| Case Report | ||
Open Vet J. 2023; 13(1): 114-118 Open Veterinary Journal, (2023), Vol. 13(1): 114–118 Case Report Use of a gum elastic bougie in a cat with severe upper airway stenosisKeiko Kato, Takaharu Itami*, Shidow Torisu, Toshikazu Sakai and Kazuto YamashitaDepartment of Small Animal Clinical Sciences, School of Veterinary Medicine, Rakuno Gakuen University, Ebetsu, Japan Submitted: 11/07/2022 Accepted: 05/12/2022 Published: 23/01/2023 *Corresponding Author: Takaharu Itami. Department of Small Animal Clinical Sciences, School of Veterinary Medicine, Rakuno Gakuen University, Ebetsu, Japan. Email: t-itami [at] rakuno.ac.jp © 2023 Open Veterinary Journal
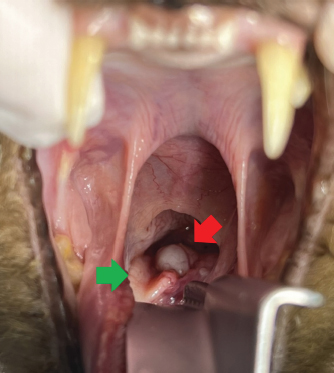
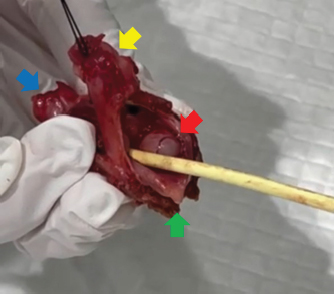
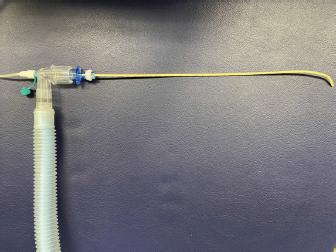
AbstractABSTRACT Background: Gum elastic bougie (GEB) is an airway management device for patients who are difficult to intubate and its use has been reported in human medicine. However, to our knowledge, no reports in veterinary medicine have described oxygenation using GEB. We describe a case in which GEB was used to maintain oxygenation in a cat with severe upper airway stenosis. Case Description: A 10-year-old neutered male domestic shorthair cat was diagnosed with a laryngeal tumor with severe upper airway stenosis. During anesthesia induction, the normal laryngeal structure could not be confirmed; orotracheal intubation was difficult, resulting in a “cannot intubate, cannot oxygenate” status. The GEB was inserted, making it possible to oxygenate the cat until a permanent tracheostoma could be created, but hypoventilation was noted. Conclusion: Although GEB are not useful for proper ventilation, they can be useful for temporary oxygenation in veterinary medicine when airway management is difficult. Keywords: Cat, Gum elastic bougie, Oxygenation, Tumor, Upper airway stenosis. IntroductionAirway management is an important part of general anesthesia. Orotracheal intubation is commonly performed for airway management in veterinary medicine, but veterinarians may occasionally be unable to visualize the larynx and insert the endotracheal tube into the trachea. Such situations characterized by the inability to oxygenate despite respiratory arrest are termed “cannot intubate, cannot oxygenate (CICO)” and represent an emergency that requires surgical intervention in human medicine. Respiratory complications, and more specifically airway obstruction, accounted for most of the cases of anesthesia-related mortality in studies conducted on cats (Brodbelt et al., 2008). Tumor-induced upper airway stenosis has the potential to cause CICO situations and result in complications such as hypoxemia and hypercapnia. The gum elastic bougie (GEB) is an airway management device for patients who are difficult to intubate, which is often used in human medicine in the UK (Latto et al., 2002). Having a thin, hollow, elastic structure, the GEB can be used as an endotracheal tube introducer or tube exchanger, and also allows for temporary oxygenation. However, to our knowledge, no reports in veterinary medicine have described oxygenation using GEB. We describe a case in which a cat with severe upper airway stenosis due to a tumor was able to maintain oxygenation using GEB. Case DetailsA 10-year-old neutered male domestic shorthair cat weighing 5.5 kg was diagnosed as having a laryngeal tumor. The owner first recognized changes in the cat’s voice, which was followed by aphonia 5 months