The reason for such different results may be the contamination of organs with diatoms after death. However, the latest studies use modern in-house protocols to avoid organ contamination with diatoms after death. Differences in results are visible in studies by other authors. Luneta et al. found diatoms in slightly less than half of the samples in which death did not result from drowning, while Aurer and Möttönen did not find a single diatom in the internal organs of bodies that did not drown (Auer and Möttönen, 1938; Leunetta et al., 2013).
Fig. 3. Epithemia adnata (G-D1).
Fig. 4. Cymbella sp. (G-D3).
Fig. 5. Blood filling of hepatic sinusoids and centrolobular vein (HE, ×100).
Fig. 6. Congested portal blood vessels as well as sinusoids, and hepatocytes with balloon appearance in places (HE, ×200).
Fig. 7. Kidney parenchyma also shows signs of congestion (HE, ×40). Signs of hydropic and vacuolar degeneration can be seen in the kidney samples of all groups of rats, and signs of acute tubular necrosis can be seen in one of the samples (group G2) (Figs. 7 and 8).
Fig. 8. Signs of hydropic and vacuolar degeneration in epithelial cells of renal tubules (HE, ×200). Brain tissue samples of all groups of rats show a lower or higher degree of edema (Fig. 9).
Fig. 9. Brain tissue showing signs of pericellular and perivascular edema (HE, ×100).
Fig. 10. Heart muscle with congested interstitial blood vessels (HE, ×100). The problem of finding diatoms in the stomach and not in other organs can also mean a false positive test because diatoms can be eaten in the digestive tract or water and food that is consumed. Previous studies have already proven that diatoms can penetrate the barrier of the gastric mucosa and thus contaminate other organs, giving a false positive result (Du et al., 2023). We believe that in our study we have overcome this because the bodies of rats in whose stomachs diatoms were found were not kept submerged for such a long time that this barrier would be broken through. In our study, by histological examination of brain tissue, we found classic signs of edema, without the presence of diatoms. During drowning, due to cessation of breathing and reduced oxygen supply to the brain, anoxic damage to neurons and death of neurons occurs. We believe that the absence of signs of neuron degeneration in our study is due to the relatively short time after drowning when the samples were taken. Studies have proven that if resuscitation is started on time, the recovery of neurons can be complete (Timperman, 1969). Ikeda et al. found signs of shock in the brain tissue sample after drowning, which was histologically presented as microthrombosis of blood vessels, and hyaline and fibrin accumulations in brain thrombs (Ikeda et al., 1998). After a histological examination of the brain tissue of drowned rats, Mahrous et al. (2022) found signs of interstitial edema were found as well as degenerative neurons that were shrunken, with pyknotic nuclei and eosinophilic cytoplasm (Ibrahim et al., 2022). Signs of degenerative changes caused by drowning were found in the liver samples. It is believed that drowning and hypotension during recovery lead to irreversible changes in the organs caused by a lack of oxygen. Similar changes were found in other studies, where the liver showed small but numerous clusters of hyaline bodies in the liver sinusoids (Ikeda et al., 1998). Our results show signs of overcrowding of hepatic sinusoids with partially ballooned hepatocytes. These results were found in previous studies, where hepatocytes had hydropic degeneration (Ibrahim et al., 2022). The changes that can occur to the organs can largely depend on the type of water in which the drowning occurred, from salt water to fresh water. In our study, rats were drowned in water from the Bosnia River. Upon examination of the heart muscle, we found congested blood vessels, with no signs of degeneration. In contrast to our results, Mahrous et al., found signs of cardiac muscle cell damage after drowning in salt water, which were presented as a greater number of vacuoles in the cytoplasm, a reduced