| Research Article | ||
Open Vet. J.. 2024; 14(4): 980-989 Open Veterinary Journal, (2024), Vol. 14(4): 980–989 Original Research Hematological ratios and indices in canine large B-cell lymphomaAlessandra Gavazza1, Valentina Cremonini2, Arianna Miglio2*, Chiara Starita3, Giacomo Rossi1 and Maria Teresa Antognoni21School of Biosciences and Veterinary Medicine, University of Camerino, Matelica, Italy 2Department of Veterinary Medicine, University of Perugia, Perugia, Italy 3IDEXX Laboratories Italia, Milano, Italy *Corresponding Author: Arianna Miglio. Department of Veterinary Medicine, University of Perugia, Italy. Email: arianna.miglio [at] unipg.it Submitted: 19/10/2023 Accepted: 01/03/2024 Published: 30/04/2024 © 2024 Open Veterinary Journal
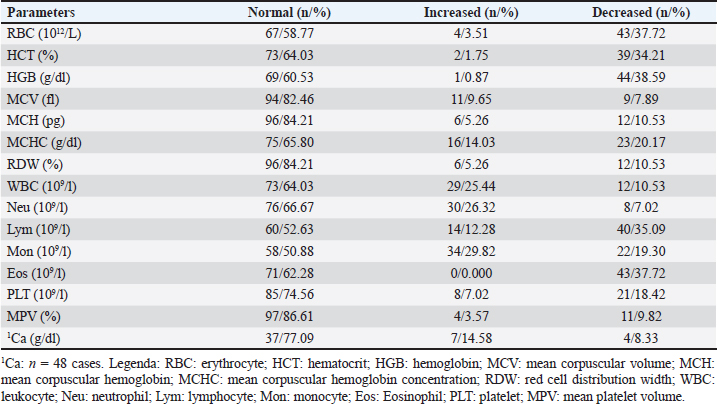
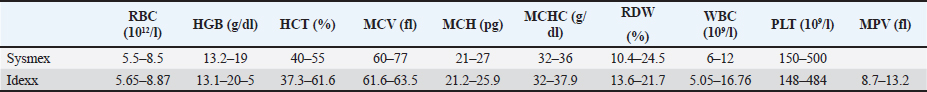
AbstractBackground: Canine lymphoma is the most common hematopoietic cancer in dogs. Numerous studies have evaluated the prognostic value of hematological abnormalities and ratios in both humans and dogs with lymphoma. Aim: To compare hematological parameters and complete blood count ratios between a population of dogs affected by lymphoma and healthy dogs to identify potential prognostic markers for lymphoma. Methods: This retrospective case-control study compares hematological parameters and complete blood count ratios between a population of 114 dogs affected by multicentric large B-cell lymphoma (LBCL) and 60 healthy dogs. Results: The study found several statistically significant differences between the hematological indices of LBCL dogs and healthy dogs, but no correlation between these parameters and the survival times of 78 dogs treated with chemotherapy Madison Wisconsin protocol. In addition, hematological alterations were evaluated such as anemia, leukocytosis, and thrombocytopenia. Conclusion: Hematological ratios have been suggested as potential prognostic markers for canine LBCL but their real prognostic value remains controversial and requires future investigation. Keywords: Dogs, Lymphoma, CBC, Indices, Ratios. IntroductionCanine lymphoma is the most prevalent hematopoietic malignancy in dogs. This term encompasses a group of heterogeneous diseases that differ in clinical presentation, immunophenotype, and prognosis (Valli et al., 2013; Zandvliet, 2016; Antognoni et al., 2021; Magni et al., 2023). Canine Lymphoma is a correspondent to non-Hodgkin Lymphoma in humans. Large B-cell lymphoma (LBCL) is the most frequent immunophenotype of multicentric lymphoma in dogs. Typically, lymphoma is diagnosed in middle-aged or dogs older than 10 years. Although no significant gender predisposition has been demonstrated, spayed females appear to have an increased risk (Zandvliet, 2016). The most widely used therapy for canine lymphoma consists of a multidrug combination (CHOP-based protocol) of cyclophosphamide, doxorubicin, vincristine, prednisone, and l-asparaginase without maintenance further therapy. The neoplasm is extremely aggressive, with a median survival time under treatment of approximately 8–10 months in dogs with LBCL (Bienzle and Vernau, 2011; Valli et al., 2013; Zandvliet, 2016). Many prognostic factors have been considered significant for LBCL, including clinical symptoms, stage, histological aspects, grade, proliferation markers, and response to treatment (Zandvliet, 2016; Davies et al., 2018). Given the aggressive behavior of LBCL, prognostic markers that allow monitoring the course of the disease in an easy, repeatable, and inexpensive way, are of critical importance. Many studies have focused on hematological parameters as potential prognostic markers. The hematologic examination is a minimally invasive procedure available to all veterinary clinicians, and it is routinely executed before chemotherapy administration. Several hematological parameters both in human and veterinary medicine have been proposed as prognostic markers for many different diseases, including vascular (Balta et al., 2016), degenerative (Wan et al., 2020), and inflammatory diseases (Neumann, 2021), as well as different types of tumors, such as soft tissue sarcoma (Macfarlane et al., 2016), laryngeal carcinoma (Yılmaz et al., 2018), acute myeloid leukemia (Zhang et al., 2021), and lymphomas (Henriques et al., 2021), and others. The possibility to use neutrophils/lymphocytes ratio (NLR) as an independent prognostic factor has been investigated in human patients with LBCL. To date, a high NLR value has been found to be associated with poor overall survival and poor progression-free survival. At the time of diagnosis, an NLR cut-off value of 3 has been reported in one study (Wang et al., 2017), and 3.5 in another (Porrata et al., 2010). This association between a high NLR and poor prognosis may be related to the production of inflammation mediators, resulting in immunosuppression and a reduction in the patient’s immune efficacy. In addition, a high platelets/lymphocytes ratio (PLR) appears to be correlated with a worse clinical condition of the patient and a poor prognosis in human LBCL, as reported by a 2019 meta-analysis study (Chen et al., 2019). In veterinary medicine, the predictive value of platelets/neutrophils ratio (PNR), NLR, and