| Case Report | ||
Open Vet. J.. 2021; 11(4): 680-685 Open Veterinary Journal, (2021), Vol. 11(4): 680–685 Case Report Conservative treatments for feline fibroadenomatous changes of the mammary glandGabriele Marino1*, Michela Pugliese1, Fabiana Pecchia1,2, Giuseppe Garufi3, Vincenzo Lupo1,4, Stefania Di Giorgio1 and Alessandra Sfacteria11Department of Veterinary Sciences, University of Messina, Messina, Italy 2Polivet, Rome, Italy 3Ambulatorio tre fontane, Reggio Calabria, Italy 4Almavet, Trapani, Italy *Corresponding Author: Gabriele Marino. Department of Veterinary Sciences, University of Messina, Messina, Italy. Email: marinog [at] unime.it Submitted: 15/07/2021 Accepted: 22/10/2021 Published: 21/11/2021 © 2021 Open Veterinary Journal
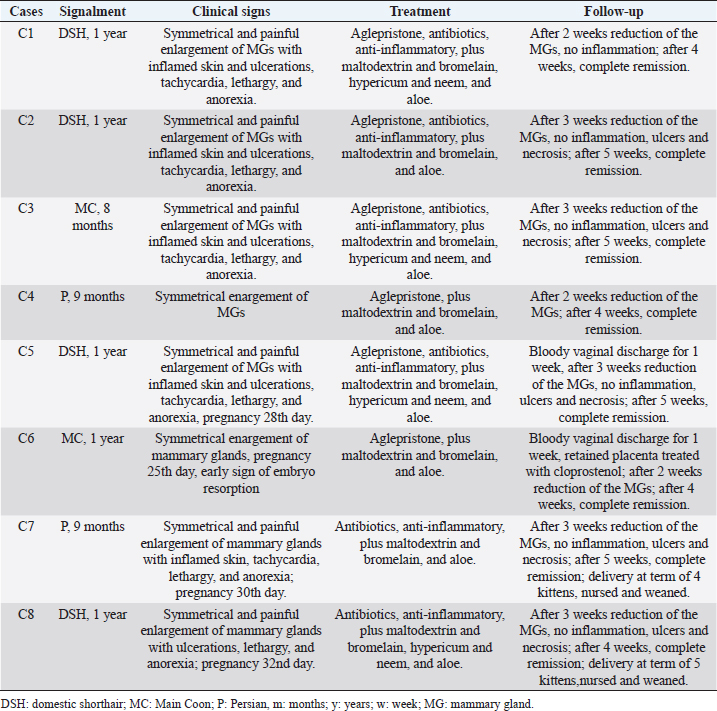
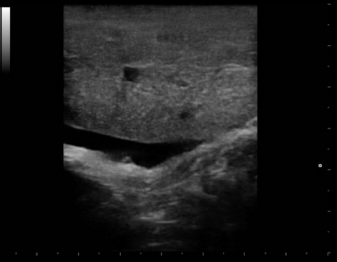
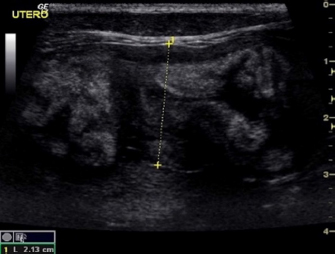
AbstractBackground: Fibroadenomatous changes (FAC) of the mammary gland in cats represents a benign, progesterone-associated fibroglandular proliferation of one or more mammary glands that may occur in intact female cats at the time of puberty, during pregnancy or pseudopregnancy, or in female and male cats of any age under progestin treatment. Nowadays, the elective treatment of FAC is based on the progesterone antagonist aglepristone. This study aimed to report the treatment of FAC with a combination of drugs designed to preserve mammary gland integrity, even in pregnant cats. Case Description: Eight sexually intact female cats with FAC showed mammary glands that were symmetrically enlarged and inflamed in all cases, and the skin was ulcerated in six cats. Four cats were on days 25–32 of pregnancy at presentation. Non-pregnant cats were treated with aglepristone and with a dietary supplement containing maltodextrin and bromelain. The mammary glands were massaged daily with an Aloe vera emollient gel. If the gland was inflamed or ulcerated, broad-spectrum antimicrobial, and anti-inflammatory treatments were given, and the ulcers were treated topically with a hypericum and neem-based cream. Two of the four pregnant cats were treated with the same therapeutic schedule plus cloprostenol to facilitate uterine emptying. Two pregnant cats underwent the same protocol except for aglepristone, which was not administered to safeguard the litter and see if the adjuvant therapy worked independently. At term, they delivered four and three kittens, respectively, that were normally nursed and weaned after 40 days. In all the studied cases, the mammary gland reduced in size 2–3 weeks after the start of the treatment and completely remitted after 4–5 weeks. Conclusion: This case series encourages adjuvant therapy in the course of FAC to preserve mammary gland integrity and functionality. Exploiting the natural decline of progesterone at the end of pregnancy (or pseudopregnancy), the therapy may also be used without aglepristone, when its use has other limitations. Keywords: Cat, Tumor, Aglepristone, Hypericum, Aloe. IntroductionFibroadenomatous changes (FAC) of the mammary gland in cats, also referred to as fibroepithelial or fibroadenomatus mammary hyperplasia, fibroadenoma complex, or mammary hypertrophy, are benign proliferations of the mammary ducts and mainly of the periductal connective tissue under progesterone dependence. The disease usually occurs in unspayed female cats at the time of