number of nuclei in the cells, and an inflammatory infiltrate, but also edema and congestion of blood vessels as in our results (Ibrahim et al., 2022). Christe et al. (2008) found an enlarged heart on the post-autopsy material, with an increased volume of the right atrium and right ventricle, while the left side of the heart was enlarged in only one person (Christe et al., 2008). Unfortunately, in the available forensic literature, we were able to find a limited number of studies that comparatively investigated macroscopic and microscopic changes after antemortem and postmortem drowning (Banting et al., 1938; McEwen and Gerdin, 2016). The most frequently mentioned changes in cases of drowning are found at the respiratory and cardiac levels and include pulmonary congestion, pulmonary edema and pulmonary hemorrhage, foam in the trachea, mouth, and nasal cavity, right ventricular detachment, and drowning of media into the stomach (Lindstedt and Schaeffer, 2002; Farrugia and Ludes, 2011; Szpilman et al., 2012; Munro and Munro, 2013). Pathohistological examination of the internal organs of rats of all groups in our study found uniform changes that were not significantly different between groups. Previous studies on human preparations have shown that such histological changes recorded on organs can also be found on the corpses of people who did not die due to drowning, so these are not characteristic histological changes for drowning (Farrugia and Ludes, 2011). In the experimental animal study by Piegara et al. (2019), non-specific histological changes were also found in the lungs, liver, and heart, which ultimately coincides with our results (Piegari et al., 2019). These findings indicate a small and insufficient contribution of the specifics of the autopsy and histological analyzes in determining the final cause of death in cases of drowning, and especially the distinction between antemortem and postmortem arrival of the body in the water. Since the same mechanism of death can have many causes of death, the signs found at autopsy in drowning are not conclusive as they may be discovered during autopsy for other suffocation deaths as well. For example, pulmonary edema or pulmonary hemorrhage, as well as right ventricular distension, can be observed in a wide range of diseases, such as allergic reactions, neurological diseases, and acute kidney diseases (Brown et al., 2008; Murray, 2011; Sureka et al., 2015). In our study, we used a combination of classic pathohistological descriptions of changes in several internal organs combined with observation of the appearance of diatoms in several organs. In this way, we excluded the possibility of false positive results that can be found in some cases. Previous quantitative studies have shown that there is a difference in the number of diatoms in false-positive and true-drowning cases. Therefore, the use of diatomaceous earth tests on only one branch cannot be a reliable predictor for the diagnosis of drowning, and the analysis of several organs in combination with other methods is recommended to obtain the most reliable finding of drowning (Shen et al., 2019). Previous studies also showed that the number of diatoms depends on the type of water medium in which the drowning occurred (Sonoda et al., 2022). However, studies have shown that there are statistical differences in the number of diatoms in false positive cases and actual drowning cases. Therefore, a comprehensive analysis of multiple organs, rather than just one organ, would be more useful for the diagnosis of drowning. Relatively uniform changes are observed in the liver samples of all groups of rats, which in each sample include a certain degree of congestion, with overcrowding of the centrolobular veins, but also the veins of the portal space, as well as dilation of sinusoids-filled with erythrocytes, while hepatocytes in places show signs of paper degeneration. Signs of hydropic and vacuolar degeneration can be seen in the kidney samples of all groups of rats, and signs of acute tubular necrosis can be seen in one of the samples (group G1). Brain samples