the level of anemia as prognostic factors in dogs with a diagnosis of LBCL has been suggested. Patients with a higher PNR above 0.032 showed earlier disease progression than others, while patients with NLR above 7.5 showed a higher mortality rate at 180 days (Henriques et al., 2021). On the other hand, several studies in both human and veterinary medicine have failed to demonstrate a statistically significant association between NLR and overall survival or progression-free survival (Mutz et al., 2015; Azuma et al., 2019). In humans, multiple studies have identified higher red blood cell (RBC) distribution width (RDW) as a negative prognostic factor in patients with LBCL (Zhou et al., 2017; Ai et al., 2018; Hasan and Elmeshhedany, 2021). In dogs, the prognostic value of this index has been investigated for a few diseases (Guglielmini et al., 2013, 2021, 2022; Garcia-Arce et al., 2022; Miglio et al., 2023) and only one study considered LBCL (Martinez et al., 2019). Furthermore, to date, the red blood cell distribution width to total serum calcium ratio (RDW/Ca) has been investigated and suggested as a ratio of prognostic relevance only in patients with acute pancreatitis, in both humans (Gravito-Soares et al., 2018; Han et al., 2021) and canine species (Guglielmini et al., 2022). However, the prognostic value of these hematological ratios in canine LBCL remains controversial and under investigated. Most of the existing studies conducted on this topic lack a control group of healthy patients for comparison. The main objective of the study is to assess the role of hematological ratios in LBCL by establishing a comprehensive list of dogs with LBCL and comparing them to reference intervals (RIs) in a population of healthy dogs. We also aimed to investigate the possible correlation of these indexes with the survival times of dogs receiving treatment with a chemotherapy Madison Wisconsin protocol. Furthermore, complete blood count (CBC) and Ca modifications compared to the reference range (RR) and the possible correlation of white blood cell (WBC), RBC, and Platelet (PLT) count with survival times were evaluated. Materials and MethodsAnimal recruitmentThe medical records of 180 dogs presented at two University Teaching Hospitals (University of Camerino and University of Perugia), between 2012 and 2022 were retrospectively reviewed. Dogs affected by lymphoma were considered eligible if they had a diagnosis of multicentric lymphoma, according to the criteria established by the World Health Organization (WHO) classification (Valli et al., 2011) not specialists in hematopathology, in applying the World Health Organization (WHO. Dogs with infiltration of neoplastic cells in peripheral blood and/or bone marrow, detected by cytological observation, were excluded from the study. The control group included healthy blood donor dogs. Data regarding hematology CBC and available calcium level measurements of both the investigated groups of dogs were obtained from the review of the medical database and subsequently analyzed. Dogs with LBCLThe first group included a total of 114 dogs affected by LBCL classified in the III–IV stage based on the WHO staging. For all dogs, the diagnostic protocol was similar to those indicated in previous studies (Valli et al., 2011; Marconato et al., 2015; Mutz et al., 2015; Henriques et al., 2021). The evaluation was performed by considering history, physical examination, CBC and microscopic blood smear evaluation with differential count (Supplementary Table 1), biochemistry and urinalysis, thoracic radiographs, abdominal ultrasound, and cytology evaluation of fine-needle aspirate (FNA) of enlarged peripheral lymph nodes. FNA of the liver and spleen were included in case of suggested altered ultrasound appearance. Immunophenotyping of lymphoma was performed by lymph node immunohistochemistry (CD21, CD79a, CD45) or flow cytometry (CD3, CD5, CD21, CD34, CD79a). A bone marrow FNA aspirate and cytology were performed in 41 dogs, but no circulating neoplastic cells were observed on the blood smear of all cases by expert veterinary or board-certified clinical pathologists. Seventy-eight dogs were treated, with prior written informed consent by the owners, with chemotherapy Madison-Wisconsin protocol (L-asparaginase, cyclophosphamide, vincristine, doxorubicin, prednisone). The duration of the administration of chemotherapy lasts 25 weeks. Healthy dogsThe second group of dogs, defined as being healthy (H), served as a control for the investigated parameters. These dogs were presented for a complete period of screening before blood donation and they underwent an evaluation to accomplish the requirements indicated in the Italian Ministry of Health Guidelines regarding the healthy measures adopted in veterinary blood transfusion (Ministero della Salute Dipartimento della Sanità Pubblica e dell’Innovazione, 2016), i.e., history of no clinical signs, regular prophylaxis, and vaccination, physical examination without findings. CBC, blood smear evaluation, total serum protein, and serological titers were also routinely evaluated. A total of 60 control dogs were enrolled in the study, all of whom were clinically healthy, between 2 and 8 years