puberty, during pregnancy or pseudopregnancy, or in female and male cats of any age under progestin treatment (Allen, 1973; Zappulli et al., 2019). Progesterone drives the development and growth of the mammary gland through the progesterone receptor on stromal and epithelial cells (Martín De Las Mulas et al., 2000). Some other local growth factors are probably involved even though progesterone is the main inductor of FAC (Mol et al., 1996). Two ultrasound and gross patterns have been described: the solid type with scant fluid accumulation and the parenchymal intraductal pattern with fluid-filled spaces (Hayden et al., 1989; Payan-Carreira, 2013). The two patterns can be combined in the same lesion or one can be predominant. The affected mammary gland shows a rapid increase in size diffusely, symmetrical or asymmetrical, ranging from 1.5 to even 18 cm (Payan-Carreira, 2013). In severe cases, some patients had erythematous and necrotic areas on their skin with systemic symptoms such as anemia, fever, tachycardia, apathy, and anorexia (Loretti et al., 2004). The severity of the disease has encouraged in the past non-conservative treatments such as ovariectomy to remove the source of progesterone associated or not with a total or partial mastectomy to remove the damaged mammary glands. Excision of the ovaries usually leads to regression of the mammary tissue within 3 to 4 weeks, but in some cases, regression is not achieved (Görlinger et al., 2002; de Melo et al., 2020). Mastectomy is a difficult procedure to perform in FAC-affected cats because of the extensiveness of the mammary glands and the poor survival rate; it is the last treatment option to be considered in non-responsive lesions or when the mammary gland presents extensive necrotic changes (Payan-Carreira, 2013). The use of aglepristone as the elective drug for the treatment of FAC has been exploited (Wehrend et al., 2001; Görlinger et al., 2002; Vitasek and Dendisova, 2006; de Melo et al., 2020), reducing but not cancelling the number of cats that need a mastectomy. Finally, there are no therapeutic schedules to treat FAC in pregnant female cats without compromising fertility, lactation, and litters. The purpose of the present study is to report a case series of four non-pregnant, and four pregnant female cats with FAC treated conservatively with a combination of drugs and nutraceuticals. Case DetailsEight intact female cats were referred for the treatment of FAC between 2015 and 2020. Ages at admission ranged from 8 to 12 months (Table 1). Four cats were domestic shorthair (C1, C2, C5, and C8), two cats were Maine Coon (C3 and C6), and two were Persian (C4 and C7). None of the cats received exogenous progestins but had a history of recent heats. Four cats (C5, C6, C7, and C8) had been mated and were between the 25th and 32nd day of pregnancy at presentation. The mammary glands were bilaterally enlarged, and no milk secretion was detected. Skin ulceration, inflamed, and painful mammary glands were present in six cases (C1, C2, C3, C5, C7, and C8) (Fig. 1a and b). General signs (tachycardia, lethargy, and anorexia) were strongly related to these changes. The diagnosis of FAC was based on clinical symptoms. Fine-needle aspiration biopsy of the mammary tissue was performed to support the clinical diagnosis. The combination of glandular-epithelial tissue and mesenchymal cells and