before the first medical examination at a local veterinary hospital. The patient’s respiratory condition continued to worsen, and radiographs confirmed a tumor in the pharyngeal area. A naso-esophageal feeding tube was placed because of anorexia. The cat was referred to Rakuno Gakuen University Animal Medical Center (RGU-AMC) for diagnosis and treatment. Examinations performed at RGU-AMC showed that the cat’s general condition was poor with labored breathing, decreased activity, and somnolence. In addition, he presented with mouth-breathing and severe drooling (Fig. 1). Ultrasonography showed a mixed echogenic tumor, while complete blood cell count and serum biochemical examination analysis revealed mild thrombocytopenia and hyperphosphatemia. Due to the deterioration of the respiratory condition during the examination, the cat was placed in an oxygen cage. Emergency surgery with total laryngectomy, removal of the tumor, tracheostomy, and percutaneous endoscopic gastrostomy was indicated. Before anesthesia induction, the surgeons prepared for emergency tracheotomy if orotracheal intubation proved impossible. Anesthesia was induced using alfaxalone (Alfaxan; Meiji Seika Pharma Co., Ltd. Tokyo, Japan) without premedication. Alfaxalone 5 mg/kg was diluted to 5 ml using normal saline (i.e., 1 mg/kg/ml) and intravenously administered through the cephalic venous catheter at the rate of approximately 0.5 mg/kg/minute. During administration, an Elizabethan collar (Animal Necker, side CAT; Menix Co. Ltd., Tokyo, Japan) was covered with a shower cap (Shower cap; Sanyo Burashi Co., Ltd. Ehime, Japan) to create a temporary oxygen hood and oxygen was delivered into the hood (5 l/minutes) to prevent the accumulation of exhaled carbon dioxide. The laryngeal tumor was recognized visually (Fig. 2), and endotracheal tube (Portex endotracheal tube, internal diameter [ID]: 3 mm, outer diameter [OD]: 4.2 mm; Smiths Medical Japan Ltd., Tokyo, Japan) insertion was attempted but was not possible. Percutaneous oxygen saturation (SpO2) could not be measured during induction of anesthesia due to the cat’s black and gray coat color, but the visible mucous membranes showed cyanosis, and a CICO status was confirmed. Therefore, a GEB was inserted (Airway Exchange Catheter, 8 Fr; Cook Medical Japan G.K., Tokyo, Japan) into the trachea (Fig. 3). The GEB could be inserted within 2 minutes from a small gap beside the laryngeal tumor, through which the cat could be oxygenated until tracheotomy. The SpO2 could be maintained at 99% or higher by connecting the GEB with a circle anesthetic rebreathing system (Isepo; ACOMA Medical Industry Co., Ltd., Tokyo, Japan) (Fig. 4). However, severe hypoventilation with an end-tidal carbon dioxide pressure (PetCO2) value exceeding 100 mmHg was observed immediately after connecting to the anesthesia circuit. When manual ventilation was performed to lengthen the expiratory time (inspiratory and expiratory ratio=1:4), the PetCO2 gradually decreased to approximately 50 mmHg. Subsequently, the GEB was carefully maintained, and anesthesia was maintained with 1% sevoflurane in oxygen (2 l/minutes) delivered via an anesthetic machine with an out-of-circuit vaporizer. After intravascular administration of fentanyl 2.5 µg/kg (Fentanyl injection “Daiichi Sankyo”; Daiichi Sankyo Propharma Co., Ltd. Tokyo, Japan), permanent tracheostomy was performed and used for insertion of the endotracheal tube (ID: 3.5 mm/OD: 4.9 mm), after which the GEB was removed.