old, weighed more than 25 kg, and of different breeds and sexes. Blood collection and analysisAll analyses evaluated in this study were performed on the day of diagnosis for dogs affected by LBCL. All dogs had CBC parameters measured using automated hematology analyzers (ProCyte Dx, IDEXX®, and Sysmex XT-1800-i®), on whole peripheral blood samples collected in 1 ml K3 ethylenediaminetetraacetic acid tubes. Hematological alterations were calculated based on the reference ranges of each analyzer used (Supplementary Table 2). Calcium total level was assessed by liquid chemistry (Hitachi 904, Boehringer Mannheim® and Seac Radim® reagent, Biolabo sas, France) in 1 ml serum samples. Calculation of CBC ratios and indicesNLR, PLR, monocytes/lymphocytes ratio (MLR), and PNR were calculated as ratios of the absolute values of neutrophils, platelets, monocytes to lymphocytes, and the platelet count to neutrophils, respectively. The MPV/PLT ratio was calculated as a ratio of mean platelet volume to platelets. The RDW/Ca ratio was calculated as a ratio of red cell distribution width and Ca levels. Survival timeThe survival time was calculated from the first visit to lymphoma-related death. Statistical analysisThe evaluation of the normality of parameters was performed with the Shapiro-Wilk test. Data are not normally distributed. Each variable was compared by the Mann-Whitney test. Differences were considered statistically significant when p < 0.05. The lymphoma-specific survival (LSS) was evaluated by the Kaplan-Meyer method. In addition, median and standard deviation were determined for each parameter for cases, mean, median, standard deviation, and percentiles (0.025–0.975) for control. A Kaplan-Mayer analysis with a log-rank test was performed to evaluate the correlation between ratio and LSS. A Rank correlation test was also performed by assuming as a risk factor a cut-off greater than the max calculated for ratios and indices in healthy dogs. Statistical analysis was performed using a software package (MedCalc® Version 19.1.3., Ostend, Belgium). Ethical approvalNot needed for this retrospective study. ResultsOne hundred and fourteen cases of LBCL that met the inclusion criteria were included in the study. Of these cases, 78 were treated with the Madison Wisconsin protocol. The mean age of the cases was 7.95 ± 2.93 (SD) years, with 70 (61.4%) males and 44 (38.6%) females. The most common breeds included 32 (28.07%) mixed breed, 17 (14.91%) German Shepherd, 6 (5.26%) Golden Retriever, 6 (5.26%) Rottweiler, 5 (4.38%) Boxer, 5 (4.38%) Border collie, 5 (4.38%) Labrador retriever, 5 (4.38%) Irish Setter, 4 (4.38%) Dobermann, 4 (4.38%) Bernese Mountain dog, and 25 (21.9%) other breeds. The mean age of the control dogs was 5.00 ± 2.01 (SD) years, with 33 (55.00%) males and 27 (45.00%) females. The most common breeds included 15 (25.00%) Segugio italiano, 10 (16.66%) mixed breeds, 4 (6.67%) Weimaraner, 4 (6.67%) Ariegeois, 4 (6.67%) Bleu de Gascoigne, 4 (6.67%) Bracco Italiano, 3 (5%) and 16 (26,66%) dogs of various other breeds. A CBC was performed at the time of diagnosis for all cases, and the results and any alterations are described in Table 1. Serum calcium measurements were evaluated for 48 cases. The statistical results of the control group’s ratios are reported in Table 2. The reference values are expressed by percentiles (0.025/0.975). Table 3 shows ratios and indexes both in cases and control groups and compared by statistical methods. None of the ratios and indexes examined can be considered a prognostic factor related to survival in a population of dogs with lymphoma (end point 6 and 12 months; rank correlation test; p > 0.05). Also, the rank correlation test performed by assuming as a risk factor a cut-off greater than the mean calculated for ratios and indices in healthy dogs (NLR > 2.54; MLR > 0.13; PNR > 41.49; PLR > 106.89; MPV/PLT > 0.04; RDW > 16.9; RDW/Ca > 1.91) not resulted as a prognostic factor. The lymphoma-specific median survival (LSS) time (represented in Fig. 1) for the 78 treated cases was 223 days (range 11–1792), with two dogs still alive. Among the dogs, 28 (36.84%) died within 180 days, while 48 (63.16%) survived > 180 days. The LSS of anemic dogs was 172 days, compared to 247 days for nonanemic dogs, but no statistical significance was found between survival and the presence of anemia. Furthermore, we did not find an association between LSS and neutrophil and platelet count. Three dogs whose LSS was >1050 days (1074, 1298, and 1792 days) (Marconato et al., 2011, 2015; Childress et al., 2018; Davies et al., 2018; Childress et al., 2022; Faroni et al., 2021) received additional chemotherapy protocols when, following initial clinical remission, they developed relapse. DiscussionThe aim of the present study was to evaluate a complete list of ratio and hematological indices in canine lymphoma, compare them with ratios in healthy dogs, and eventually study the prognostic role of these parameters with LSS. Table 1. Hematological alterations in dogs with DLBCL.
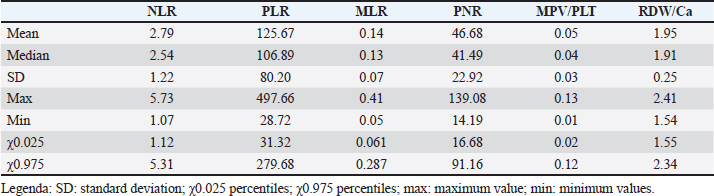
Table 2. RIs of control dogs’ ratios.
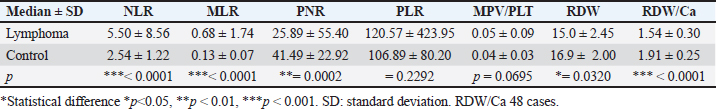
Table 3. Ratio and indexes in healthy and DLBCL dogs.
