| Research Article | ||
Open Vet J. 2023; 13(6): 677-683 Open Veterinary Journal, (2023), Vol. 13(6): 677–683 Original Research Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 catsDeborah De Bastiani1*, Vincenzo Montinaro2, Erica Cipolla2, Roberto Bussadori1, Guido Pisani3 and Filippo Cinti41Clinica Veterinaria Gran Sasso, Milano, Italy 2Clinica Veterinaria Malpensa—AniCura, Samarate, Italy 3Centro Veterinario Luni Mare, Luni, Italy 4Clinica Veterinaria Privata San Marco—Viale dell'Industria, Veggiano, Italy *Corresponding Author: Deborah De Bastiani. Clinica Veterinaria Gran Sasso, Milano, Italy. Email: deborah.debastiani [at] hotmail.com Submitted: 06/01/2023 Accepted: 07/05/2023 Published: 01/06/2023 © 2023 Open Veterinary Journal
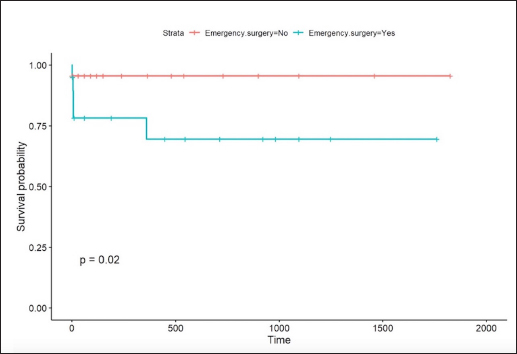
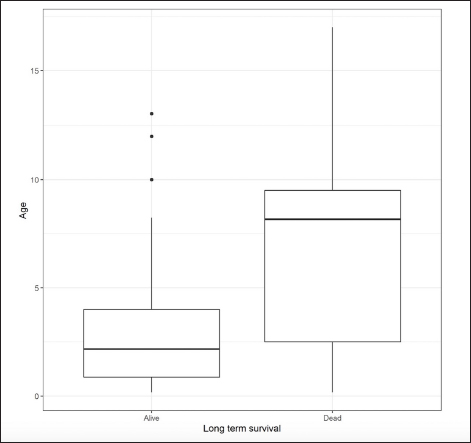
AbstractBackground: Diaphragmatic herniorraphy is the treatment of choice for traumatic diaphragmatic hernia (TDH). Several methods have been described for the removal of residual air and fluid during and after surgery, such as the insertion of chest drains, intercostal thoracentesis, and transdiaphragmatic thoracentesis. However, there are no indications regarding the most useful technique and the impact that choice of technique could have in the immediate postoperative period. Aim: To evaluate the development of complications and outcomes associated with the use of intraoperative transdiaphragmatic thoracentesis in cats undergoing diaphragmatic herniorrhaphy for TDH. Methods: Medical records of cats treated for acute and chronic TDH between 2010 and 2019 were reviewed. Cats were included if intraoperative pneumothorax was treated with transdiaphragmatic thoracentesis, without the use of intercostal chest drain. Outcome, intra- and post-operative complications were recorded. Results: Intraoperative and postoperative complication rates were 3.3% and 12.4%, respectively. Development of postoperative pneumothorax was associated with the presence of comorbidities (p=0.046). The overall survival rate was 93.3%. Long-term survival had a significant association with the presence of comorbidities (p =0.045), if the procedure was performed as an emergency (p =0.041) or in older cats (p =0.011). Conclusion: Intraoperative transdiaphragmatic thoracentesis could be considered an effective method for the removal of residual air after surgery for TDH, because it ensures a good outcome for the patient, with low development of complications, especially for uncomplicated cases. The presence of comorbidities, the need to perform a surgical procedure in emergency, and the age of the patient can be considered factors influencing the development of complications. Critical patient selection, based on assessment of potential risk factors for complications is warranted to understand which patient will benefit from thoracostomy tube placement. Keywords: Thoracic diaphragmatic hernia, Transdiaphragmatic thoracentesis, Trauma surgery. IntroductionDiaphragmatic hernia has a traumatic origin in 85% of cases. In most cases, trauma is caused by a motor vehicle accident; other causes include falls and penetrating wounds (Garson et al., 1980; Levine, 1987; Sullivan and Reid, 1990; Schmiedt et al., 2003; Minihan et al., 2004; Yool, 2014; Hunt and Johnson, 2018). Because of the nature of trauma, cats with traumatic diaphragmatic hernia (TDH) often present with multisystemic injuries (musculoskeletal lesions or other soft tissue injuries) (Hunt et al., 2018). In polytraumatized dogs and cats presenting with musculoskeletal trauma, 39% of the cases have also thoracic cavity injuries (Spackman et al., 1984; Tamas et al., 1985). Diaphragmatic herniorrhaphy is the treatment of choice for TDH. Reported survival rates range between 54% and 90% (Garson et al., 1980; Sullivan and Reid, 1990; Gibson et al., 2005; Yool, 2014; Legallet et al., 2017; Hunt and Johnson, 2018). Recent studies showed good survival rates in patients treated surgically within 24 hours (Gibson et al., 2005; Legallet et al., 2017), as opposed to patients that underwent surgery after 24 hours or more (Boudrieau and Muir, 1987; Sullivan and Reid, 1990). In the postoperative period, up to 50% of cases may develop complications (Schmiedt et al., 2003; Minihan et al., 2004; Hunt and Johnson, 2018). The most commonly reported are pneumothorax, hemothorax and other pleural effusions, re-expansion pulmonary edema, cardiac arrhythmias, shock, and