| Case Report | ||
Open Vet. J.. 2022; 12(2): 192-196 Open Veterinary Journal, (2022), Vol. 12(2): 192–196 Case Report Intralesional steroid injection after endoluminal esophageal stricture dilatation in a catMaría Cecilia Ricart1,2*, Sergio Rodriguez2 and Guadalupe Dova31Universidad de Buenos Aires, Facultad de Ciencias Veterinarias, Cátedra de Clínica Médica de Pequeños Animales, CABA, Argentina 2EndoVete, Endoscopia Veterinaria, CABA, Argentina 3Gedyt, Gastroenterología Diagnóstica y Terapéutica, CABA, Argentina *Corresponding Author: María Cecilia Ricart. Universidad de Buenos Aires, Facultad de Ciencias Veterinarias, Cátedra de Clínica Médica de Pequeños Animales, CABA, Argentina. Email: cricart [at] fvet.uba.ar Submitted: 03/11/2021 Accepted: 18/02/2022 Published: 25/03/2022 © 2022 Open Veterinary Journal
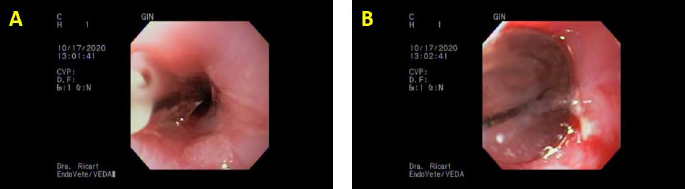
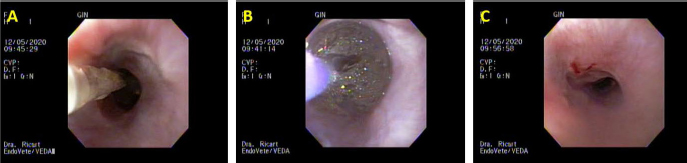
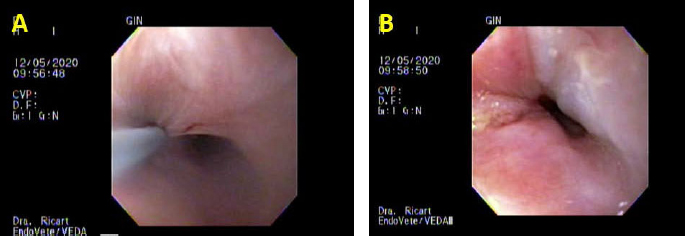
AbstractBackground: Benign esophageal strictures arise from various etiologies, mostly severe esophagitis. Although endoscopic balloon dilation is still the first-line therapy, refractory or recurrent strictures do occur and remain a challenge to the endoluminal treatment. The aim of this report was to communicate a recurrent esophageal stricture resolution in a cat treated with balloon dilatation and steroid injections in Ciudad de Buenos Aires, Argentina. Case Description: A 1-year-old spayed mix-breed female cat was consulted to the Veterinary Endoscopy Service for recurring regurgitation after two previous esophageal dilations. The cat had received doxycycline for Mycoplasma spp. infection and 20 days after the treatment consulted for dysphagia and regurgitation. Upper esophagogastroscopy (UGE) was performed with an Olympus CV-160 8.7 mm diameter endoscope; an annular 7 mm stricture was observed 3 cm caudal to the cranial esophagus sphincter. Three balloon dilatations procedures were performed with a Boston Scientific Controlled Radial Expansion (CRE) balloon 8–10–12 mm of 1 minute each. Because of ongoing clinical signs, another UGE was performed 15 days from the first procedure: a 3 mm stricture was encountered, balloon dilatation was repeated with 6–10–12 mm diameter, and a four-quadrant triamcinolone was injected in the submucosa. Clinically, the cat could eat with no alterations until day 20, where it started with mild dysphagia. Another UGE was performed, and the known stricture conserved a 11 mm diameter and balloon dilatation 12–15–16.5 mm with triamcinolone injection was repeated 30 days after the previous procedure. The cat could eat kibbles with no clinical signs in an 11-month follow-up. Conclusion: The alternative to triamcinolone injection after balloon dilatation presented in this clinical report was successful and it could be a therapeutic option for recurrent esophageal strictures in cats as it is in human medicine. Keywords: Balloon dilatation, Dysphagia, Feline. IntroductionA benign esophageal stricture (BES) arises from various etiologies and is defined by the narrowing of the lumen due to fibrosis or scar formation. In human medicine, simple strictures need three to five sessions of endoscopic dilatation, while benign refractory esophageal strictures (BRES) occur due to an inability to successfully maintain a stricture of a diameter of 14 mm over 5 sessions at 2-week or recurrent esophageal strictures as a result of an inability to maintain a satisfactory luminal diameter for 4 weeks once a diameter of 14 mm has been achieved (Siersema, 2019). In cats, two to four dilatation procedures may lead to the clinical resolution of esophageal strictures (German et al., 2005). Factors implicated in BES may include mechanical injuries, iatrogenic trauma during surgery or endoscopy, congenital stenosis, and chemical injuries (especially documented in cats) (Tan et al., 2017). Clinical signs of strictures depend on how narrow the stricture