Fig. 1. The cat was shown opening mouth to breath and severe saliva was observed in the oxygen cage.
Fig. 2. A rigid laryngeal tumor was identified and the endotracheal tube could not be intubated into the trachea. Green arrow: epiglottis, Red arrow: Laryngeal tumor.
Fig. 3. The figure of inserted GEB with the excised laryngeal tumor. The GEB could be inserted from a small gap beside the laryngeal tumor. Blue arrow: trachea, Green arrow: epiglottis, Red arrow: laryngeal tumor, Yellow arrow: esophagus. After the tracheostomy, computed tomography was performed to examine the tumor spread and metastasis. Fentanyl 2 µg/kg/hours, ketamine 0.6 mg/kg/hours (Ketamine Inj. 5% “Fujita”; Fujita Pharmaceutical. Co., Ltd., Tokyo, Japan), and remifentanil 20 µg/kg/hours (Remifentanil for intravenous injection “Daiichi Sankyo”; Daiichi Sankyo Propharma Co., Ltd. Tokyo, Japan) were administered in a continuous rate infusion through the cephalic venous catheter as analgesia. During total laryngectomy and percutaneous endoscopic gastrostomy, bradycardia (heart rate: 94 beats/minutes) and hypotension (mean arterial pressure <60 mmHg) were observed. For improvement of bradycardia and hypotension, intravenous atropine 20 µg/kg (atropine sulfate injection; Fuso Pharmaceutical Industries Ltd., Osaka, Japan) was administered twice with dobutamine constant rate infusion at 3 µg/kg/minutes (Dobutrex; Kyowa Pharmaceutical Industry Co., Ltd. Osaka, Japan). After the surgery, sevoflurane was discontinued. The total anesthesia time was 246 minutes. When the eyelid reflex and jaw muscle tension returned, the endotracheal tube inserted into the tracheostomy was removed. After the removal of the endotracheal tube, the larynx was found to be narrowed by the tumor. Tracheal tube intubation was not possible for the resected laryngeal tumor, and hence only GEB could be inserted. After extubation, the cat was calm, and SpO2=100% could be maintained by 30% oxygen inhalation and 60%~80% humidity in the oxygen cage. The cat was discharged 4 days later. Pathology revealed that the resected laryngeal tumor was a squamous cell carcinoma. After discharge, the cat underwent radiation therapy 4 times and died approximately 2 months after the permanent tracheostomy because of a mucous plug, even though his general condition was good.
Fig. 4. The GEB can be connected to a circle anesthesia rebreathing system and can perform oxygenation from its tip. DiscussionWe report the findings for a cat with severe upper airway stenosis and difficult airway management that showed a CICO status. The laryngeal tumor prevented the insertion of the endotracheal tube, but a GEB could be inserted into the trachea through a small gap beside the tumor, from which oxygenation could be performed before a permanent tracheostomy could be completed. Thus, temporary oxygenation using the GEB can be considered useful for cats with severe upper airway stenosis caused by a laryngeal tumor. The GEB, which was developed in the UK and first reported in the early 1970s, is a commonly used device in human medicine in the UK (Henderson, 2003). However, reports describing the use of GEBs in veterinary medicine are limited. GEBs are similar to stylets and are mainly used for insertion into the tracheal tube and as a guide for intubation. However, GEBs have greater flexibility and malleability than stylets. Moreover, a hole in the tip of the bougie can be used for oxygenation by connecting it to an anesthesia circuit. This apparatus is thought to be more useful than stylets because oxygenation can be achieved by inserting a