organ failure from the initial trauma (Schmiedt et al., 2003; Minihan et al., 2004; Hunt and Johnson, 2018). These complications usually develop in the early postoperative period (within 24–48 hours) and could be life-threatening (Schmiedt et al., 2003; Minihan et al., 2004; Yool, 2014; Hunt and Johnson, 2018). To achieve better monitoring for the development of postoperative pneumothorax and pleural effusion, some authors advocate placing a thoracic drain until insignificant quantities of air and less than 2–3 ml/kg/day of fluid are accumulating (Garson et al., 1980; Hunt and Johnson, 2018). Thoracic drains are most commonly placed at an intercostal space between ribs 6 and 9. Some authors also describe the use of small gauge thoracic drains inserted through the diaphragm and allowed to exit through the laparotomy incision (Hunt and Johnson, 2018). However, another acceptable method to remove residual air is thoracentesis through the use of a catheter or needle (Wilson and Hayes, 1986; Sullivan and Reid, 1990; Bellenger et al., 1996; Gibson et al., 2005; Yool, 2014; Hunt and Johnson, 2018). In an early study, Sullivan and Reid (1990) suggested the use of intercostal thoracentesis (via a large catheter, a three-way tap, and a syringe) during surgery to remove residual air and fluid. No pneumothorax, nor pleural effusion was noted in the patients in the postoperative period (Sullivan and Reid, 1990). To date, however, there are no indications regarding the most useful technique to remove air during or after surgery and the impact that choice of technique could have in the immediate postoperative period. The objective of this study is to evaluate the use of intraoperative transdiaphragmatic thoracentesis for residual pneumothorax removal in cats subjected to diaphragmatic herniorrhaphy, assessing complication rates as well as survival. Our hypothesis was that intraoperative transdiaphragmatic thoracentesis can be performed with minimal postoperative complications in cats with TDH. Materials and MethodsStudy design and eligibility criteriaMedical data from four different institutions regarding cats with a diagnosis of TDH in the period from 2010 to 2019 were reviewed. Cats that underwent surgical treatment of TDH and transdiaphragmatic thoracentesis without the use of postoperative chest drain, with comprehensive clinical records and a follow-up period of at least 2 weeks were included in the study. Cats with incomplete data, use of chest drain, or congenital diaphragmatic hernia were excluded from this study. Data retrieved from the records included signalment, clinical history, cause of TDH, examination findings, duration of clinical signs, emergency treatment, time from admission to surgery, type of diaphragmatic tear, surgical treatment, and postoperative management. Diaphragmatic hernias were defined as acute if the symptoms had been present for less than 2 weeks. In the other cases, diaphragmatic hernias were considered chronic. Furthermore, for each patient, the presence of comorbidities associated with the trauma that had caused the TDH was recorded and was categorized as either the presence of musculoskeletal or soft tissue-related injuries. Postoperative radiographs were performed and residual pneumothorax was subjectively classified as absent, mild, moderate, or severe. The length of hospitalization and survival to discharge were also described. Short-term follow-up was defined as the period within 14 days from surgery, medium-term as the period beyond 14 days and within 3 months, while long-term follow-up was defined as the period beyond 3 months from surgery. Medium and long-term follow-ups were achieved by reviewing the medical records or by interviewing the owner. The outcome was considered poor if the patient died, good if the patient developed any type of complication related to the TDH, but recovered well, and excellent if in the whole follow-up period, the patient doesn’t develop any complication related to the TDH. The occurrence and intervals of any intraoperative and postoperative complication was recorded. Complications were classified as minor, if additional surgical treatment was not required to resolve, and as major, if additional surgical treatment was required to resolve or were life-threatening. Statistical analysisAll analyses were performed using R version 4.0.0. The data was initially explored through different methods depending on the nature of the outcome