the absence of prevalent immune cell populations in the cytologic smears allowed to exclude malignant growth or mastitis. Ultrasound examination of the mammary gland and doppler was employed to evaluate the structure and vascularization of the enlarged gland. FAC presented mainly as a well-circumscribed solid mass of granular, slightly hyperechoic texture, with regularly delimited margins. There was a uniform distribution of vascularity. Anechoic areas were present in the parenchyma and outside the margins (Fig. 2). Owners gave their consent to conservative treatment to preserve fertility and the integrity of the mammary glands. Mastectomy was not performed in any cases. Non-pregnant cats (C1, C2, C3, and C4) were treated on two consecutive days with subcutaneous injections of 15 mg/kg Aglepristone (ALIZIN; Virbac, Carros, France). The treatment was continued weekly with a single injection until the resolution of signs. If signs of ulcers, inflammation, or necrosis were evident in at least one mammary gland, 12.5 mg/kg q 12 hours of amoxicillin / clavulanic acid tablet formulation (SYNULOX; Zoetis, Rome, Italy) and 0.1 mg/kg q 24 hours of meloxicam (MELOXORAL oral suspension 0,5/ml; Dechra Veterinary Products, Turin, Italy) for the first day, followed to 0.05 mg/kg q 24 hours was given for 5–6 days. Furthermore, an oral dietary supplement containing maltodextrin and bromelain (BROSPET; Aurora biofarma, Milan, Italy) was administered once a day for the treatment period. Ulcers were treated topically twice daily with a cream containing hypericum and neem extract (HYPERMIX; Rimos, Mirandola, MO, Italy). The enlarged mammary glands were daily massaged with an emollient gel based on Aloe vera (ALOPET GEL; linea Angel Ariel, Grancona, VI, Italy). Two of the four pregnant female cats were treated with the same schedule for the severe enlargement and ulceration of the mammary glands (C5) and early signs of fetal resorption, deduced by the slow heart rate and the increased echodensity of amniotic fluid (C6). After 1 week, they presented bloody vaginal discharge, and ultrasound revealed four placental remnants in a cat (C6) (Fig. 3). Cloprostenol (ESTRUMATE; MSD Animal Health, Segrate, MI, Italy) at the dosage of 1.5 mcg/kg was given for three consecutive days to facilitate uterine emptying. Two pregnant female cats (C7 and C8) were treated with the schedule less the aglepristone drug to preserve the litters. In all the cases studied, after 2–3 weeks, the mammary gland reduced in size, and no ulcers or necrotic areas were detected, and after 4–5 weeks, the lesion was not more recognizable. At term, pregnant queens C7 and C8 delivered four and three kittens, which were normally nursed and weaned after 40 days (Fig. 1c). The case series is summarized in Table 1. A 1-year follow-up reveals no recrudescences of FAC in treated animals. Table 1. Summary of the clinical findings in the case series.
Fig. 1. (a) Case C1. Severe FAC with ulcers and painful glands. Resolution after 2–3 weeks with the proposed combination of drugs and nutraceuticals. (b) Case C7. A pregnant Persian female cat with enlarged mammary glands (FAC) and inflamed skin. 21 days after treatment note the mammary gland involution. (c) Case C8. A 1-years-old domestic shorthair female cat, exhibiting FAC with ulcers during pregnancy, treated without aglepristone to preserve litters.