from all groups of rats show a lower or higher degree of edema. No significant pathological changes in the sense of necrosis, hypertrophy, atrophy, and so on, were found in the heart muscle tissue samples. The only thing observed was congestion of blood vessels. The pathohistological findings of the kidneys in all examined groups indicate hydropic and vacuolar degeneration of the epithelial cells of the renal tubules, and the pathohistological findings of the brain in all groups show signs of pericellular and perivascular edema. In our study, we did not find diatoms in the kidneys. Previous studies prove that the number of diatoms found may be lower than expected, as in liver samples. Since the middle of the last century, there have been certain disagreements among numerous authors about the reliability of diatom findings in internal organs such as the kidney, liver, or bone marrow. The reason for this is the high rate of occurrence of false positive findings (Timperman, 1969). The results of the pathohistological examination of the kidneys in our study coincide with those of other authors. In previous studies, after drowning, signs of glomerular enlargement with hypercellular changes were found on the kidneys, signs of degeneration were present in the tubules, such as their uneven expansion and edema of the cells of the tubular walls, and in the interstitium, there were congested capillaries were present (Ibrahim et al., 2022). Seong et al. (2012) also reported signs of acute tubular necrosis after drowning (Seong et al., 2012). In contrast to our results, diatom abundance in the liver and kidney was in direct proportion with water density. In addition, the abundance of diatoms in the lungs, kidneys, and liver was positively correlated (Ren et al., 2021). Our results indicate that the diatom test should be combined with pathohistological analysis as support for the diagnosis of drowning. Therefore, a detailed analysis of multiple organs would be more useful. The pathohistological findings of the organs showed better specificity compared to the diatom test, respectively. Because there were only a small number of samples, and poor literature data on the presence of diatoms in the investigated organs, in our research we did not prove that diatoms or microscopic algae are in the brain and kidneys, but we did in the stomach. Our results suggest that the diatom test is a valid tool to support the diagnosis of drowning in the forensic pathology analysis of the cause of death. AcknowledgmentsNone. Conflict of interestThe authors declare that there is no conflict of interest. FundingThis research is supported by the Cantonal Ministry of Science, Higher Education and Youth of Bosnia and Herzegovina 2023/24; number: 27-02-35-37080-16/23. Authors’ contributionsAll authors contributed equally to this research. Data availabilityAll data are provided in the manuscript. ReferencesAuer, A. and Möttönen, M. 1938. Diatoms and drowning. Z. Rechtsmed. 101(2), 87–98. Banting, F.G., Hall, G.E., Janes, J.M., Leibel, B. and Lougheed, D.W. 1938. Physiological studies in experimental drowning (a preliminary report). Can. Med. Assoc. J. 39, 226–228. Brown, P.J., Skuse, A.M. and Tappin, S.W. 2008. Pulmonary haemorrhage and fibrillary glomerulonephritis (pulmonary-renal syndrome) in a dog. Vet. Rec. 162, 486–488. Cantonati, M. and Lange-Bertalot, H. 2011. Diatom monitors of close-to-pristine, very-low alkalinity habitats: three new Eunotia species from springs in nature parks of the south-eastern Alps. J. Limnol. 70, 209–221. Carballeira, R., Vieira, D.N., Febrero-Bande, M. and Muñoz Barús, J.I. 2018. A valid method to determine the site of drowning. Int. J. Legal. Med. 132(2), 487–497. Christe, A., Aghayev, E., Jackowski, C., Thali, M.J. and Vock, P. 2008. Drowning--post-mortem imaging fndings by computed tomography. Eur. Radiol. 18(2), 283–290. Coelho, S., Ramos, P., Ribeiro, C., Marques, J. and Santos, A. 2016. Contribution to the determination of the place of death by drowning—a study of diatoms’ biodiversity in Douro river estuary. J. Forensic. Leg. Med. 41, 58–64. Demirci, T., Sener, M.T., Sahpaz, A., Sener, E. and Kok, A.N. 2020. The diagnostic value of the changes in the renal glomerulus in the postmortem diagnosis of freshwater drownings. Am. J. Forensic. Med. Pathol. 