bougie in CICO cases (Gataure et al., 1996). The narrowest available tracheal tube has an ID of 2.0 mm and an OD of 2.9 mm, which unfortunately was not available at our institution at this time. Thin straight tubes are also inconvenient because they are prone to clogging due to bending. On the contrary, the ID of GEBs has not been clarified. However, a GEB has an OD of 2.667 mm (8 Fr.) and is narrower than the tracheal tube as mentioned above, allowing temporary oxygenation and ventilation. In the present case, the cat could only be airway-managed and oxygenated (SpO2 >99%) using the GEB until tracheotomy. In veterinary medicine, an emergency tracheotomy may be the first choice in cases like the present case because the devices and guidelines for difficult airway management have not improved at the same pace as in human medicine. Since a permanent tracheostomy was planned for this cat as well, an emergency tracheotomy would be the first choice, but the GEB allowed oxygenation to be achieved. The prognosis for a permanent tracheostomy in cats is known to be very poor, due to sudden death from mucous plugs and the progression of neoplasia (Stepnik et al., 2009). In addition, careful skin and trachea incision is required to reduce complications, which is difficult in emergency situations. Therefore, a permanent tracheostomy was planned in this case while maintaining as much oxygenation as possible. Furthermore, tracheotomy is considered to be a relatively tolerable procedure (Carroll, 1999); nevertheless, weak analgesics and light depth of anesthesia should be avoided from the perspective of animal welfare. While administration of an appropriate depth of anesthesia and analgesia is desirable before performing a tracheostomy, sometimes it is not possible in an emergency situation. The insertion of GEB in this cat allowed tracheotomy after the administration of sevoflurane and fentanyl. In this cat, SpO2 could not be measured during induction of anesthesia, but the cat showed obvious cyanosis. Hypoxemia is defined as a partial pressure of oxygen in arterial blood (PaO2) <60 mmHg or SpO2 <90% (Gaynor et al., 1999). Hypoxemia is caused by many factors, including airway obstruction (Wilson and Shih, 2015). Though it can affect many organs such as the kidney, eyes, and brain damage caused by hypoxic encephalopathy is very common and can result in a coma (Duncalf and Weitzner, 1963; Schmiedt et al., 2016; Brown et al., 2019; Dunn and Isaacs, 2020; Spencer et al., 2021). Fortunately, no neurological symptoms were observed after recovery from anesthesia in this case. However, according to the American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway in human medicine, CICO is also an indication for emergency tracheotomy; thus, hypoxemia with the bougie in place should not be prolonged (Apfelbaum et al., 2022). Hypercapnia is defined as a partial pressure of carbon dioxide in arterial blood (PaCO2) or PetCO2 >55 mmHg (Gaynor et al., 1999). Hypercapnia is caused by many factors, including airway obstruction (Haskins, 2015), and persistent hypercapnia causes respiratory acidosis and increased intracranial pressure (Itami et al., 2019). In addition, hypercapnia and hypoxemia cause reductions in cardiac output and blood pressure, delayed recovery, and inadequate tissue perfusion (McDonell and Kerr, 2015). This cat showed PetCO2 over 100 mmHg at the time of GEB insertion. The inner diameter of the GEB was very small, and a high airway resistance was thought to be the cause of hypoventilation. When the airway resistance is high, if the exhalation time is