Fig. 2. Case C2. Ultrasound image of FAC revealed a solid pattern with a small cystic area and abundant oedema in the perimammary region.
Fig. 3. Case C6. A pregnant 1-years-old Maine Coon cat with FAC presenting placental remnants at ultrasound after the treatment with aglepristone. DiscussionThe reported cases were affected by the classical form of spontaneous FAC. They were all young cats with a history of no progestin treatment. The mammary glands were symmetrically enlarged, and, in the last instance they were responsive to therapy. Progestin treatments are sometimes associated with unresponsive forms of FAC in female and even in male cats (Görlinger et al., 2002; de Melo et al., 2020). Young animals are more affected for an unknown reason (Görlinger et al., 2002), perhaps for the fact that they present an increased ratio of spontaneous ovulation (Gudermuth et al., 1997). FAC is a rapid growth of the mammary gland as an exaggerated answer of the first progesterone expositions. The first goal of the therapeutic approach should focus on the removal of the progesterone. Aglepristone is a progesterone receptor blocker, and the result of this case series confirms that it is the first-line drug to treat FAC (Görlinger et al., 2002), mainly in non-pregnant and progestin-treated cats. In our experience, ulcers, necrosis, and mastitis are the main risk of FAC and affect the complete involution of the gland also after therapy. In these cases, partial or total mastectomy may be considered (Payan-Carreira, 2013) with loss of the reproductive value of the cat. This case series suggested that adjuvant therapy may facilitate involution, reducing oedema, infection, and necrotic changes. Despite the low number of cases of pregnant cats with effective resolution and the lack of a control group or experimental design, the proposed therapeutical approach has been possible to preserve the integrity of the mammary gland without the necessity of a mastectomy. Broad-spectrum antimicrobial treatment and nonsteroidal anti-inflammatory drugs may help treat infected, inflamed, and painful mammary glands (Payan-Carreira, 2013). The frequent occurrence of oedema suggested the adjuvant use of a dietary supplement containing maltodextrin and bromelain. The substances reduce oedema, bruising, pain, and healing time following trauma or surgical procedures (MacKay and Miller, 2003). A topic medication of ulcers in FAC with neem and hypericum was applied for the high antioxidant, anti-inflammatory, and antimicrobial activity (Wölfle et al., 2014). Finally, energic massage with emollient creams was administered to facilitate mammary circulation and give the cat relief. The choice of a topical application of aloe is supported by its anti-inflammatory and anti-oedema pharmacological property and the presence of angiogenic factors (Drudi et al., 2018). The maintenance of pregnancy in the cat also requires the presence of progesterone. Consequently, the cats with FAC that are pregnant abort after treatment with aglepristone (Görlinger et al., 2002). There is some evidence that the drug does not work well in cats as an abortive agent, not capable of emptying the uterus. Endometritis and retained placenta or fetuses have been reported (Görlinger et al., 2002; Fieni et al., 2006; Georgiev and Wehrend, 2006). The use of an ecbolic as prostaglandin is then recommended in association (Fieni et al., 2006). In two pregnant cases with FAC, the schedule was modified to preserve litters eliminating the aglepristone and exploiting the normal decline of progesterone at the end of pregnancy. After delivery, FAC may evolve in mastitis (Burstyn, 