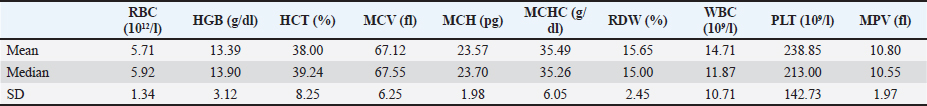
One hundred and fourteen dogs with LBCL and sixty control dogs were analyzed. Anemia (predominantly normocytic normochromic or macrocytic hypochromic) was present in about 37% of examined cases with LBCL and, in many studies, has been described as a negative prognostic indicator in dogs treated with CHOP-based chemotherapy protocol (Miller et al., 2009; Curran and Thamm, 2016; Henriques et al., 2021). We can observe that MCV was increased (macrocytosis) only in 9% of cases, to show that, probably, it is not regenerative. However, in this study, we did not find any statistical association between anemic subjects and LSS, despite having observed a decrease in survival times, as described by Vos et al. (2019). This is probably because the cases of LBCL were limited to the III and IV clinical stages and the anemia observed was always mild or moderate and only in two cases severe. Observed anemia in oncologic disease is mostly associated with chronic disease in conjunction with decreased availability of iron, but also with bone marrow erythroid hypoplasia and immune-mediated hemolytic process, but underlying pathogenesis in veterinary patients is, to date, not fully understood (Mutz et al., 2015; Garrett et al., 2002). No correlation between platelet counts and leukocyte counts, and LSS was found. Neutropenia, typical of more advanced subjects undergoing chemotherapy, was also present in a reduced number of cases, supporting the lack of bone marrow involvement at this stage (Henriques et al., 2021). The median LSS of LBCL was 223 days, similar to other studies previously reported with the same chemotherapy protocol used (Gavazza et al., 2008; Henriques et al., 2021; Mutz et al., 2015). The control group was represented by healthy dogs that regularly donate blood to the veterinary blood banks of the University of Perugia and the University of Camerino. This allowed us to calculate a complete list of indices and evaluate RI in healthy dogs. This process begins with a healthy reference population made up of individuals who are initially chosen based on inclusion or exclusion criteria. In some research papers, the value of the hematological ratio from healthy dogs has been partially evaluated to compare them with pathological cases, but the RIs were never calculated for a full variety of ratios. To make medical decisions and to evaluate the patient’s conditions the test results are compared with correct Ris (Forget et al., 2017; Latimer and Duncan, 2011a). It has been recognized to be essential to evaluate the RIs of ratios with statistical methods in healthy animals to estimate the difference between oncologic and hematological disease (Geffré et al., 2009; Friedrichs et al., 2012; Miglio et al., 2020). So far, NLR is the most investigated index, and we can observe that the median value determined in our study (2.54) is between that determined by Benvenuti et al. (2020) (3 median) and Rejec (2017) (2.7 median). Moreover, the evaluation of RIs in healthy dogs allowed us to make a statistical comparison with the indices calculated in the population affected by lymphoma. Table 3 shows the statistically significant differences in ratio and hematological indexes between the two populations. Malignancy-associated systemic inflammatory response assessed by CBC indices (NLR, PLR, MLR, MPV/PLT, PLR) has already been shown to correlate with the pathogenesis and prognosis of certain cancers in humans and veterinary (Bhatti et al., 2010; Kwon et al., 2012; Balta et al., 2013; Marconato et al., 2015). In the present study, we used, in relation to the risk factor, as a cut-off a value greater than the mean obtained from indices in healthy dogs to be able to provide a unique value independent from receiver operating characteristic (ROC) curves. None of the variables analyzed showed statistical significance. Below is the description and commentary of the individual indexes. The NLR ratio has been widely investigated in both human and veterinary medicine for oncological and nononcological diseases. The purpose of this study was to compare the body’s inflammatory response with the immune response derived from disorders. The systemic inflammatory response in dogs and humans with neoplastic conditions, which interact directly and indirectly with host’s inflammatory cells, has been well described (Elinav et al., 2013). In our study, NLR in lymphoma was two times greater than in the control group (5.50 versus 2.54; p < 0.0001) due to the production of neutrophils in the inflammatory response and tumor-associated immunosuppressive mediators. In humans, NLR > 3.5 was considered a negative prognostic factor for survival (Porrata et al., 2010) but no correlation was found in the present study. Then, the NLR was not found to be a significant value for LSS in this study, similar to what was observed by Mutz et al. (2015) but contrary to the results reported by Henriques et al. (2021), who found a positive association between survival and NLR > 7.45 at 180 days. The median of patients with NLR < 5.5 (max normal value) was compared with patients with NLR > 5.5 and no statistically significant difference was found. Regarding leukocytosis, and in particular neutrophilia, as a typical value in advanced tumor stages that was associated to inflammation and tissue necrosis, we can observe that, instead, in our study neutrophilia was present in 26% of dogs and lymphopenia in 35% of dogs (Watabe et al., 2011). Significant statistical differences between LBCL subjects and healthy dogs were also observed for MLR (0.68 vs. 0.13) and PNR (25.89 vs. 41.49). As previously reported, higher MLR was associated with a risk of death in dogs with sepsis (Pierini et