| Original Article | ||
Open Vet. J.. 2022; 12(3): 351-355 Open Veterinary Journal, (2022), Vol. 12(3): 351–355 Original Research Positive outcomes after surgical correction of grade IV medial patellar luxation in small breed dogsMitsuhiro Isaka*Laboratory of Companion Animal Surgery, Department of Small Animal Clinical Sciences, School of Veterinary Medicine, Rakuno Gakuen University, Hokkaido, Japan Corresponding Author: Mitsuhiro Isaka. Department of Small Animal Clinical Sciences School of Veterinary Medicine, Rakuno Gakuen University 582 Bunkyodai Midorimachi, Ebetsu, Hokkaido 069-8501, Japan. Email: m-isaka [at] rakuno.ac.jp Submitted: 29/09/2021 Accepted: 06/05/2022 Published: 30/05/2022 © 2022 Open Veterinary Journal
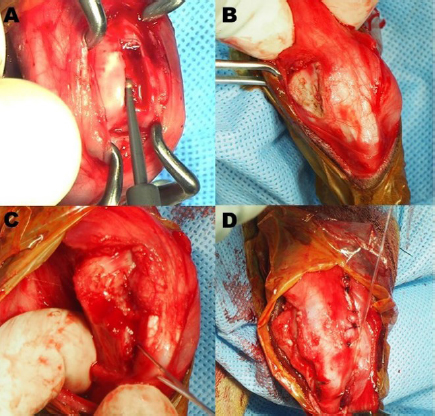
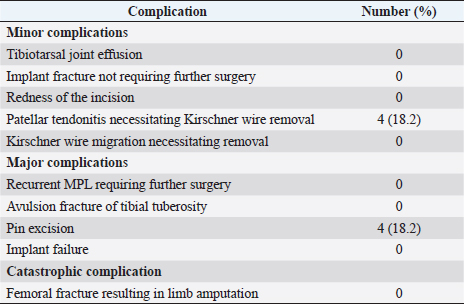
AbstractBackground: Medial patellar luxation (MPL) is a common orthopedic condition in dogs. After surgical correction, the recurrent rates appear to be higher and outcomes worse in grade IV than in lower grade MPL. Aim: To describe the outcomes of surgical correction of canine grade IV MPL. Methods: This retrospective study analyzed the medical records of 16 dogs (11 females, 5 males; mean age=5.05 years) with 22 stifle joints (8 left and 14 right) that underwent MPL surgery at Rakuno Gakuen University between May 2015 and October 2020. The procedures included capsulorrhaphy, trochlear block recession, tibial tuberosity transposition, medial retinacular release, and lateral fabellotibial suturing. The types of postsurgical complications, including a recurrence of MPL, were recorded. Results: Twelve of the 16 (75 %) dogs had concurrent contralateral MPL, and 2 dogs (12.5%) had concurrent cranial cruciate ligament rupture. The mean follow-up was 12.1 months. No lameness was observed. The outcomes of surgery for grade IV MPL were not associated with bilateral surgery, age, sex, body weight, or the preoperative quadriceps angle. Although none of the dogs showed any major or catastrophic complications following surgery, postoperative minor and major complications were observed in 8 of the 22 stifle joints (36.4%). Conclusion: Grade IV MPL is a complex orthopedic disease in dogs, which requires surgical patellar realignment to improve limb function. The surgical techniques used in this study were associated with a good prognosis without a surgical revision. Keywords: Canine diseases, Cranial cruciate ligament, Medial Patellar Luxation, Outcomes assessment, Postoperative complications. IntroductionMedial patellar luxation (MPL) is one of the most common orthopedic diseases in dogs (Roush, 1993). MPL is categorized according to Singleton’s four-grade system and is associated with anatomic abnormalities (Singleton, 1969). The most severe form is a grade IV luxation, which is characterized by permanent patellar luxation that cannot be reduced manually. Generally, various skeletal abnormalities, such as coxa vara, distal femoral varus, hypoplastic trochlear ridges, medial femoral condylar hypoplasia, tibial varus, and torsion, can be associated with MPL and are more common in dogs with grade IV MPL than in those with lower grade MPL (Bound et al., 2009; Wangdee et al., 2013; Yasukawa et al., 2016). Surgical treatment is recommended for dogs with MPL because it reduces pain and lameness. The risk of complications increases with the grade of MPL, and the severity of patellar luxation is associated with the number of corrective procedures required (Alam et al., 2007; Wangdee et al., 2013; Cashmore et al., 2014). In small breeds, the rate of MPL recurrence is higher, and outcomes are worse after surgical correction of grade IV MPL than those in lower grade luxation (Wangdee et al., 2013; Dunlap et al., 2016). The cranial cruciate ligament (CCL) is critical for the stability of the stifle joint. The function of this ligament has been described as stabilization during cranial tibial movement, preventing excessive relaxation of the stifle joint and internal rotation of the tibia (de Rooster