and predictor variables (age, sex, body weight, duration of clinical signs, abdominal ultrasound, emergency surgery, type of sutures, concomitant procedure, comorbidities, thoracocentesis, day of hospitalization). Contingency tables were then created in the case of categorical predictors. When the predictors were ordinal or continuous, boxplots were presented if the outcome was categorical, and a scatterplot if the outcome was interval. Tests of association between the outcome and the predictor variables were then assessed. Short-term, mid-term, and long-term survival, intraoperative complications, and postoperative complications were all categorical outcomes. When testing these outcomes against categorical predictor variables, a Fisher’s exact test was applied, and the p-value was reported. In the case where the predictor variables were interval or continuous, the median and inter-quartile range were reported and the data was fit to a logistic regression. The odds ratios were obtained from the model by back-transforming the coefficients and were reported alongside the 95% confidence intervals (95% CI) as well as the respective p-value. Time until discharge was an interval outcome and when testing for an association between this outcome and a binary predictor variable, the Mann-Whitney test was conducted. In the case when the predictor variable was categorical more than two levels the Kruskal-Wallis test was applied. For both of these cases, the p-value was reported. For continuous or interval predictors, Spearman’s correlation was reported. Ethical approvalThis work involved the use of non-experimental animals only (including owned or unowned animals and data from prospective or retrospective studies). Established internationally recognized high standards (“best practice”) of individual veterinary clinical patient care were followed. ResultsPopulation data, clinical presentation, and diagnostic investigationsNinety cats met the inclusion criteria and were included in the study. The most represented breed was Domestic Shorthair [89 (98.9%)]; one subject was a Maine Coon [1 (1.1%)]. There were 52 males (57.8%) [29/52 neutered (32.2%)] and 38 females (42.2%) [15/38 spayed (16.7%)]. The median age was 34 months (range 1.5–204) and the median body weight was 4 kg (range 0.4–6). The cause of trauma was available in the majority of the cases [66 (73%)]. In 57 cases (86%), cats were hit by a car. Other causes of TDH were: falls [6 (9%)], dog bites [2 (3%)], and maltreatment [1 (1.5%)]. In the remaining cases [24 (26.7%)], the possible cause of trauma was unknown, but the traumatic origin of the disease was presumed by the presence of other clinical signs (cutaneous lesions, bone fractures). The most common clinical sign at presentation was restrictive dyspnea [86 (95.5%)]. Other clinical signs included: lameness [8 (8.9%)], hematuria [4 (4.4%)], vomiting [2 (2.2%)], anorexia [2 (2.2%)], and lethargy [2 (2.2%)]. Seventeen cats [17/90 (19.9%)] presented with comorbidities, including musculoskeletal lesions (ribs, femur, pelvis, or jaw fracture), or soft tissue injuries (sharing injuries, abdominal wall lesions, and hematoma) caused by the inciting trauma. Clinical signs were present for a median period of 1 day (range: 2 hours–4 weeks). In 59/90 cases (65.6%) TDH was considered acute, while in 5/90 cases (5.6%) it was chronic. In the remaining 26 cases, there was no information recorded regarding the duration of clinical signs. Thoracic radiography was the main investigation used to diagnose TDH in all but one cat [89 (98.9%)]. In one case, the initial thoracic radiography was not able to detect TDH, which was instead diagnosed later during computed tomography. In 23 cases (25.6%) ultrasonography was used, combined with radiography, to make a diagnosis of TDH. All cats were triaged on arrival for initial emergency stabilization. Treatment included oxygen therapy, fluid therapy, and analgesics. Surgical procedure and intra-operative complicationsAfter medical stabilization, surgery was performed as soon as the patient was stable in 70 cats (77.8%). The median time from presentation to surgery was 24 hours (range 3–72 hours). For 20 cats (22.2%), emergency surgery was necessary due to the sudden worsening of their clinical condition despite medical treatment. The median time for medical stabilization was 6 hours (range 4–72 hours). The emergency cases included dyspnea not improving with oxygen