al., 2020) but lower MLR in nonsurvivors dogs with primary immune-mediated hemolytic anemia was noticed (Alaimo et al., 2023). The development of lymphopenia (35%) and monocytosis (29%) was marked in LBCL dogs and could explain higher MLR. Monocytes are an essential component of the innate immune system, which may be elevated in various diseases, generally migrate from blood to various tissues, and secrete a variety of substances that modulate inflammatory response (Latimer and Duncan, 2011b). Dogs with lymphoma that present PNR value above 0.032 have an earlier disease progression but no correlation with LSS has been demonstrated. The interaction between neutrophils and platelets in cancer can cause changes in the PNR index in both humans and dogs, especially where paraneoplastic hypercoagulability syndrome is present. The presence of different mediators in the hypercoagulability syndrome plays a crucial role in perpetuating inflammation and thus the progression of cancer (Henriques et al., 2021). In our study, PNR was lower in dogs with lymphoma compared to healthy dogs because thrombocytopenia is more frequent than thrombocytosis, and neutrophilia is proportionally represented in a higher percentage of cases. However, no correlation between these indices and LSS has been observed but we cannot rule out that it influences the progression of the disease. The PLR index was not systematically studied in neoplastic diseases. No statistically significant difference between LBCL and healthy dogs (120.57 vs. 106.89) for the PLR index was observed in this report. In human patients affected by B cell lymphoma, the high value of PLR was associated with shorter overall survival and progression free survival (Wang et al., 2017). Thus far, in dogs diffuse large B cell lymphoma PLR value was associated with Overall Survival but not for the progression of the disease (Henriques et al., 2021). A study showed that PLR was not significantly different despite the observation that the highest values of PLR were found in dogs with oropharyngeal tumors when compared to healthy dogs. The results do not support PLR as a systemic biomarkers oropharyngeal tumors disease activity (Rejec et al., 2017). Also, MPV, if increased, indicates an abnormal rate of platelet production and stimulation. Thrombocytosis and increased MPV are indicated to be associated with a worse prognosis in multiple solid tumors in humans (Karaman et al., 2011; Kurt et al., 2012; Korniluk et al., 2019). The study of Rejec et al. (2017) does not confirm significant differences in MPV/PLT values between groups of healthy and neoplastic dogs (Rejec et al., 2017). Similar to the PLR, unfortunately, no statistically significant difference was observed in this study between dogs with lymphoma and healthy dogs. Therefore, the role of the MPV/PLT ratio remains inconclusive (Rejec et al., 2017). The interpretation of RDW in combination with mean corpuscular volume (MCV) may further aid the subclassification of anemias. High baseline RDW has previously been demonstrated as an independent prognostic marker of poor outcomes in human patients with LBCL (Periša et al., 2015). Then, RDW is suggested as a parameter reflecting the level of systemic inflammatory response in dogs and is helpful in predicting its severity and results in acute pancreatitis (Guglielmini et al., 2022). Moreover, significantly increased RDW values were noticed in dogs with cardiorespiratory, renal, neoplastic (lymphoma), hepatic, endocrine, and immune-mediated diseases. Despite having found a significant difference between dogs with lymphoma and healthy dogs in our study, surprisingly the RDW of the first is lower than the second. This trend agrees with the results reported by the study of Martinez et al. (2019), in which the diagnosis of multicentric lymphoma was based on peripheral lymphadenopathy and cytological or histopathological, but the clinical staging was missing. In addition, both values are fully within the reference ranges, therefore it does not seem to have prognostic significance unlike in cardiovascular diseases (Martinez et al., 2019). Indeed, a recent study showed that RDW can be considered, even within RIs, an independent predictor of poor outcomes in dogs with myxomatous mitral valve disease (Guglielmini et al., 2021). Certainly, further evaluation of the prognostic meaning of RDW in cancer, and particularly, in canine, lymphoma is necessary. It will also be useful to evaluate the progress of RDW in the progression of the disease. RDW/Ca ratio has been shown to be an excellent predictor of acute pancreatitis severity and mortality in humans (Han et al., 2021). In dogs with acute pancreatitis, RDW/Ca was significantly higher in nonsurvivors compared to survivors, which suggests that the presence of hypocalcemia can be a concern in dogs with this condition and an RDW of >12.7% had good accuracy in predicting short-term death (Guglielmini et al., 2022). However, in dogs with lymphoma, hypocalcemia was rarely observed, but hypercalcemia was more frequently observed in immunophenotype T (Zandvliet, 2016). This may explain the lack of correlation of the RDW/Ca index with the survival times. The study presents several limitations, including the retrospective nature and some dogs, as described, have received multiple chemotherapy treatments. Also, it is known that the interpretation of the blood and bone marrow smear was strongly operator-dependent but this limit cannot be eliminated. In addition, bone marrow cytology was not performed in all dogs, but they were classified in clinical stage III–IV excluding the presence of circulating neoplastic cells on blood and/or bone marrow smears. ConclusionA comprehensive evaluation of