et al., 2006). Lateral fabellotibial suturing techniques have been used as antirotational techniques for canine MPL (Hammer, 1979). However, to our knowledge, no studies have evaluated the outcomes and complications after internal rotation reconstruction using lateral fabellotibial suturing techniques for grade IV MPL in dogs. The purpose of this study was to determine the complications and surgical outcomes of surgical correction with internal rotation reconstruction of grade IV canine MPL in small breeds at 12 months after surgery. Materials and MethodsStudy populationWe reviewed the medical records of 100 dogs with MPL referred to the Rakuno Gakuen University that underwent surgery between May 2015 and October 2020. Among these, only dogs that had undergone surgery for grade IV MPL were included in the study. This resulted in 16 dogs with 22 affected stifle joints (8 on the left and 14 on the right) being analyzed in this study. Medical record reviewMedical records were reviewed to collect information on the dog breed, sex, and body weight at the time of surgery. Information was recorded on the affected limb, the presence and grade of concurrent contralateral MPL, and all surgical procedures, any implants, and preoperative quadriceps (Q) angles in radiographs (Pinna and Romagnoli, 2017). The surgical procedures performed, intra- and postoperative complications, were recorded. Complications were categorized as minor (not requiring additional surgical or medical treatment to resolve), major (complications or associated adverse effects requiring further surgical and medical treatment), and catastrophic (complications or associated adverse effects that caused permanent unacceptable impairment of function, were directly related to death, or prompted euthanasia), as defined previously (Cook et al., 2010). The only exception was that pin migration requiring removal under sedation was classified as a minor complication. For analytical purposes, recurrent MPL was classified as a major complication only when a surgical revision requiring general anesthesia had to be performed; a surgical revision was recommended but declined by the dog owner; or a grade IV MPL recurred. Additionally, a stifle joint with recurrent MPL and an outcome defined as unsuccessful on follow-up evaluation was classified as a major complication. The revision was defined as a surgical procedure performed at the anatomic site of the original surgery. The grade of any postoperative MPL was also recorded. Follow-up evaluationThe follow-up was short-term from at least 3 months to 6 months postoperatively (Cook et al., 2010; Dunlap et al., 2016). The mean follow-up time was 12.1 ± 11.4 months (between 6 and 44 months). The dog owners completed a questionnaire on their perceptions of their dogs’ postoperative pain, function, and quality of life (Cook et al., 2010). An orthopedic examination and radiography were performed when possible. A single observer (Dr. Isaka) performed all orthopedic examinations. The presence and grade of MPL, joint effusion, muscle atrophy, crepitus, CCL rupture, medial buttress, and signs of pain on joint palpation were recorded. Lameness at standing was evaluated while the dog was standing, walking, and trotting using the scale by Cook et al. (2010): 0=no observable lameness; 1=intermittent mild weight-bearing lameness with little, if any, change in gait; 2=consistent mild weight-bearing lameness with little change in gait; 3=moderate weight-bearing lameness with obvious lameness and noticeable change in gait; 4=severe weight-bearing lameness (toe-touching lameness only); and 5=nonweight-bearing lameness. The study protocol was approved by the review and ethics committee of Rakuno Gakuen University (VH20B9). Statistical analysisCategorical data of complications were presented as number and percentage. Other data were shown as average ± standard deviation. Comparisons of categorical data between dogs with and without complications were made using the Fisher exact test, with values of p ≤ 