therapy [4 (4.4%)], the presence of herniated dilated organs (particularly stomach and small intestine) [2 (2.2%)], and serious injuries of the abdominal wall [1 (1.1%)]. A standard midline celiotomy approach was used in all cases, without the need to extend the incision into a caudal sternotomy. The description of the diaphragmatic tear was available in 62/90 cases (68.9%). The diaphragmatic tear was circumferential in 34/62 cats (53.8%), radial in 18/62 cats (29%), or combined in the remaining 6/62 cats (9.6%). The side of hernia was registered in 64/90 cases (71.1%). The left-to-right distribution was quite uniform, with 26/64 (40.6%) cases having left-sided tears, 23/64 (35.9%) having right-sided tears, and 15/64 (23.4%) having bilateral tears. The most common herniated organ was the liver [73 (81.1%)]. Other herniated organs included: small intestine [39 (43.3%)], omentum [37 (41.1%)], spleen [28 (31.1%)], stomach [28 (31.1%)], gallbladder [7 (7.8%)], colon [3 (3.3%)], pancreas [2 (2.2%)], and kidney [1 (1.1%)]. After repositioning the herniated organs into the abdominal cavity, the thoracic cavity was explored through the traumatic tear in the diaphragm, to rule out the presence of pulmonary lesions caused by trauma or by tissue handling. Pulmonary lacerations were not seen in the visible lung lobes (caudal and accessory lobes) in any patient. Concomitant surgical procedures performed included removal of fractures ribs [1/90 (1.1%)], enterectomy [1/90 (1.1%)], caudectomy [1/90 (1.1%)], and wound treatment of a shearing injury [2/90 (2.2%)]. One patient [1/90 (1.1%)] had strong adhesions between a herniated kidney and the thoracic caudal vena cava but no additional surgical procedure was necessary. Three cats (37.5%) required fracture repair; this was done in a second surgical procedure when the patient was stable. The diaphragmatic tear was reconstructed using a suture pattern and material at the discretion of the primary surgeon. In all cases, residual air remaining in the thoracic cavity after the closure of the diaphragmatic tear was removed intraoperatively via a transdiaphragmatic thoracentesis using a butterfly needle attached to a three-way stopcock and a syringe of variable volume, until the intrathoracic negative pressure was reestablished. Intraoperative complications were registered in three patients [3/90; (3.3%)]. In one case, the cat had an acute cardiac arrest. A second cat developed severe respiratory difficulty at the end of the surgery, which required repeated thoracentesis via an intercostal approach to evacuate residual air. For the third cat with strong adherences between the kidney and the thoracic caudal vena cava, it was decided to leave the herniated kidney into the thoracic cavity. Postoperative complications and outcomesImmediate postoperative radiographies were performed in all the patients, but information regarding the results was available only for 42/89 cats (47.2%). In 37/42 (88%), pneumothorax was not present. In 4/42 (9.5%) residual pneumothorax was considered mild, while in 1/42 (2.4%) was considered moderate. Postoperative complications were registered in 11 of the 89 surviving cats (12.4%) (5 cases of pneumothorax, 4 pleural effusions, 1 diaphragmatic hernia recurrence, 1 death). Five cats [5/11 (45.5%)] developed pneumothorax. In one case, this complication was considered minor because it resolved spontaneously. In the four remaining cases, the complication was considered major. In two cats, an intercostal thoracentesis was necessary. One cat with a chronic TDH but no information about the presence of comorbidities and pulmonary disease, manifested mild pneumothorax and the end of the surgery and then developed a severe pneumothorax 2 hours later. This was managed by inserting a thoracostomy tube, but the cat died 4 days later because of the worsening of the pneumothorax. The last cat, which was presented for a recent dog bite that caused rib wall lacerations, had moderate pneumothorax on postoperative radiography. No pulmonary macroscopic lacerations were noted during surgery, so it was managed via two repeated intercostal thoracentesis. After 6 hours, dyspnea was presented again and pneumothorax was managed via an intercostal thoracentesis, but the cat died suddenly after the development of tension pneumothorax. The median time between the end of the surgery and the development of pneumothorax was 4 hours (range: 2–6 hours). A statistically