hematological ratios and indices was conducted and compared with a healthy dog population. Ratios were economical and easy markers to evaluate immune processes and acute or chronic inflammation. In our study, despite having observed several statistically significant differences between the hematological ratios of LBCL dogs and healthy, no correlation with survival times was found. Then, the prognostic value of hematological ratios is still controversial in canine LBCL also in relation to the method of calculating the cut-offs, and it remains under investigation. AcknowledgmentThe authors are grateful to Niccolò Rossi for the English revisions. Conflict of interestThe authors declare that there is no conflict of interest. FundingNone. Authors’ contributionsAll authors contributed to this study. All authors read and approved the final manuscript. Data availabilityAll data from this study are provided in the manuscript. ReferencesAi, L., Mu, S. and Hu, Y. 2018. Prognostic role of RDW in hematological malignancies: a systematic review and meta-analysis. Cancer Cell. Int. 18(1), 61. Alaimo, C., De Feo, G., Lubas, G. and Gavazza, A. 2023. Utility and prognostic significance of leukocyte ratios in dogs with primary immune-mediated hemolytic anemia. Vet. Res. Commun. 47(1), 305–310. Antognoni, M.T., Misia, A.L., Brachelente, C., Mechelli, L., Paolini, A. and Miglio, A. 2021. Non epitheliotropic b-cell lymphoma with plasmablastic differentiation versus cutaneous plasmacytosis in a 12-Years-Old BEAGLE: case presentation and clinical review. Vet. Sci. 8(12), 317. Azuma, Y., Nakaya, A., Fujita, S., Satake, A., Nakanishi, T., Tsubokura, Y., Saito, R., Konishi, A., Hotta, M., Yoshimura, H., Ishii, K., Ito, T. and Nomura, S. 2019. Neutrophil-to-lymphocyte ratio (NLR) fails to predict outcome of diffuse large B cell lymphoma. Leukemia Res. Rep. 12, 100173. Balta, S., Demirkol, S., Unlu, M., Arslan, Z. and Celik, T. 2013. Neutrophil to lymphocyte ratio may be predict of mortality in all conditions. Br. J. Cancer, 109(12), 3125–3126. Balta, S., Ozturk, C., Balta, I., Demirkol, S., Demir, M., Celik, T. and Iyisoy, A. 2016. The neutrophil–lymphocyte ratio and inflammation. Angiology 67(3), 298–299. Benvenuti, E., Pierini, A., Gori, E., Lucarelli, C., Lubas, G. and Marchetti, V. 2020. Neutrophil-to-lymphocyte ratio (NLR) in canine inflammatory bowel disease (IBD). Vet. Sci. 7(3), 141. Bhatti, I., Peacock, O., Lloyd, G., Larvin, M. and Hall, R.I. 2010. Preoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil-lymphocyte versus platelet-lymphocyte ratio. Am. J. Surg. 200(2), 197–203. Bienzle, D. and Vernau, W. 2011. The diagnostic assessment of canine lymphoma: implications for treatment. Clin. Lab. Med. 31(1), 21–39. Chen, Y., Zhang, Z., Fang, Q. and Jian, H. 2019. Prognostic impact of platelet-to-lymphocyte ratio on diffuse large B-cell lymphoma: a meta-analysis. Cancer Cell Int. 19(1), 245. Childress, M.O., Christian, J.A., Ramos-Vara, J.A., Rosen, N.K. and Ruple, A. 2022. Greater baseline serum C-reactive protein concentrations are associated with reduced survival in dogs receiving cyclophosphamide, doxorubicin, vincristine, and prednisone chemotherapy for primary nodal diffuse large B-cell lymphoma. Vet. J. 289, 105911. Childress, M.O., Ramos-Vara, J.A. and Ruple, A. 2018. Retrospective analysis of factors affecting clinical outcome following CHOP-based chemotherapy in dogs with primary nodal diffuse large B-cell lymphoma. Vet. Comp. Oncol. 16(1), E159–E168. Curran, K. and Thamm, D.H. 2016. Retrospective analysis for treatment of naïve canine multicentric lymphoma with a 15-week, maintenance-free CHOP protocol: fifteen-week CHOP protocol for canine lymphoma. Vet. Comp. Oncol. 14, 147–155. Davies, O., Szladovits, B., Polton, G., Garden, O.A., Leo, C. and Lara-Garcia, A. 2018. Prognostic significance of clinical presentation, induction and rescue treatment in 42 cases of canine centroblastic diffuse large B-cell multicentric lymphoma in the United Kingdom. Vet. Comp. Oncol. 16(2), 276–287. Elinav, E., Nowarski, R., Thaiss, C. A., Hu, B., Jin, C. and Flavell, R. A. 2013. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nature Rev. Cancer, 13(11), 759–771. Faroni, E., Sabattini, S., Lenzi, J., Guerra, D., Comazzi, S., Aresu, L., Mazzanti, A., Zanardi, S., Cola, V., Lotito, E. and Marconato, L. 2021. Sleeping beauty: anesthesia may promote relapse in dogs with diffuse large b-cell lymphoma in complete remission after chemo-immunotherapy. Front. Vet. Sci. 8, 760603. Forget, P., Khalifa, C., Defour, J.-P., Latinne, D., Van Pel, M.-C. and De Kock, M. 2017. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res. Notes 10(1), 12. Friedrichs, K.R., Harr, K.E., Freeman, K.P., Szladovits, B., Walton, R.M., Barnhart, K.F. and Blanco-Chavez, J. 2012. ASVCP reference interval guidelines: determination of de novo reference intervals in veterinary species and other related topics. Vet. Clin. Pathol. 41(4), 441–453. Garcia-Arce, M., Gow, A.G., Handel, I., Ngoi, W. and Thomas, E. 2022. Retrospective evaluation of red blood cell distribution width as a prognostic factor in critically ill dogs (December 2016 to April 2017): 127 cas. J. Vet. Emerg. Crit. Care, 32(3), 405–412. Garrett, L.D., Thamm, D.H., Chun, R., Dudley, R. and Vail, D.M. 2002. Evaluation of a 6-month chemotherapy protocol with no maintenance therapy for dogs with lymphoma. J. Vet. Int. Med. 16(6), 704–709. Gavazza, A., Lubas, G., Valori, E. and Gugliucci, B. 2008. Retrospective survey of malignant lymphoma cases in the dog: clinical, therapeutical and prognostic features. Vet. Res. Commun. 32(S1), 291–293. Geffré, A., Friedrichs, K., Harr, K., Concordet, D., Trumel, C. and Braun, J.-P. 2009. Reference values: a review. Vet. Clin. Pathol. 