0.05 considered significant. ResultsStudy dogsFive dogs were male (4 castrated and 1 intact) and 11 were female (7 spayed and 4 intact). The breeds were as follows: Toy poodle (n=7), Pomeranian (n=3), Chihuahua (n=2), Yorkshire Terrier (n=2), Italian Greyhound (n=1), and mixed breed (n=1). Body weight at the time of surgery ranged from 1.95 to 6.92 kg (3.59 ± 1.44 kg). Age at the time of surgery ranged from 6 months to 12.0 years (5.05 ± 4.03 years; six dogs were less than a year old). Twelve of the 16 (75%) dogs had concurrent contralateral MPL (one grade I, one grade II, four grade III, and six grade IV). In addition, concurrent CCL rupture diagnosed by orthopedic examination, including cranial drawer signs and tibial compression test, without injury of tears was observed in 2 of 16 dogs (12.5%). Preoperative radiographic evaluation demonstrated a mean Q angle of 37.4 ± 6.0°, which was not associated with postoperative complications (mean postoperative Q angle of 8.3 ± 2.1°). Surgical methodsThe surgical techniques entailed capsulorrhaphy, trochlear block recession, tibial tuberosity transposition (TTT), medial retinacular release, and lateral fabellotibial suturing in all cases. Fabellotibial suturing was used of a single strand swaged on monofilament nylon (SECUROS, USA), and the tunnel location of the tibia was 2–3 mm apart from the osteotomy site of TTT (Fig. 1). Dogs with bilateral grade IV MPL underwent a single-stage bilateral procedure. Complications of MPL reconstructionPostoperative complications were observed in 8 of the 22 stifle joints (36.4%). No complications developed in the other 14 (63.6%) joints. Minor complications were confirmed in four stifles (18.2%), and major complications developed in four (18.2%) joints (Table 1). No surgical revision of any joint was necessary. None of the variables, age, body weight, concurrent contralateral MPL, ipsilateral CCL rupture, or the total number of procedures performed at the first surgery, was statistically associated with the development of minor and major postoperative complications. At the short-term follow-up examination, the MPL was resolved in all joints, and there was no lameness in any dog (100%).
Fig. 1. Surgical procedures. (A) Trochlear block recession. (B) Medial retinacular release. (C) Tibial tuberosity transposition using two Kirchner wires. (D) Lateral fabellotibial suturing using monofilament nylon. Table 1. Complications after surgical correction of grade IV medial patellar luxation in 16 small breed dogs (n=22 joints).
DiscussionThe risk of CCL rupture is higher in canine grade IV MPL than in lower grade luxations, which has been suggested to result from the chronic internal rotation of the tibia and increased strain on the CCL (Campbell et al., 2010). However, in our study, only 12.5% of the joints with grade IV MPL showed concurrent CCL rupture. In other words, general surgical techniques for MPL with lateral fabellotibial suturing are thought to be suitable for grade IV MPL in dogs with and without CCL rupture for preventing internal tibial rotation. The proportion of stifle joints that developed major complications after the surgical correction of grade IV MPL was much lower than that in other studies of grade IV MPL in small breed dogs (Dunlap et al., 2016; Hans et al., 2016). Hans et al. (2016) found an overall complication rate of 25.5%, with major complications, including revision surgery, occurring in 12.8% of 47 grade IV stifles. In another study of 24 grade IV MPL (Dunlap et al., 2016), approximately half of the dogs had postoperative complications (28% had minor complications and 24% had major complications), including a surgical revision rate of 21%. Approximately 40% of Pomeranian dogs with grade IV MPL showed a recurrence in a further study (Wangdee et al., 2013). In our cohort, no stifle joint required revision surgery after surgical correction for grade IV MPL, and the overall proportion of a recurrence of MPL within the 3-month follow-up period was the same. In our study, the