significant association between the development of postoperative pneumothorax and the presence of comorbidities (p=0.046) was identified. Four cats [4/11 (36.4%)] developed pleural effusions. In one patient, this complication was considered as minor because it resolved spontaneously. In three cats, the complication was considered as major. In two cases, a thoracostomy tube was required. In particular, one cat showed an inflammatory effusion that diminished in the next few days. Another cat developed a pyothorax and died the following day. The third cat showed signs of pleural effusion 2 days after surgery. Thoracic radiography ruled out diaphragmatic hernia recurrence, but the cat was euthanized at the behest of the owner. The average duration between the end of the surgery and the development of pleural effusion was 4 days (range: 1–7 days). No statistically significant associations were found between any of the variables and the occurrence of pleural effusion. One cat [1/11 (9%)] died few hours after the end of the surgical procedure, due to severe re-expansion pulmonary edema. Another cat [1/11 (9%)] showed signs of dyspnea 2 days postoperatively and thoracic radiography showed diaphragmatic hernia recurrence. A second surgery was carried out and the cat recovered well. The overall mortality rate was 6.6% (6/90). Short-, mid-, and long-term follow-upThe median duration of hospitalization was 2 days (range: 1–6 days). A statistically significant difference between time until discharge and comorbidities (p=0.036) was assessed, with 11 cats (26.8%) without comorbidities being discharged within a day, while only 1 cat (4.3%) with comorbidities was discharged within a day. Short-term follow-up was available for all 84 surviving cats. There were no statistically significant associations between short-term survival and any of the variables measured. In the majority of cases [82/90 cases (91.1%)]. the cats recovered well and did not show problems related to the TDH. One cat [1/90 (1.1%)] was presented 4 days after the discharge for vomiting unrelated to the previous problem of TDH. Another cat [1/90 (1.1%)] was presented 6 days after the discharge for anorexia. It was euthanized because of the worsening of preexisting chronic kidney disease. On mid-term follow-up, no death was registered and all the patients recovered well. The median long-term follow-up was 24 months (range 1–60 months). For long-term survival, a statistically significant association was found with the need to perform emergency surgery (p=0.041), the presence of comorbidities (p=0.045), and the older age of the patient (p=0.011). The median age of the cats that survived was 2.2 years and those that died were 8.2 years. Furthermore, 5/30 (16.7%) of cats that had comorbidities did not survive in the long term, and only 2/60 (3.3%) cats that had no comorbidities died in the long term. Overall, the outcome was considered poor for 6/90 cats (6.6%), good for 7/90 (7.7%), and excellent for the remaining 77/90 (85.6%). DiscussionThe study reports the use of transdiaphragmatic thoracentesis after herniorrhaphy for TDH. The intraoperative and postoperative complications rates were 3.3% and 12.4%, respectively, while the overall survival rate was 93.3%, in line with the results reported in the literature (Garson et al., 1980; Sullivan and Reid, 1990; Gibson et al., 2005; Legallet et al., 2017). These results support accepting our hypothesis that intraoperative transdiaphragmatic thoracentesis could be considered an effective method because it ensures an excellent outcome for the majority of the patients, with low development of complications, especially in uncomplicated cases. The most common complication encountered in our study was postoperative pneumothorax [5/89 (5.6%)]. In particular, this complication was significantly associated with the presence of comorbidities, considered as both the presence of musculoskeletal lesions (ribs, femur, pelvis, or jaw fracture) and soft tissue injuries (sharing injuries, abdominal wall lesions, and hematoma). Nevertheless, our study showed that the majority of the patients that developed pneumothorax in the postoperative period were successfully managed via percutaneous thoracentesis. Three cats had additional thoracic pathology. There was one cat with strong adherences between herniated kidney and thoracic caudal vena cava, one with rib fractures and one with thoracic wall laceration