short, exhalation is not possible and the alveolar ventilation becomes low; moreover, the circulation is suppressed by the auto-positive end-expiratory pressure (auto-PEEP). In this cat, PetCO2 was gradually reduced by trying to secure ventilation by prolonging the exhalation time, and no circulatory suppression was observed until the time of tracheostomy. Thus, airway management with the GEB provides minimal ventilation and oxygenation and should only be used on a temporary basis. Proper use of GEB for airway management requires further investigation. This case had some limitations. Arterial blood gas analysis was not implemented before and after insertion of the GEB because the cat showed severe dyspnea, and it was not technically possible to collect arterial blood immediately after inserting the bougie. Therefore, respiratory parameters such as PaO2 and PaCO2 could not be accurately evaluated. In conclusion, when managing anesthesia for suspected upper airway stenosis caused by conditions such as a laryngeal tumor, an emergency tracheotomy and various oxygenation devices should be prepared to avoid CICO before induction of anesthesia. In conclusion, a GEB has the potential to be one of the oxygenation devices useful for difficult airway management in veterinary medicine. Conflict of interestThe authors declare that there is no conflict of interest. Author contributionsKato, K. and Itami, T.: Anesthesia management and manuscript drafting, and approval of the final manuscript. Torisu, S. and Sakai, T.: Case evaluation, surgery, and follow-up. Yamashita, K.: Manuscript supervision. ReferencesApfelbaum, J.L., Hagberg, C.A., Connis, R.T., Abdelmalak, B.B., Agarkar, M., Dutton, R.P., Fiadjoe, J.E., Greif, R., Klock, P.A., Mercier, D., Myatra, S.N., O’Sullivan, E.P., Rosenblatt, W.H., Sorbello, M. and Tung, A. 2022. 2022 American society of anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology 136, 31–81. Brodbelt, D.C., Blissitt, K.J., Hammond, R.A., Neath, P.J., Young, L.E., Pfeiffer, D.U. and Wood, J.L. 2008. The risk of death: the confidential enquiry into perioperative small animal fatalities. Vet. Anaesth. Analg. 35, 365–373. Brown, C.A., Rissi, D.R., Dickerson, V.M., Davis, A.M., Brown, S.A. and Schmiedt, C.W. 2019. Chronic renal changes after a single ischemic event in an experimental model of feline chronic kidney disease. Vet. Pathol. 56, 536–543. Carroll, G.L. 1999. Analgesics and pain. Vet. Clin. North. Am. Small. Anim. Pract. 29, 701–717. Duncalf, D. and Weitzner, S.W. 1963. The influence of ventilation and hypercapnia on intraocular pressure during anesthesia. Anesth. Analg. 42, 232–246. Dunn, J.F. and Isaacs, A.M. 2020. The impact of hypoxia on blood-brain, blood-CSF, and CSF-brain barriers. J. Appl. Physiol. (1985). 131, 977–985. Gataure, P.S., Vaughan, R.S. and Latto, I.P. 1996. Simulated difficult intubation. Comparison of the gum elastic bougie and the stylet. Anaesthesia 51, 935–938. Gaynor, J.S., Dunlop, C.I., Wagner, A.E., Wertz, E.M., Golden, A.E. and Demme, W.C. 1999. Complications and mortality associated with anesthesia in dogs and cats. J. Am. Anim. Hosp. Assoc. 