2010; Payan-Carreira, 2013). Kittens have been reported to be unable to nurse satisfactorily with offspring death over a short time period (Payan-Carreira, 2013). In this series, the two pregnant cases normally nursed and weaned kittens, despite the presence of a severe FAC with necrotic changes at presentation. Considering the similar time of recovery in the reported cases, it is possible to hypothesize that, in non-pregnant cats, the decline of progesterone after pseudopregnant cats may act in the same way and aglepristone, in some specific cases, could be not administered. These findings and considerations on FAC certainly require further studies. AcknowledgmentsThe research was partially supported by FFABR Unime grants. Conflict of interestThe authors declare that there is no conflict of interest. Authors contributionsConceptualization: G.M., F.P.; methodology: F.P., G.G., V.L.; writing—original draft preparation: S.D.G., G.M.; writing—review and editing: M.P., A.S.; funding acquisition: G.M., A.S., M.P. All authors have read and agreed to the published version of the manuscript. ReferencesAllen, H.L. 1973. Feline mammary hypertrophy. Vet. Pathol. 10, 501–508. Burstyn, U. 2010. Management of mastitis and abscessation of mammary glands secondary to fibroadenomatous hyperplasia in a primiparturient cat. J. Am. Vet. Med. Assoc. 236, 326–329. de Melo, E.H., Câmara, D.R., Notomi, M.K., Jabour, F.F., Garrido, R.A., Nogueira, A.C., Júnior, J.C. and de Souza, F.W. 2021 Effectiveness of ovariohysterectomy on feline mammary fibroepithelial hyperplasia treatment. J. Feline Med. Surg. 23, 351–356. Drudi, D., Tinto, D., Ferranti, D., Fiorelli, F., Dal Pozzo, M. and Capitani, O. 2018. Aloe barbadensis miller versus silver sulfadiazine creams for wound healing by secondary intention in dogs and cats: a randomized controlled study. Res. Vet. Sci. 117, 1–9. Fieni, F., Martal, J., Marnet, P.G., Siliart, B. and Guittot, F. 2006. Clinical, biological and hormonal study of mid-pregnancy termination in cats with aglepristone. Theriogenology 66, 1721–1728. Georgiev, P. and Wehrend, A. 2006. Mid-gestation pregnancy termination by the progesterone antagonist aglepristone in queens. Theriogenology 65, 1401–1406. Görlinger, S., Kooistra, H.S., van den Broek, A. and Okkens, A.C. 2002. Treatment of fibroadenomatous hyperplasia in cats with aglepristone. J. Vet. Intern. Med. 16, 710–713. Gudermuth, D.F., Newton, L., Daels, P. and Concannon, P. 1997. Incidence of spontaneous ovulation in young, group-housed cats based on serum and fecal concentrations of progesterone. J. Reprod. Fertil. Suppl. 51, 177–184. Hayden, D.W., Barnes, D.M. and Johnson, K.H. 1989. Morphologic changes in the mammary gland of megestrol acetate-treated and untreated cats: a retrospective study. Vet. Pathol. 26, 104–113. Loretti, A.P., Ilha, M.R.S., Breitsameter, I. and Faraco, C.S. 2004. Clinical and pathological study of feline mammary fibroadenomatous change associated with depot medroxyprogesterone acetate therapy. Arq. Bras. Med. Vet. Zootec. 56, 270–274. MacKay, D. and Miller, A.L. 2003. Nutritional support for wound healing. Altern. Med. Rev. 8, 359–377. Martín De Las Mulas, J., Millán, Y., Bautista, M.J., Pérez, J. and Carrasco, L. 2000. Oestrogen and progesterone receptors in feline fibroadenomatous change: an immunohistochemical study. Res. Vet. Sci. 68, 15–21. Mol, J.A., van Garderen, E., Rutteman, G.R. and Rijnberk, A. 1996. New insights in the molecular mechanism of progestin-induced proliferation of mammary epithelium: induction of the local biosynthesis of growth hormone (GH) in the mammary glands of dogs, cats and