is; the narrower the stricture the more pronounced the regurgitation. It is important to consider that regurgitation also could be caused by painful swallowing (Kook, 2021). In human medicine, it is reported that significant dysphagia, chest pain, heartburn, and odynophagia may also result in regurgitation (Szapáry et al., 2018). Strictures closer to the pharynx may cause more immediate regurgitation with dysphagia, whereas mild to moderate strictures may cause no clinical signs until the cat swallows firm food or a large bolus. Often there is a contraction of the strictures with gradual progression in severity of the luminal narrowing (Kook, 2021). In human medicine, the most frequent cause of BRES is peptic stricture from pathological acid exposure in gastroesophageal reflux disease; less frequent etiologies include eosinophilic esophagitis (Szapáry et al., 2018). The pathogenesis of BRES is not entirely understood even in human medicine or in animals, but chronic inflammation is presumed to have a key role. The aim of this report was to communicate a recurrent esophageal stricture in a cat treated with balloon dilatation and steroid injections in Ciudad de Buenos Aires, Argentina. Case DetailsA 1-year-old spayed mix-breed female cat was consulted to the Veterinary Endoscopy Service for recurring regurgitation after two previous esophageal dilatations. The cat had received doxycycline for a Mycoplasma spp. infection and 20 days after the treatment consulted for dysphagia and regurgitation. Two separate dilatations occurred in other endoscopy services; information regarding the level of the stricture or type of dilatation technique was not available. The only information available about the procedures was that the owner mentioned an initial 3 mm stricture; however, the final diameter was unknown. After 15 days from the last dilatation, they consulted the service. Upper esophagogastroscopy (UGE) was performed under general anesthesia with an Olympus CV-160 8.7 mm diameter endoscope. For general anesthesia, a catheter was placed in the right cephalic antebrachial vein and was induced by intravenous (IV) injection of propofol 6 mg/kg (Propofol Gray®; Productos Farmacéuticos Dr. Gray S. A. C. I., Argentina) and isoflurane 5% (Forane® Isoflurane; Abbott Laboratories, Argentina). The trachea was intubated, and anesthesia was maintained with isoflurane (Forane® Isoflurane; Abbott Laboratories, Argentina) in 100% oxygen using a Bain breathing system. After the monitoring equipment was connected, a fentanyl bolus 2 μg/kg (Fentanilo Gray®; Productos Farmacéuticos Dr. Gray S. A. C. I.) was administered. Monitoring included a lead II electrocardiogram which was used to derive heart rate, pulse oximetry, noninvasive mean arterial pressure, and rectal temperature (PDJ-3000A Multi-Parameter ICU Portable Patient Monitor, Nanjing Puao Medical Equipment Co., Ltd.). NaCl solution 0.9% (Laboratorio P.L. Rivero & Cía®. S.A.I.C, Argentina) was administered IV at 5 ml/kg/hour during anesthesia, and maropitant 1 mg/kg subcutaneous (SC) (Cerenia®, maropitant 10 mg/ml; Zoetis Inc., MI, USA) and tramadol 2 mg/kg IV (Algen® 20, Tramadol 20 mg/ml; Richmond Vet Pharma, Argentina) were also administered. During UGE, a 7 mm annular stricture was observed 3 cm caudal to the cranial esophagus sphincter. The approximate diameter was measured by the comparison of the tip of a grasping forceps. Three balloon dilatation procedures were performed with a Boston Scientific Controlled Radial Expansion (CRE) balloon 8–10–12 mm, held for 1 minute at each diameter (Fig. 1). Between dilatations, the balloon was deflated for 30 seconds to allow mucosal reperfusion. Efficacy of the dilatation in every diameter was evaluated by macroscopic mucosal damage, drawing the attention to bleeding or tearing and intact mucosa. The endoscope traversed the dilatation with no stop at the end of the procedure. Afterward, gastroscopy