35, 13–17. Haskins, S.C. 2015. Monitoring anesthetized patients pulmonary system. In Lumb and Jones veterinary anesthesia and analgesia, 5th ed. Eds., Grimm, K.A. and Lamont, L.A. Hoboken, N.J: WILEY Blackwell, pp: 86–113. Henderson, J.J. 2003. Development of the ’gum-elastic bougie’. Anaesthesia 58, 103–104. Itami, T., Hanazono, K., Oyama, N., Sano, T., Makita, K. and Yamashita, K. 2019. Cardiovascular effects of intravenous colforsin in normal and acute respiratory acidosis canine models: a dose-response study. PLoS One 14, e0213414. Latto, I.P., Stacey, M., Mecklenburgh, J. and Vaughan, R.S. 2002. Survey of the use of the gum elastic bougie in clinical practice. Anaesthesia 57, 379–384. McDonell, W.N. and Kerr, C.L. 2015. Physiology, pathophysiology, and anesthetic management of patients with respiratory disease. In Lumb and Jones veterinary anesthesia and analgesia, 5th ed. Eds., Grimm, K.A. and Lamont, L.A. Hoboken, N.J: WILEY Blackwell, pp: 513–555. Schmiedt, C.W., Brainard, B.M., Hinson, W., Brown, S.A. and Brown, C.A. 2016. Unilateral renal ischemia as a model of acute kidney injury and renal fibrosis in cats. Vet. Pathol. 53, 87–101. Spencer, S., Wheeler-Jones, C. and Elliott, J. 2021. Hypoxia and chronic kidney disease: possible mechanisms, therapeutic targets, and relevance to cats. Vet. J. 274, 105714. Stepnik, M.W., Mehl, M.L., Hardie, E.M., Kass, P.H., Reimer, S.B., Campbell, B.G., Mison, M.B., Schmiedt, C.W., Gregory, C.R. and Hobson, H.P. 2009. Outcome of permanent tracheostomy for treatment of upper airway obstruction in cats: 21 cases (1990-2007). J. Am. Vet. Med. Assoc. 234, 638–643. Wilson, D.V. and Shih, A.C. 2015. Anesthetic emergencies and resuscitation respiratory system. In Lumb and Jones veterinary anesthesia and analgesia, 5th ed. Eds., Grimm, K.A. and Lamont, L.A. Hoboken, N.J: WILEY Blackwell, pp: 114–129. | ||
| How to Cite this Article |
| Pubmed Style Kato K, Itami T, Torisu S, Sakai T, Yamashita K. Use of a gum elastic bougie in a cat with severe upper airway stenosis. Open Vet J. 2023; 13(1): 114-118. doi:10.5455/OVJ.2023.v13.i1.12 Web Style Kato K, Itami T, Torisu S, Sakai T, Yamashita K. Use of a gum elastic bougie in a cat with severe upper airway stenosis. https://www.openveterinaryjournal.com/?mno=56656 [Access: July 27, 2024]. doi:10.5455/OVJ.2023.v13.i1.12 AMA (American Medical Association) Style Kato K, Itami T, Torisu S, Sakai T, Yamashita K. Use of a gum elastic bougie in a cat with severe upper airway stenosis. Open Vet J. 2023; 13(1): 114-118. doi:10.5455/OVJ.2023.v13.i1.12 Vancouver/ICMJE Style Kato K, Itami T, Torisu S, Sakai T, Yamashita K. Use of a gum elastic bougie in a cat with severe upper airway stenosis. Open Vet J. (2023), [cited July 27, 2024]; 13(1): 114-118. doi:10.5455/OVJ.2023.v13.i1.12 Harvard Style Kato, K., Itami, . T., Torisu, . S., Sakai, . T. & Yamashita, . K. (2023) Use of a gum elastic bougie in a cat with severe upper airway stenosis. Open Vet J, 13 (1), 114-118. doi:10.5455/OVJ.2023.v13.i1.12 Turabian Style Kato, Keiko, Takaharu Itami, Shidow Torisu, Toshikazu Sakai, and Kazuto Yamashita. 2023. Use of a gum elastic bougie in a cat with severe upper airway stenosis. Open Veterinary Journal, 13 (1), 114-118. doi:10.5455/OVJ.2023.v13.i1.12 Chicago Style Kato, Keiko, Takaharu Itami, Shidow Torisu, Toshikazu Sakai, and Kazuto Yamashita. "Use of a gum elastic bougie in a cat with severe upper airway stenosis." Open Veterinary Journal 13 (2023), 114-118. doi:10.5455/OVJ.2023.v13.i1.12 MLA (The Modern Language Association) Style Kato, Keiko, Takaharu Itami, Shidow Torisu, Toshikazu Sakai, and Kazuto Yamashita. "Use of a gum elastic bougie in a cat with severe upper airway stenosis." Open Veterinary Journal 13.1 (2023), 114-118. Print. doi:10.5455/OVJ.2023.v13.i1.12 APA (American Psychological Association) Style Kato, K., Itami, . T., Torisu, . S., Sakai, . T. & Yamashita, . K. (2023) Use of a gum elastic bougie in a cat with severe upper airway stenosis. Open Veterinary Journal, 13 (1), 114-118. doi:10.5455/OVJ.2023.v13.i1.12 |