41(2), 104–109. Du, Y., Xiang, Q., Niu, Y., Liu, L., Liu, J., Su, Q., Li, Z., Shi, H., Xu, Q., Wang, H., Zhao, J. and Liu, C. 2023. Diatoms pass through the gastrointestinal barrier and lead to false-positive: an animal experiment. Forens. Sci. Med. Pathol. 20(2), 351–359. Farrugia, A. and Ludes, B. 2011. Diagnostic of drowning in forensic medicine. 3th edition. In, Forensic medicine—from old problems to new challenges. Ed., Vieira, D.N. IntechOpen. Available via https://www.intechopen.com/books/forensic-medicine-from-old-problems-tonew-challenges/diagnostic-of-drowning-inforensic-medicine (Accessed 12 May 2019). Fucci, N., Campobasso, C.P., Mastrogiuseppe, L., Puccinelli, C., Marcheggiani, S., Mancini, L., Marino, L. and Pascali, V.L. 2017. Diatoms in drowning cases in forensic veterinary context: a preliminary study. Int. J. Legal. Med. 131(6), 1573–1580. Guiry, M.D. and Guiry, G.M. 2020. World-wide electronic publication, National University of Ireland. AlgaeBase. Available via http://www.algaebase.org, searched on 24 February 2023. Ibrahim, M.A., Hagras, A.M., Khalifaa, A.M., Ali, Z.A., Eid, G.A., Rehman, A. and El Serafi, O.S. 2022. Histopathological differentiation of drowning in freshwater and saltwater in rats: forensic point of view. Int. J. Morphol. 40(4), 1134–1146. Ikeda, N., Umetsu, K., Takahashi, H. and Suzuki, T. 1988. A delayed drowning death with histological findings of shock. Z. Rechtsmed. 100(4), 265–270. Kumar Pal, S., Bhardway, N. and Ahluwalia, A.S. 2023. Role of diatoms in forensics: a molecular approach. In: Chapter 9, Insights into the world of diatoms: from essentials to applications. Eds., Srivastava, P., Sardar Khan, A., Verma, J. and Dhyani, S. Wiley Online Library, pp. 143–163. Lindeque, P.K. and Bornman, M.S. 2016. Diatoms as a forensic tool: a review of literature and case work. Forens. Sci. Inter. 266, 251–257. Lindstedt, S.L. and Schaeffer, P.J. 2002. Use of allometry in predicting anatomical and physiological parameters of mammals. Lab. Anim. 36, 1–19. Lockyer, B.E. 2021. The body recovered from water: considerations for an approach to the non-suspicious post-mortem examination. Diagn. Histopath. 27(10), 411–417. Lunetta, P., Miettinen, A., Spilling, K. and Sajantila, A. 2013. False-positive diatom test: a real challenge? a post-mortem study using standardized protocols. Leg. Med. (Tokyo). 15, 229–234. Lunetta, P. and Modell. J.H. 2005. Macroscopical, microscopical and laboratory findings in drowning victims—a comprehensive review. 3th edition. In: Forensic pathology reviews. Ed., Tsokos, M and Turk, E.E. Totowa, NJ: Humana Press, pp: 3–77. Lunetta, P., Penttilä, A. and Hällfors, G. 1998. Scanning and transmission electron microscopical evidence of the capacity of diatoms to penetrate the alveolo-capillary barrier in drowning. Int. J. Legal. Med. 111(5), 229–237. Mahrous, A.I., Abeer, M.H., Athar, M.K., Zinab A.E.A., Galal, A.E., Abdullah, R. and Osama, E.S. 2022. Histopathological Differentiation of Drowning in Freshwater and Saltwater in Rats: Forensic Point of View. Int. J. Morphol. 40(4), 1134–1146. McEwen, B.J. and Gerdin, J. 2016. Veterinary forensic pathology: drowning and bodies recovered from water. Vet. Pathol. 53(5), 1049–1056. Munro, R. and Munro, H.J. 2013. Some challenges in forensic veterinary pathology: a review. Comp. Pathol. 149, 57–73. Murray, J.F. 2011. Pulmonary edema: pathophysiology and diagnosis. Int. J. Tuberc. Lung. Dis. 15, 155–160. Piegari, G., Biase, D.D., Prisco, F., Fico, R., Ilsami, R., Pozzato, N., Genovese, A. and Paciello, O. 2019. Diagnosis of drowning and the value of the diatom test in veterinary forensic pathology. Front. Vety. Sci. 14(6), 404. Piette, M.H. and De Letter, E.A. 2006. Drowning: still a difficult autopsy diagnosis. Foren. Sci. Int. 163(1-2), 1–9. Ren, L., Chen, Y.Q., Zhou, Q.L., Liu, Z.Z., Li, Y. and Liu, Q. 2021. Relationships between diatom abundances in rat organs and in environmental waters. Curr. Med. Sci. 41 (5), 981–986. Saukko, P. and Knight B. 2004. Knight’s forensic pathology. 