38(3), 288–298. Gravito-Soares, M., Gravito-Soares, E., Gomes, D., Almeida, N. and Tomé, L. 2018. Red cell distribution width and red cell distribution width to total serum calcium ratio as major predictors of severity and mortality in acute pancreatitis. BMC Gastroenterol. 18(1), 108. Guglielmini, C., Crisi, P.E., Tardo, A.M., Di Maggio, R., Contiero, B., Boari, A., Fracassi, F. and Miglio, A. 2022. Prognostic role of red cell distribution width and other routine clinico-pathological parameters in dogs with acute pancreatitis. Animals 12(24), 3483. Guglielmini, C., Poser, H., Pria, A.D., Drigo, M., Mazzotta, E., Berlanda, M. and Luciani, A. 2013. Red blood cell distribution width in dogs with chronic degenerative valvular disease. J. Am. Vet. Med. Assoc. 243(6), 858–862. Guglielmini, C., Valentini, C.M., Contiero, B., Valente, C. and Poser, H. 2021. Red cell distribution width has a negative prognostic role in dogs with myxomatous mitral valve disease. Animals 11(3), 778. Han, T.-Y., Cheng, T., Liu, B.-F., He, Y.-R., Pan, P., Yang, W.-T., Qiang-Lai and Cao, Y. 2021. Evaluation of the Prognostic value of red cell distribution width to total serum calcium ratio in patients with acute pancreatitis. Gastroenterol. Res. Pract. 2021, 1–6. Hasan, K.M. and Elmeshhedany, A.Y. 2021. Prognostic value of absolute lymphocyte/monocyte ratio, red cell distribution width and neutrophil/lymphocyte ratio in diffuse large B-cell lymphoma patients. Cell. Mol. Biol. 67(3), 61–68. Henriques, J., Felisberto, R., Constantino-Casas, F., Cabeçadas, J. and Dobson, J. 2021. Peripheral blood cell ratios as prognostic factors in canine diffuse large B-cell lymphoma treated with CHOP protocol. Vet. Comp. Oncol. 19(2), 242–252. Karaman, K., Bostanci, E.B., Aksoy, E., Kurt, M., Celep, B., Ulas, M., Dalgic, T., Surmelioglu, A., Hayran, M. and Akoglu, M. 2011. The predictive value of mean platelet volume in differential diagnosis of non-functional pancreatic neuroendocrine tumors from pancreatic adenocarcinomas. Euro. J. Int. Med. 22(6), e95–e98. Korniluk, A., Koper-Lenkiewicz, O.M., Kamińska, J., Kemona, H. and Dymicka-Piekarska, V. 2019. Mean platelet volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions. Mediat. Inflam. 2019, 1–14. Kurt, M., Onal, I.K., Sayilir, A., Beyazit, Y., Oztas, E., Kekilli, M., Turhan, N., Karaman, K. and Akdogan, M. 2012. The role of mean platelet volume in the diagnosis of hepatocellular carcinoma in patients with chronic liver disease. Hepatogastroenterology 59(117), 1580–1582. Kwon, H.-C., Kim, S.H., Oh, S.Y., Lee, S., Lee, J.H., Choi, H.-J., Park, K.-J., Roh, M.S., Kim, S.-G., Kim, H.-J. and Lee, J.H. 2012. Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 17(3), 216–222. Latimer, K.S. and Duncan, J.R. 2011a. Generating and interpreting test results: test validity, quality control, reference values and basic epidemiology. In Duncan and Prasse’s veterinary laboratory medicine: clinical pathology, 5th ed. Hoboken, NJ: Wiley-Blackwell, pp: 365–391. Latimer, K. S. and Duncan, J. R. 2011b. Leukocytes. In Duncan and Prasse’s veterinary laboratory medicine: clinical pathology, 5th ed. Hoboken, NJ: Wiley-Blackwell, pp: 45–82. Macfarlane, L., Morris, J., Pratschke, K., Mellor, D., Scase, T., Macfarlane, M. and Mclauchlan, G. 2016. Diagnostic value of neutrophil-lymphocyte and albumin-globulin ratios in canine soft tissue sarcoma: biomarkers in soft tissue sarcoma. J. Small Anim. Pract. 57(3), 135–141. Magni, T., Signore, F.D., Vignoli, M., Terragni, R., Poli, A., Parisi, F., Sampaolo, M., Boari, A., Miglio, A. and Crisi, P.E. 2023. Skeletal muscle dissemination in a dog with T-cell lymphoma. Vet. Med. Sci. 9(1), 53–58. Marconato, L., Martini, V., Stefanello, D., Moretti, P., Ferrari, R., Comazzi, S., Laganga, P., Riondato, F. and Aresu, L. 2015. Peripheral blood lymphocyte/monocyte ratio as a useful prognostic factor in dogs with diffuse large B-cell lymphoma receiving chemoimmunotherapy. Vet. J. 206(2), 226–230. Marconato, L., Stefanello, D., Valenti, P., Bonfanti, U., Comazzi, S., Roccabianca, P., Caniatti, M., Romanelli, G., Massari, F. and Zini, E. 2011. Predictors of long-term survival in dogs with high-grade multicentric lymphoma. J. Am. Vet. Med. Assoc. 238(4), 480–485. Martinez, C., Mooney, C.T., Shiel, R.E., Tang, P.K., Mooney, L. and O’Neill, E.J. 2019. Evaluation of red blood cell distribution width in dogs with various illnesses. Can Vet. J. 60, 964–971. Miglio, A., Gavazza, A., Siepi, D., Bagaglia, F., Misia, A. and Antognoni, M.T. 2020. Hematological and biochemical reference intervals for 5 adult hunting dog breeds using a blood donor database. Animals 10(7), 1212. Miglio, A., Valente, C. and Guglielmini, C. 2023. Red blood cell distribution width as a novel parameter in canine disorders: literature review and future prospective. Animals 13(6), 985. Miller, A.G., Morley, P.S., Rao, S., Avery, A.C., Lana, S.E. and Olver, C.S. 2009. Anemia is associated with decreased survival time in dogs with lymphoma. J. Vet. Int. Med. 23(1), 116–122. Ministero della Salute Dipartimento della Sanità Pubblica e dell’Innovazione. 2016. Linea Guida relativa all’esercizio delle attività riguardanti la medicina trasfusionale in campo veterinario. Mutz, M., Boudreaux, B., Kearney, M., Stroda, K., Gaunt, S. and Shiomitsu, K. 2015. Prognostic value of baseline absolute lymphocyte concentration and neutrophil/lymphocyte ratio in dogs with newly diagnosed multi-centric lymphoma. Vet. Comp. Oncol. 13(4), 337–347. Neumann, S. 2021. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in dogs and cats with acute pancreatitis. Vet. Clin. Pathol. 