preoperative Q angles showed no association with the surgical revision and recurrence rate of MPL, which is supported by the findings of Dunlap et al. (2016). Different surgical techniques have been used for grade IV MPL. Generally, a combination of surgical techniques has been found to be more effective than single procedures in the management of MPL (Alam et al., 2007). Recently, combined tibial plateau leveling osteotomy and tibial tuberosity transposition (TPLO-TTT) has been shown to be a reliable and effective technique for treating CCL insufficiency with concomitant MPL (Leonard et al., 2016). In the future, we need to compare TPLO-TTT with general surgical techniques and lateral fabellotibial suturing in the surgical correction of canine grade IV MPL. Single-session bilateral surgery for canine MPL has been associated with poor surgical outcomes (Fullagar et al., 2017). In our study, only one surgeon (Dr. Isaka) performed all surgeries. Thus, simultaneous bilateral surgery resulted in good outcomes, a finding that is supported by a previous study (Balogh and Kramek, 2016). Our results need to be interpreted within the limitations of this study that include its retrospective design, the subjective outcome evaluation, and a lack of long-term outcome data. However, the outcome and complication definitions used in this study were as recommended by Cook et al. (2010) for retrospective orthopedic studies. Furthermore, it has been suggested that pelvic limb function should be normal or near normal between 8 and 12 weeks after surgery (Cook et al., 2010). Thus, we consider that our study design allowed for an adequate evaluation of postoperative complications. In the future, long-term studies assessing objective outcome data (i.e., force platform gait analysis) could help to accurately assess pelvic limb function following surgical correction. Still, this may be difficult to achieve as the breeds overrepresented in MPL cohorts are toy breeds (DeAngelis and Hohn, 1970; Hayes et al., 1994). In conclusion, grade IV MPL is a complex orthopedic disease in dogs that requires surgical patellar realignment to improve limb function. The surgical techniques described in this study resulted in a good prognosis without surgical revision during a follow-up of 12 months. AcknowledgmentThe authors would like to thank Editage (www.editage.com) for English language editing. Conflict of interestThe authors have no conflict of interest to declare. ReferencesAlam, M.R., Lee, J.I., Kang, H.S., Kim, I.S., Park, S.Y., Lee, K.C., Kim, N.S. 2007. Frequency and distribution of patellar luxation in dogs. 134 cases (2000 to 2005). Vet. Comp. Orthop. Traumatol. 20, 59–64. Balogh, D.G. and Kramek, B. 2016. Clinical results of single- session bilateral medial patellar luxation repair in 26 small breed dogs. Can. Vet. J. 57, 427–430. Bound, N., Zakai, D., Butterworth, S.J., Pead, M. 2009. The prevalence of canine patellar luxation in three centres: clinical features and radiographic evidence of limb deviation. Vet. Comp. Orthop. Traumatol. 22, 32–37. Campbell, C.A., Horstman, C.L., Mason, D.R. and Evans, E.B. 2010. Severity of patellar luxation and frequency of concomitant cranial cruciate ligament rupture in dogs: 162 cases (2004–2007). J. Am. Vet. Med. Assoc. 236, 887–891. Cashmore, R.G., Havlicek, M., Perkins, N.R., James, D.R., Fearnside, S.M., Marchevsky, A.M., Black, A.P. 2014. Major complications and risk factors associated with surgical correction of congenital medial patellar luxation in 124 dogs. Vet. Comp. Orthop. Traumatol. 27, 263–270. Cook, J.L., Evans, R., Conzemius, M.G., Lascelles, B.D.X., Mcllwraith, C.W., Pozzi, A., Clegg, P., Innes, J., Schulz, K., Houlton, J., Fortier, L, Cross, A.R., Hayashi, K., Kapatkin, A., Brown, D.C., Stewart, A. 2010. Proposed definitions and criteria for reporting time frame, outcome, and complications for clinical orthopedic studies in veterinary medicine. Vet. Surg. 39, 905–908. DeAngelis, M. and Hohn, R.B. 1970. Evaluation of surgical correction of canine patella luxation in 142 cases. J. Am. Vet. Med. Assoc. 