3rd edition. London, UK: CRC Press, Taylor & Francis Group, pp: 406–408. Seong, E.Y., Rhee, H., Lee, N., Lee, S.J., Song, S.H., Lee, D.W. and Kwak, I.S. 2012. A case of severe acute kidney injury by near-drowning. J. Korean. Med. Sci. 27(2), 218–220. Shen, X., Liu, Y., Xiao C, Zheng, C., Huang, J., Shi, H., Xu, Q., Cheng, J., Liu, C. and Zhao, J. 2019. Analysis of false-positive results of diatom test in the diagnosis of drowning-would not be an impediment. Int. J. Legal. Med. 133(6), 1819–1824. Sonoda, A., Kakizaki, E., Shinkawa, N., Matsuda, H. and Yukawa, N. 2022. Conventional diatom testing using strong acid: (II) Number and types of diatoms detected in closed organs and lungs of 80 autopsy cases using only new Kjeldahl flasks. Forens. Sci. Int. 341, 111510. Szpilman, D., Bierens, J.J.L.M., Handley, A.J. and Orlowski, J.P. 2012. Drowning. N. Engl. J. Med. 366, 2102–2110. Sureka, B., Bansal, K. and Arora, A. 2015. Pulmonary edema—cardiogenic or noncardiogenic? J. Family. Med. Prim. Care. 4, 290. Timperman, J. 1969. Medico-legal problems in death by drowning. Its diagnosis by the diatom method. A study based on investigations carried out in Ghent over a period of 10 years. J. Forens. Med. 16(2), 45–75. Tsuneya, S., Yoshida, M., Hoshioka, Y., Chiba, F., Inokuchi, G., Torimitsu, S. and Iwase, H. 2023. Relevance of diatom testing on closed organs of a drowned cadaver who died after receiving treatment for 10 days: a case report. Leg. Med. 60, 102168. | ||
| How to Cite this Article |
| Pubmed Style Dervišević E, Čamdžić N, Mašić E, Katica M, Šuta N, Spahić E, Lazović E, Bešić A. Biological markers as an additional method of determining drowning. Open Vet. J.. 2024; 14(11): 3047-3054. doi:10.5455/OVJ.2024.v14.i11.33 Web Style Dervišević E, Čamdžić N, Mašić E, Katica M, Šuta N, Spahić E, Lazović E, Bešić A. Biological markers as an additional method of determining drowning. https://www.openveterinaryjournal.com/?mno=218840 [Access: January 25, 2026]. doi:10.5455/OVJ.2024.v14.i11.33 AMA (American Medical Association) Style Dervišević E, Čamdžić N, Mašić E, Katica M, Šuta N, Spahić E, Lazović E, Bešić A. Biological markers as an additional method of determining drowning. Open Vet. J.. 2024; 14(11): 3047-3054. doi:10.5455/OVJ.2024.v14.i11.33 Vancouver/ICMJE Style Dervišević E, Čamdžić N, Mašić E, Katica M, Šuta N, Spahić E, Lazović E, Bešić A. Biological markers as an additional method of determining drowning. Open Vet. J.. (2024), [cited January 25, 2026]; 14(11): 3047-3054. doi:10.5455/OVJ.2024.v14.i11.33 Harvard Style Dervišević, E., Čamdžić, . N., Mašić, . E., Katica, . M., Šuta, . N., Spahić, . E., Lazović, . E. & Bešić, . A. (2024) Biological markers as an additional method of determining drowning. Open Vet. J., 14 (11), 3047-3054. doi:10.5455/OVJ.2024.v14.i11.33 Turabian Style Dervišević, Emina, Nina Čamdžić, Ermin Mašić, Muhamed Katica, Nedim Šuta, Edina Spahić, Edina Lazović, and Aida Bešić. 2024. Biological markers as an additional method of determining drowning. Open Veterinary Journal, 14 (11), 3047-3054. doi:10.5455/OVJ.2024.v14.i11.33 Chicago Style Dervišević, Emina, Nina Čamdžić, Ermin Mašić, Muhamed Katica, Nedim Šuta, Edina Spahić, Edina Lazović, and Aida Bešić. "Biological markers as an additional method of determining drowning." Open Veterinary Journal 14 (2024), 3047-3054. doi:10.5455/OVJ.2024.v14.i11.33 MLA (The Modern Language Association) Style Dervišević, Emina, Nina Čamdžić, Ermin Mašić, Muhamed Katica, Nedim Šuta, Edina Spahić, Edina Lazović, and Aida Bešić. "Biological markers as an additional method of determining drowning." Open Veterinary Journal 14.11 (2024), 3047-3054. Print. doi:10.5455/OVJ.2024.v14.i11.33 APA (American Psychological Association) Style Dervišević, E., Čamdžić, . N., Mašić, . E., Katica, . M., Šuta, . N., Spahić, . E., Lazović, . E. & Bešić, . A. (2024) Biological markers as an additional method of determining drowning. Open Veterinary Journal, 14 (11), 3047-3054. doi:10.5455/OVJ.2024.v14.i11.33 |