50(1), 45–51. Periša, V., Zibar, L., Sinčić-Petričević, J., Knezović, A., Periša, I. and Barbić, J. 2015. Red blood cell distribution width as a simple negative prognostic factor in patients with diffuse large B-cell lymphoma: a retrospective study. Croatian Med. J. 56(4), 334–343. Pierini, A., Gori, E., Lippi, I., Lubas, G. and Marchetti, V. 2020. Are leukocyte and platelet abnormalities and complete blood count ratios potential prognostic markers in canine sepsis? Front. Vet. Sci. 7, 578846. Porrata, L.F., Ristow, K., Habermann, T., Inwards, D.J., Micallef, I.N. and Markovic, S.N. 2010. Predicting survival for diffuse large B-cell lymphoma patients using baseline neutrophil/lymphocyte ratio. Am. J. Hematol. 85(11), 896–899. Rejec, A., Butinar, J., Gawor, J. and Petelin, M. 2017. Evaluation of complete blood count indices (NLR, PLR, MPV/PLT, and PLCRi) in healthy dogs, dogs with periodontitis, and dogs with oropharyngeal tumors as potential biomarkers of systemic inflammatory response. J. Vet. Dentist. 34(4), 231–240. Valli, V.E., Kass, P.H., Myint, M.S. and Scott, F. 2013. Canine lymphomas: association of classification type, disease stage, tumor subtype, mitotic rate, and treatment with survival. Vet. Pathol. 50(5), 738–748. Valli, V.E., Myint, M.S., Barthel, A., Bienzle, D., Caswell, J., Colbatzky, F., Durham, A., Ehrhart, E.J., Johnson, Y., Jones, C., Kiupel, M., Labelle, P., Lester, S., Miller, M., Moore, P., Moroff, S., Roccabianca, P., Ramos-Vara, J., Ross, A., Scase, T., Tvedten, H. and Vernau, W. 2011. Classification of canine malignant lymphomas according to the World Health Organization Criteria. Vet. Pathol. 48(1), 198–211. Vos, N., Pellin, M. and Vail, D.M. 2019. A comparison of 12- and 19-week CHOP protocols using non-randomized, contemporaneous controls. Vet. Comp. Oncol. 17(3), 276–284. Wan, J., Wang, X., Zhen, Y., Chen, X., Yao, P., Liu, W., Lu, E., Du, Y., Liu, H. and Zhao, S. 2020. The predictive role of the neutrophil–lymphocyte ratio in the prognosis of adult patients with stroke. Chinese Neurosurg. J. 6(1), 22. Wang, J., Zhou, X., Liu, Y., Li, Z. and Li, X. 2017. Prognostic significance of neutrophil-to-lymphocyte ratio in diffuse large B-cell lymphoma: a meta-analysis. PLoS One 12(4), e0176008. Watabe, A., Fukumoto, S., Komatsu, T., Endo, Y. and Kadosawa, T. 2011. Alterations of lymphocyte subpopulations in healthy dogs with aging and in dogs with cancer. Vet. Immunol. Immunopathol. 142(3–4), 189–200. Yılmaz, B., Şengül, E., Gül, A., Alabalık, U., Özkurt, F.E., Akdağ, M. and Topçu, İ. 2018. Neutrophil–lymphocyte ratio as a prognostic factor in laryngeal carcinoma. Indian J. Otolaryngol. Head Neck Surg. 70(2), 175–179. Zandvliet, M. 2016. Canine lymphoma: a review. Vet. Quart. 36(2), 76–104. Zhang, Q., Yang, Q., Weng, Y., Huang, Z., Chen, R., Zhu, Y., Dai, K., Zhang, S., Jiang, S. and Yu, K. 2021. Neutrophil-to-lymphocyte ratio correlates with prognosis and response to chemotherapy in patients with non-M3 de novo acute myeloid leukemia. Translat. Cancer Res. 10(2), 1013–1024. Zhou, S., Fang, F., Chen, H., Zhang, W., Chen, Y., Shi, Y., Zheng, Z., Ma, Y., Tang, L., Feng, J., Zhang, Y., Sun, L., Chen, Y., Liang, B., Yu, K. and Jiang, S. 2017. Prognostic significance of the red blood cell distribution width in diffuse large B-cell lymphoma patients. Oncotarget, 8(25), 40724–40731. Supplementary MaterialsSupplementary Table 1. Differential blood count.
Supplementary Table 2. RR of hematological parameters.
| ||
| How to Cite this Article |
| Pubmed Style Gavazza A, Cremonini V, Miglio A, Starita C, Rossi G, Antognoni MT. Hematological ratios and indices in canine large B-cell lymphoma. Open Vet. J.. 2024; 14(4): 980-989. doi:10.5455/OVJ.2024.v14.i4.5 Web Style Gavazza A, Cremonini V, Miglio A, Starita C, Rossi G, Antognoni MT. Hematological ratios and indices in canine large B-cell lymphoma. https://www.openveterinaryjournal.com/?mno=173624 [Access: January 08, 2026]. doi:10.5455/OVJ.2024.v14.i4.5 AMA (American Medical Association) Style Gavazza A, Cremonini V, Miglio A, Starita C, Rossi G, Antognoni MT. Hematological ratios and indices in canine large B-cell lymphoma. Open Vet. J.. 2024; 14(4): 980-989. doi:10.5455/OVJ.2024.v14.i4.5 Vancouver/ICMJE Style Gavazza A, Cremonini V, Miglio A, Starita C, Rossi G, Antognoni MT. Hematological ratios and indices in canine large B-cell lymphoma. Open Vet. J.. (2024), [cited January 08, 2026]; 14(4): 980-989. doi:10.5455/OVJ.2024.v14.i4.5 Harvard Style Gavazza, A., Cremonini, . V., Miglio, . A., Starita, . C., Rossi, . G. & Antognoni, . M. T. (2024) Hematological ratios and indices in canine large B-cell lymphoma. Open Vet. J., 14 (4), 980-989. doi:10.5455/OVJ.2024.v14.i4.5 Turabian Style Gavazza, Alessandra, Valentina Cremonini, Arianna Miglio, Chiara Starita, Giacomo Rossi, and Maria Teresa Antognoni. 2024. Hematological ratios and indices in canine large B-cell lymphoma. Open Veterinary Journal, 14 (4), 980-989. doi:10.5455/OVJ.2024.v14.i4.5 Chicago Style Gavazza, Alessandra, Valentina Cremonini, Arianna Miglio, Chiara Starita, Giacomo Rossi, and Maria Teresa Antognoni. "Hematological ratios and indices in canine large B-cell lymphoma." Open Veterinary Journal 14 (2024), 980-989. doi:10.5455/OVJ.2024.v14.i4.5 MLA (The Modern Language Association) Style Gavazza, Alessandra, Valentina Cremonini, Arianna Miglio, Chiara Starita, Giacomo Rossi, and Maria Teresa Antognoni. "Hematological ratios and indices in canine large B-cell lymphoma." Open Veterinary Journal 14.4 (2024), 980-989. Print. doi:10.5455/OVJ.2024.v14.i4.5 APA (American Psychological Association) Style Gavazza, A., Cremonini, . V., Miglio, . A., Starita, . C., Rossi, . G. & Antognoni, . M. T. (2024) Hematological ratios and indices in canine large B-cell lymphoma. Open Veterinary Journal, 14 (4), 980-989. doi:10.5455/OVJ.2024.v14.i4.5 |