humans. J. Steroid. Biochem. Mol. Biol. 57, 67–71. Payan-Carreira, R. 2013. Feline mammary fibroepithelial hyperplasia: a clinical approach. In Ed., Payan-Carreira, London, UK: IntechOpen. Avaialbe via https://www.intechopen.com/books/insights-from-veterinary-medicine/feline-mammary-fibroepithelial-hyperplasia-a-clinical-approach Vitasek, R. and Dendisova, H. 2006. Treatment of feline mammary fibroepithelial hyperplasia following a single injection of proligestone. Acta. Vet. Brno. 75, 295–297. Wehrend, A., Hospes, R. and Gruber, A.D. 2001. Treatment of feline mammary fibroadenomatous hyperplasia with a progesterone-antagonist. Vet. Rec. 148, 346–347. Wölfle, U., Seelinger, G. and Schempp, C.M. 2014. Topical application of St. John's wort (Hypericum perforatum). Planta. Med. 80, 109–120. Zappulli, V., Peña, L., Rasotto, R. Goldschmidt, M., Gama, A., Scruggs, J. and Kiupel M. 2019. Mammary tumors. In Surgical pathology of tumors of domestic animals. Ed., Kiupel M, Washington, DC: Davis-Thompson DVM Foundation, pp: 206–208. | ||
| How to Cite this Article |
| Pubmed Style Marino G, Pugliese M, Pecchia F, Garufi G, Lupo V, Giorgio SD, Sfacteria A. Conservative treatments for feline fibroadenomatous changes of the mammary gland. Open Vet. J.. 2021; 11(4): 680-685. doi:10.5455/OVJ.2021.v11.i4.19 Web Style Marino G, Pugliese M, Pecchia F, Garufi G, Lupo V, Giorgio SD, Sfacteria A. Conservative treatments for feline fibroadenomatous changes of the mammary gland. https://www.openveterinaryjournal.com/?mno=97597 [Access: January 25, 2026]. doi:10.5455/OVJ.2021.v11.i4.19 AMA (American Medical Association) Style Marino G, Pugliese M, Pecchia F, Garufi G, Lupo V, Giorgio SD, Sfacteria A. Conservative treatments for feline fibroadenomatous changes of the mammary gland. Open Vet. J.. 2021; 11(4): 680-685. doi:10.5455/OVJ.2021.v11.i4.19 Vancouver/ICMJE Style Marino G, Pugliese M, Pecchia F, Garufi G, Lupo V, Giorgio SD, Sfacteria A. Conservative treatments for feline fibroadenomatous changes of the mammary gland. Open Vet. J.. (2021), [cited January 25, 2026]; 11(4): 680-685. doi:10.5455/OVJ.2021.v11.i4.19 Harvard Style Marino, G., Pugliese, . M., Pecchia, . F., Garufi, . G., Lupo, . V., Giorgio, . S. D. & Sfacteria, . A. (2021) Conservative treatments for feline fibroadenomatous changes of the mammary gland. Open Vet. J., 11 (4), 680-685. doi:10.5455/OVJ.2021.v11.i4.19 Turabian Style Marino, Gabriele, Michela Pugliese, Fabiana Pecchia, Giuseppe Garufi, Vincenzo Lupo, Stefania Di Giorgio, and Alessandra Sfacteria. 2021. Conservative treatments for feline fibroadenomatous changes of the mammary gland. Open Veterinary Journal, 11 (4), 680-685. doi:10.5455/OVJ.2021.v11.i4.19 Chicago Style Marino, Gabriele, Michela Pugliese, Fabiana Pecchia, Giuseppe Garufi, Vincenzo Lupo, Stefania Di Giorgio, and Alessandra Sfacteria. "Conservative treatments for feline fibroadenomatous changes of the mammary gland." Open Veterinary Journal 11 (2021), 680-685. doi:10.5455/OVJ.2021.v11.i4.19 MLA (The Modern Language Association) Style Marino, Gabriele, Michela Pugliese, Fabiana Pecchia, Giuseppe Garufi, Vincenzo Lupo, Stefania Di Giorgio, and Alessandra Sfacteria. "Conservative treatments for feline fibroadenomatous changes of the mammary gland." Open Veterinary Journal 11.4 (2021), 680-685. Print. doi:10.5455/OVJ.2021.v11.i4.19 APA (American Psychological Association) Style Marino, G., Pugliese, . M., Pecchia, . F., Garufi, . G., Lupo, . V., Giorgio, . S. D. & Sfacteria, . A. (2021) Conservative treatments for feline fibroadenomatous changes of the mammary gland. Open Veterinary Journal, 11 (4), 680-685. doi:10.5455/OVJ.2021.v11.i4.19 |