was unremarkable. Anesthetic recovery was successful with no complications. The cat was discharged with indications for oral administration of 0.5 g sucralfate every 8 hours and to start oral wet feeding after 6 hours. The cat could eat soft food normally for 6 days, and thereafter it started with oral dysphagia and regurgitation; by day 10, it could only eat fluids and still had dysphagia. Another UGE under general anesthesia was performed 15 days from the first procedure with our service. A 3 mm stricture was encountered in the same place, and balloon dilatation was repeated with 6–10–12 mm diameter and a four-quadrant 0.3 ml of triamcinolone acetate 40 mg/ml was injected using a per-endoscopic needle (Disposable Injector NM-200 L, Olympus Medical Systems Corp®., Tokyo, Japan) in the submucosa. The procedure and the efficacy of the dilatation were performed as before. Anesthetic protocol and recovery were unremarkable. Clinically, the cat could eat with no alterations until day 20, where it started with mild dysphagia. Another UGE with the same anesthetic protocol was performed; the known stricture conserved a 11 mm diameter and balloon dilatation of 12–15–16.5 mm with triamcinolone injection was repeated 30 days after the previous procedure (Figs. 2 and 3). The cat could eat kibbles as a normal diet with weight gain with no clinical signs until an 11-month follow-up after the last treatment.
Fig. 1. The first set of dilatations with our endoscopy service. (A) Initial dilatation with a Boston Scientific CRE balloon of 12 mm. (B) Maximum inflation of the same balloon; note the mild bleeding and tearing of the mucosa; last dilatation of that day.
Fig. 2. Third day of endoluminal dilatation and second triamcinolone injection. (A) Initial dilatation with a Boston Scientific CRE balloon of 12 mm. (B) Balloon inflated during the maneuver; note there is no evidence of bleeding or tearing of the mucosa. (C) Macroscopic evaluation of mucosal damage after the third dilatation of the day; mild tearing is observed.
Fig. 3. Third day of endoluminal dilatation and second triamcinolone injection. (A) First quadrant injection in the submucosa with a per-endoscopic needle, 0.3 ml of triamcinolone acetate 40 mg/ml. (B) Evaluation of the endoluminal procedure after the four-quadrant injection. DiscussionThis case report describes successful therapy of recurrent esophageal strictures by combined endoscopic balloon dilatations in a cat local submucosal triamcinolone acetate injections that failed to respond to three balloon dilatations alone. In this clinical case, balloon dilatation was the therapeutic option, thus the stricture was annular; in other cases presenting long strictures, Savary–Gilliard dilatation is the better therapeutical option, and they need more dilatation sessions (Novais et al., 2008). Intralesional steroid injections have been suggested to inhibit the inflammatory response, thereby the stricture formation (Siersema, 2019). There were no differences in response outcomes between injections ranging from 0.5 to 2.8 ml of triamcinolone acetate or acetonide 10 or 40 mg/ml in human medicine Poincloux et al., 2017 In veterinary medicine, as to the authors’ knowledge, there are no specific guidelines with regard to the injection dose. The dose in this clinical case (triamcinolone acetate 40 mg/ml 0.3 ml in each quadrant) was chosen empirically. This is the range used in human medicine. The cat did not develop any complications associated with the high dose of corticosteroids. Double-blinded prospective studies are necessary to evaluate the range of dose for cats and dogs and guidelines for its use. Systemic corticosteroids have questionable efficacy in the prevention of esophageal strictures in human beings and dogs (Poincloux et al., 2017). It may be argued that a successful outcome in this clinical case might have been achieved with a fourth or fifth balloon dilatation procedure