secondary to a dog bite injury. Two of them developed pneumothorax in the postoperative period, but one of them died despite thoracentesis. This strongly suggested that pulmonary pathology such as a laceration was present but not identified during preoperative investigations or intraoperative assessment. Based on our findings, a comprehensive assessment of the patient must be carried out before surgery, in particular, to identify thoracic pathology to help guide decision-making regarding whether a thoracic drain is required or not. Unfortunately, data regarding postoperative radiographic evaluation was available for less than half of patients, so it is not possible to make any comment on its value for predicting postoperative complications. No association between the development of pleural effusion and the presence of comorbidities was found. The survival rate in our study was 93.3%, similar to the survival rates reported in the literature (Garson et al., 1980; Sullivan and Reid, 1990; Gibson et al., 2005; Legallet et al., 2017). In long-term survival, an association between mortality and the need to perform emergency surgery, the presence of comorbidities, and the older age of the patient were found (Figs. 1–3). A correlation between comorbidities and survival has been reported in previous studies (Schmiedt et al., 2003; Legallet et al., 2017). This relationship is likely due to the greater severity of the initial trauma and the subsequent inability of the animal to compensate for the additional stress caused by anesthesia and surgery, causing increasing mortality rates (Schmiedt et al., 2003; Legallet et al., 2017). The requirement for emergency surgery was associated with a reduced survival rate. In this study, we considered an emergency surgery to be one performed in a patient that was still unstable but not improving despite medical treatment. It is therefore unsurprising that these patients had a higher mortality rate. The correlation between age and long-term survival was also found by Schmiedt et al. (2003). Older cats could have subclinical conditions that make recovery from trauma, anesthesia, and surgery more difficult. The retrospective nature of this study means there are a number of limitations, not least the quality and completeness of the clinical records available for review. The multi-center setting of the study means that there was a lack of standardized protocols for medical and surgical management of the cases. The study lacks information about preoperative laboratory findings and imaging studies that could improve the identification of comorbidities (in particular, thoracic lesions). These are not only risk factors for complications in our study, they are also factors that may influence whether a thoracic drain is placed for postoperative management. Moreover, the low case number compromises statistical validity. A large number of prospective studies are warranted to evaluate how some factors, such as duration of TDH, preoperative laboratory findings and imaging studies could help identify risk factors for the development of complications in order to help the decision-making on the use of the best method to evacuate air after TDH treatment.
Fig. 1. Kaplan-Meier analysis shows how patient referred for emergency surgery has more postoperative complications and shorter survival.
Fig. 2. Kaplan-Meier analysis shows how comorbidities negatively influenced postoperative complications and survival.
Fig. 3. Spread of age across long-term survival. Age was one of the risk factors associated with long-term survival and complications. ConclusionIn keeping with previously published information (Wilson and Hayes, 1986; Sullivan and Reid, 1990; Bellenger et al., 1996; Gibson et al., 2005; Yool, 2014; Hunt and Johnson, 2018), intraoperative transdiaphragmatic thoracentesis can be considered a useful method to remove residual air from the thoracic cavity of cats undergoing diaphragmatic hernia repair provided the case is not complicated by thoracic pathology such as pulmonary laceration or hemothorax. A correct patient selection, which included an analysis of risk factors for the development of complications, is warranted. Conflict of interestThe authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Authors’ contributionDDB, VM, EC, RB, GP, FC conceived the ideas of the study; DDB wrote the manuscript; DDB, FC, VM were major contributors to writing the manuscript and all other authors commented on the manuscript; FC performed the analyses. ReferencesBellenger, C.R., Hunt, G.B., Goldsmid, S.E. and Pearson, M.R. 1996. Outcomes of thoracic surgery in dogs and cats. Aust. Vet. J. 74(1), 25–30. Boudrieau, R.J. and Muir, W.M. 1987. Pathophysiology of traumatic diaphragmatic hernia in dogs. Compend. Contin. Educ. Pract. Vet. 9, 379–385. Garson, H.L., Dodman, N.H. and Baker, G.J. 1980. Diaphragmatic hernia. Analysis of fifty-six cases in dogs and cats. J. Small Anim. Pract. 