156, 587–594. de Rooster, H., de Bruin, T. and van Bree, H. 2006. Morphologic and functional features of canine cruciate ligaments. Vet. Surg. 35, 769–780. Dunlap, A.E., Kim, S.E., Lewis, D.D., Christopher, S.A., Pozzi, A. 2016. Outcomes and complications following surgical correction of grade IV medial patellar luxation in dogs: 24 cases (2008–2014). J. Am. Vet. Med. Assoc. 249, 208–213. Fullagar, B.A., Rajala-Schultz, P. and Hettlich, B.F. 2017. Comparison of complication rates of unilateral, staged bilateral, and single-session bilateral surgery for the treatment of bilateral medial patellar luxation in dogs. Can. Vet. J. 58, 39–44. Hammer, D.L. 1979. Surgical treatment of grade IV patellar luxation in the neoambulatory dog. J. Am. Vet. Med. Assoc. 174, 815–818. Hans, E.C., Kerwin, S.C., Elliott, A.C., Butler, R., Saunders, W.B., Hulse, D.A. 2016. Outcome following surgical correction of grade 4 medial patellar luxation in dogs: 47 stifles (2001–2012). J. Am. Anim. Hosp. Assoc. 52, 162–169. Hayes, A.G., Boudrieau, R.J., Hungerford, L.L. 1994. Frequency and distribution of medial and lateral patella luxation in dogs: 124 cases (1982–1992). J. Am. Vet. Med. 205, 716–720. Leonard, K.C., Kowaleski, M.P., Saunders, W.B., McCarthy, R.J., Boudrieau, R.J. 2016. Combined tibial plateau levelling osteotomy and tibial tuberosity transposition for treatment of cranial cruciate ligament insufficiency with concomitant medial patellar luxation. Vet. Comp. Orthop. Traumatol. 29, 536–540. Pinna, S. and Romagnoli, N. 2017. Radiographic measurement of the quadriceps angle in dogs. PLoS One 12, e0185833. Roush, J.K. 1993. Canine patellar luxation. Vet. Clin. North Am. Small Anim. Pract. 23, 855-868. Singleton, W.B. 1969. The surgical correction of stifle deformities in the dog. J. Small Anim. Pract. 10, 59-69. Wangdee, C., Theyse, L.F., Techakumphu, M., Soontornvipart, K., Hazewinkel, H.A.W. 2013. Evaluation of surgical treatment of medial patellar luxation in Pomeranian dogs. Vet. Comp. Orthop. Traumatol. 26, 435–439. Yasukawa, S., Edamura, K., Tanegashima, K., Seki, M., Teshima, K., Asano, K., Nakayama, T., Hayahi, K. 2016. Evaluation of bone deformities of the femur, tibia, and patella in Toy Poodles with medial patellar luxation using computed tomography. Vet. Comp. Orthop. Traumatol. 29, 29–38. | ||
| How to Cite this Article |
| Pubmed Style Mitsuhiro Isaka. Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.. Open Vet. J.. 2022; 12(3): 351-355. doi:10.5455/OVJ.2022.v12.i3.7 Web Style Mitsuhiro Isaka. Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.. https://www.openveterinaryjournal.com/?mno=119537 [Access: January 25, 2026]. doi:10.5455/OVJ.2022.v12.i3.7 AMA (American Medical Association) Style Mitsuhiro Isaka. Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.. Open Vet. J.. 2022; 12(3): 351-355. doi:10.5455/OVJ.2022.v12.i3.7 Vancouver/ICMJE Style Mitsuhiro Isaka. Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.. Open Vet. J.. (2022), [cited January 25, 2026]; 12(3): 351-355. doi:10.5455/OVJ.2022.v12.i3.7 Harvard Style Mitsuhiro Isaka (2022) Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.. Open Vet. J., 12 (3), 351-355. doi:10.5455/OVJ.2022.v12.i3.7 Turabian Style Mitsuhiro Isaka. 2022. Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.. Open Veterinary Journal, 12 (3), 351-355. doi:10.5455/OVJ.2022.v12.i3.7 Chicago Style Mitsuhiro Isaka. "Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.." Open Veterinary Journal 12 (2022), 351-355. doi:10.5455/OVJ.2022.v12.i3.7 MLA (The Modern Language Association) Style Mitsuhiro Isaka. "Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.." Open Veterinary Journal 12.3 (2022), 351-355. Print. doi:10.5455/OVJ.2022.v12.i3.7 APA (American Psychological Association) Style Mitsuhiro Isaka (2022) Positive Outcomes after Surgical Correction of Grade IV Medial Patellar Luxation in Small Breed Dogs.. Open Veterinary Journal, 12 (3), 351-355. doi:10.5455/OVJ.2022.v12.i3.7 |