alone without the corticosteroid injections. There are reports of successful outcomes achieved in 88% of canines and felines with endoscopic balloon dilatation with a range of one to five procedures (Fraune et al., 2009). In another retrospective study of canine and feline animals suffering from esophageal strictures, despite one to four balloon dilation procedures (mean=3), stenosis recurred and subsequent esophageal stenting was chosen as an alternative therapeutic procedure. This article mentions that this procedure was performed in five dogs and in three cats; in these seven animals the stenting was successful; however, three had mild and three of them had severe discomfort evaluated as poor tolerance, ptyalism, persistence of occasional regurgitations, or needed progressive stent removal and replacement. In the three cats, trichobezoar caught was observed (Da Riz et al., 2021). It should be taken into account that the European Society of Gastrointestinal Endoscopy does not recommend permanent stent placement in humans for refractory benign stricture; stents should usually be removed at a maximum of 3 months following insertion (Spaander et al., 2021). The frequency at which the procedures were performed was not possible to control; unfortunately, the indication of repeating the procedure every 4–7 days was not a possibility in this clinical case. The third dilatation was delayed for 30 days because of owners’ personal reasons. As the American Heart Association and the American Society of Gastrointestinal Endoscopy do not recommend routine antibiotic coverage prophylaxis in human medicine, even if bacteremia is the most common complication that occurs in 2%–23% of the cases (Poincloux et al., 2017), it was decided not to give amoxicillin/clavulanic acid or other broad-spectrum antibiotics as other clinical reports in dogs or cats had empirically decided before (Corgozinho et al., 2009; Fraune et al., 2009; Poincloux et al., 2017). The cat showed no clinical signs of bacteremia as a consequence of the dilatation procedures in either session. The use of routine antibiotic coverage prophylaxis in dogs and cats should be reconsidered because of its concern for increased antimicrobial resistance and long-term changes in microbiota composition (Ziese and Suchodolski, 2021). ConclusionThe alternative to triamcinolone injection after balloon dilatation presented in this clinical report was successful and it could be a therapeutic option for recurrent esophageal strictures in cats as it is in human medicine. The clinical signs of strictures depend on the degree of obstruction; most of the time there is a gradual progression as the stricture continues to contract, with more pronounced regurgitation and dysphagia; clinicians should take into account this differential diagnosis. AcknowledgmentThe authors would like to acknowledge the authorization from the family of the cat for the publication of the case report. Authors’ contributionsMCR: case evaluation, endoscopic management, manuscript drafting, and approval of the final manuscript; SMR: case evaluation, anesthesia administration and monitoring, critical revisions, and approval of the final manuscript; GD: endoscopic guidance, critical revisions, and approval of the final manuscript. Conflicts of interestAll authors declare that there are no conflicts of interest. ReferencesCorgozinho, K.B., Neves, A., Belchior, C., Toledo, F., Moreira de Souza, H.J. and da Hora, A.S. 2009. Uso de triancinolona local em uma gata com estenose esofágica. Acta Sci. Vet. 34, 175–178. Da Riz, F., Béguin, J., Manassero, M., Faucher, M. and Freiche, V. 2021. Outcome of dogs and cats with benign oesophageal strictures after balloon dilatation or stenting: 27 cases (2002–2019). J. Small Anim. Pract. 62(10), 886–894. Fraune, C., Gaschen, F. and Ryan, K. 2009. Intralesional corticosteroid injection in addition to endoscopic balloon dilation in a dog with benign oesophageal strictures. J. Small Anim. Pract. 