21(9), 469–481. Gibson, T.W., Brisson, B.A. and Sears, W. 2005. Perioperative survival rates after surgery for diaphragmatic hernia in dogs and cats: 92 cases (1990-2002). J. Am. Vet. Med. Assoc. 227(1), 105–109. Hunt, G.B. and Johnson, K.A. 2018. Diaphragmatic Hernias. In Veterinary surgery small animals expert consult. Eds., Tobias KM, and Johnston, SA. Elsevier Saunders, vol. 2. pp: 1592–1603. Legallet, C., Thieman Mankin, K. and Selmic, L.E. 2017. Prognostic indicators for perioperative survival after diaphragmatic herniorrhaphy in cats and dogs: 96 cases (2001-2013). BMC Vet. Res. 13(1), 16. Levine, S.H. 1987. Diaphragmatic hernia. Vet. Clin. North Am. Small Anim. Pract. 17(2), 411–430. Minihan, A.C., Berg, J. and Evans, K.L. 2004. Chronic diaphragmatic hernia in 34 dogs and 16 cats. J. Am. Anim. Hosp. Assoc. 40(1), 51–63. Schmiedt, C.W., Tobias, K.M. and Stevenson, M.A. 2003. Traumatic diaphragmatic hernia in cats: 34 cases (1991-2001). J. Am. Vet. Med. Assoc. 222(9), 1237–1240. Spackman, C.J.A., Caywood, D.D., Feeney, D.A. and Johnston, G.R. 1984. Thoracic wall and pulmonary trauma in dogs sustaining fractures as a result of motor vehicle accidents. J. Am. Vet. Med. Assoc. 185(9), 975–977. Sullivan, M. and Reid, J. 1990. Management of 60 cases of diaphragmatic rupture. J. Small Anim. Pract. 31, 425–430. Tamas, P.M., Paddleford, R.R. and Krahwinkel, D.J. Jr. 1985. Thoracic trauma in dogs and cats presented for limb fractures. J. Am. Anim. Hosp. Assoc. 21(2), 161–166. Wilson, G.P. 3rd and Hayes, H.M. Jr. 1986. Diaphragmatic hernia in the dog and cat: a 25-year overview. Semin. Vet. Med. Surg. Small Anim. 1(4), 318–326. Yool, D.A. 2014. Diaphragm. In Feline soft tissue and general surgery. Eds., Langley-Hobbs, S.J., Demetriou, J. and Ladlow, J. Saunders, pp: 521–530. | ||
| How to Cite this Article |
| Pubmed Style DD, VM, EC, RB, Pisani G, Cinti F. Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats. Open Vet J. 2023; 13(6): 677-683. doi:10.5455/OVJ.2023.v13.i6.1 Web Style DD, VM, EC, RB, Pisani G, Cinti F. Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats. https://www.openveterinaryjournal.com/?mno=133658 [Access: May 11, 2024]. doi:10.5455/OVJ.2023.v13.i6.1 AMA (American Medical Association) Style DD, VM, EC, RB, Pisani G, Cinti F. Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats. Open Vet J. 2023; 13(6): 677-683. doi:10.5455/OVJ.2023.v13.i6.1 Vancouver/ICMJE Style DD, VM, EC, RB, Pisani G, Cinti F. Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats. Open Vet J. (2023), [cited May 11, 2024]; 13(6): 677-683. doi:10.5455/OVJ.2023.v13.i6.1 Harvard Style , D. D., , . V. M., , . E. C., , . R. B., Pisani, . G. & Cinti, . F. (2023) Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats. Open Vet J, 13 (6), 677-683. doi:10.5455/OVJ.2023.v13.i6.1 Turabian Style , Deborah De-Bastiani, Vincenzo Montinaro, Erica Cipolla, Roberto Bussadori, Guido Pisani, and Filippo Cinti. 2023. Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats. Open Veterinary Journal, 13 (6), 677-683. doi:10.5455/OVJ.2023.v13.i6.1 Chicago Style , Deborah De-Bastiani, Vincenzo Montinaro, Erica Cipolla, Roberto Bussadori, Guido Pisani, and Filippo Cinti. "Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats." Open Veterinary Journal 13 (2023), 677-683. doi:10.5455/OVJ.2023.v13.i6.1 MLA (The Modern Language Association) Style , Deborah De-Bastiani, Vincenzo Montinaro, Erica Cipolla, Roberto Bussadori, Guido Pisani, and Filippo Cinti. "Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats." Open Veterinary Journal 13.6 (2023), 677-683. Print. doi:10.5455/OVJ.2023.v13.i6.1 APA (American Psychological Association) Style , D. D., , . V. M., , . E. C., , . R. B., Pisani, . G. & Cinti, . F. (2023) Complications and outcome of traumatic diaphragmatic hernia repair without post-operative chest drain: Retrospective study in 90 cats. Open Veterinary Journal, 13 (6), 677-683. doi:10.5455/OVJ.2023.v13.i6.1 |