50, 550–553. German, A.J., Cannon, M.J., Dye, C., Booth, M.J., Pearson, G.R., Reay, C.A. and Gruffydd-Jones, T.J. 2005. Oesophageal strictures in cats associated with doxycycline therapy. J. Feline Med. Surg. 7(1), 33–41. Kook, P.H. 2021. Esophagitis in cats and dogs. Vet. Clin. North Am. Small Anim. Pract. 51, 1–15. Novais, P., Lemme, E., Equi, C., Medeiros, C., Lopes, C. and Vargas, C. 2008. Estenoses benignas de esôfago: abordagem endoscópica com velas de Savary-Gilliard [Benign strictures of the esophagus: endoscopic approach with Savary-Gilliard bougies]. Arq Gastroenterol. 45(4), 290–4. Poincloux, L., Rouquette, O. and Abergel, A. 2017. Endoscopic treatment of benign esophageal strictures: a literature review. Exp. Rev. Gastroenterol. Hepatol. 11(1), 53–64. Siersema, P.D. 2019. How to approach a patient with refractory or recurrent benign esophageal stricture. Gastroenterology 156, 7–10. Spaander, M.C.V., van der Bogt, R.D., Baron, T.H., Albers, D., Blero, D., de Ceglie, A., Conio, M., Czakó, L., Everett, S., Garcia-Pagán, J.C., Ginès, A., Jovani, M., Repici, A., Rodrigues-Pinto, E., Siersema, P.D., Fuccio, L. and van Hooft, J.E. 2021. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—update 2021. Endoscopy 53(7), 751–762. Szapáry, L., Tinusz, B., Farkas, N., Márta, K., Szakó, L., Meczker, A., Hágendorn, R., Bajor, J., Vincze, Á., Gyöngyi, Z., Mikó, A., Csupor, D., Hegyi, P. and Erőss, B. 2018. Intralesional steroid is beneficial in benign refractory esophageal strictures: a meta-analysis. World J. Gastroenterol. 24(21), 2311–2319. Tan, D., Weisse, C., Berent, A. and Lamb, K.E. 2017. Prospective evaluation of an indwelling esophageal balloon dilatation feeding tube for treatment of benign esophageal strictures in dogs and cats. J. Vet. Intern. Med. 32, 693–700. Ziese, A.N. and Suchodolski, J.S. 2021. Impact of changes in gastrointestinal microbiota in canine and feline digestive diseases. Vet. Clin. North Am. Small Anim. Pract. 51, 155–169. | ||
| How to Cite this Article |
| Pubmed Style Ricart MC, Rodriguez S, Dova G. Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat. Open Vet. J.. 2022; 12(2): 192-196. doi:10.5455/OVJ.2022.v12.i2.6 Web Style Ricart MC, Rodriguez S, Dova G. Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat. https://www.openveterinaryjournal.com/?mno=136271 [Access: January 11, 2026]. doi:10.5455/OVJ.2022.v12.i2.6 AMA (American Medical Association) Style Ricart MC, Rodriguez S, Dova G. Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat. Open Vet. J.. 2022; 12(2): 192-196. doi:10.5455/OVJ.2022.v12.i2.6 Vancouver/ICMJE Style Ricart MC, Rodriguez S, Dova G. Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat. Open Vet. J.. (2022), [cited January 11, 2026]; 12(2): 192-196. doi:10.5455/OVJ.2022.v12.i2.6 Harvard Style Ricart, M. C., Rodriguez, . S. & Dova, . G. (2022) Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat. Open Vet. J., 12 (2), 192-196. doi:10.5455/OVJ.2022.v12.i2.6 Turabian Style Ricart, Mara Cecilia, Sergio Rodriguez, and Guadalupe Dova. 2022. Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat. Open Veterinary Journal, 12 (2), 192-196. doi:10.5455/OVJ.2022.v12.i2.6 Chicago Style Ricart, Mara Cecilia, Sergio Rodriguez, and Guadalupe Dova. "Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat." Open Veterinary Journal 12 (2022), 192-196. doi:10.5455/OVJ.2022.v12.i2.6 MLA (The Modern Language Association) Style Ricart, Mara Cecilia, Sergio Rodriguez, and Guadalupe Dova. "Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat." Open Veterinary Journal 12.2 (2022), 192-196. Print. doi:10.5455/OVJ.2022.v12.i2.6 APA (American Psychological Association) Style Ricart, M. C., Rodriguez, . S. & Dova, . G. (2022) Intralesional steroid injection after endoluminal esophageal stricture dilatation in a cat. Open Veterinary Journal, 12 (2), 192-196. doi:10.5455/OVJ.2022.v12.i2.6 |