| Case Report | ||
Open Vet. J.. 2024; 14(8): 2110-2115 Open Veterinary Journal, (2024), Vol. 14(8): 2110–2115 Case Report A rare case of “Hawkins type 3” talar neck fracture in a catJon Andre Berg1,2*1Department of Preclinical Sciences and Pathology, Faculty of Veterinary Medicine, Norwegian University of Life Sciences, Ås, Norway 2AniCura Jeløy Dyresykehus, Moss, Norway *Corresponding Author: Jon Andre Berg. Department of Preclinical Sciences and Pathology, Faculty of Veterinary Medicine, Norwegian University of Life Sciences, Ås, Norway. Email: jon.andre.berg [at] nmbu.no Submitted: 23/06/2024 Accepted: 11/07/2024 Published: 31/08/2024 © 2024 Open Veterinary Journal
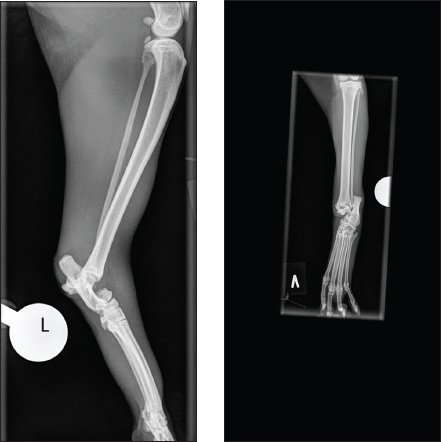
ABSTRACTBackground: Fractures of the talus are relatively infrequently reported in small animals. Furthermore, talar neck fracture in cats seems to be very rare. This case report aims to consider the diagnosis, treatment, and a 7-month follow-up of a cat with a Hawkins type 3 talar fracture treated with a type 1b external skeletal fixator (ESF). Emphasizing on the complexity of the injury, considering treatment options and complications, and comparing them to previous reports on cats and humans. Case Description: A 4.5-year-old mixed-breed cat was diagnosed with a Hawkins type 3 talar fracture. Additionally, there were considerations related to the collateral support of the hock joint. The fracture fragment, i.e., the talar body and parts of the neck, was reduced with pointed reduction forceps through a small medial insition. The fracture was then stabilized with a trans articular type 1b ESF. Based on radiographic fracture assessment, de-staging of the frame was done 8 weeks postoperatively. While complete frame removal was at 12 weeks postoperatively. Seven months after the fracture, the cat was minimally lame when walking, and there was a reduced range of motion in the hock joint compared to the contralateral joint. Conclusion: Based on this case and the four previous cases with talar neck fractures, we cannot conclude, but ESF seems to be a good solution, especially when considering the possibility of disruption to the collateral support of the hock joint in this case. Keywords: Cats, External fixation, Fracture, Talocrural joint, Talus. IntroductionThe tarsal joint consists of the tarsal bones and the joints between the crus and the metatarsus. Ninety percent of movement occurs in the tarsocrural joint (Carmichael and Marshall, 2018). The talus is the only bone that articulates with the tibia and fibula and is the most complex structure of all tarsal bones. Anatomically, the talus consists of the body, neck, and head, where the body is composed of the trochlea, which articulates with the cochlea of the tibia. The talar head articulates with the central tarsal bone (Vollmerhausl et al., 2002a). Furthermore, there is a strong articulation between the talus and the calcaneus (Vollmerhausl et al., 2002a, 2002b). The talus gets most of its blood supply from the dorsal pedal artery, a continuation of the cranial tibial artery at the level of the tarsocrural joint (Barnes, 1993; Lahunta et al., 2013). The supporting structures of the feline tarsal joint differ from those of the dog and have been well described (Young et al., 1993; Vollmerhausl et al., 2002b). Injuries to the talus are complicated because the bone is articular and plays a prominent role in the weight-bearing process (Carmichael and Marshall, 2018). Talar fractures are uncommon in cats and dogs, with talar neck fractures being extremely rare in cats (McCartney and Carmichael, 2000; Piermattei et al., 2006; DeCamp et al., 2016). In humans, talar fractures represent 0.1%–2.5% of all fractures and 3%–5% of foot and ankle fractures (von Knoch et al., 2007; Fournier et al., 2012; Lee et al., 2020). There is no current classification system for talar neck fractures in small animals, while in humans, talar neck fractures are classified after Hawkins, where Hawkin’s type 3 talar neck fracture is defined as displaced with subtalar and tibiotalar dislocation (Hawkins LG, 1970). This case report describes radiographical findings, management, and mid-term follow-up of a cat with a Hawkins-type 3 talar neck fracture (Cook et al., 2010). Case DetailsA mixed-breed spayed female cat, 4.5 years old and 5.2 kg, was seen at the out-of-hours service due to acute non-weight-bearing lameness of unknown cause on the left pelvic limb. This is a client-owned cat, and the owner signed a consent form approving all interventions mentioned here. Therefore, no further ethical approval was needed. The basic clinical examination and neurological examination were unremarkable. The cat was examined for evidence of other injuries apart from the limb. This included a general blood profile (hematology and biochemistry) and thoracic and abdominal radiographs, all unremarkable. The initial treatment was intravenous fluid (IV) 25 ml/hour (Ringer acetat, Fresenius Kabi) and analgesia in the form of 0.3 mg/kg/4 hours Methadone (0.3 mg/ml) intramuscular (IM) (Insistor vet, VetViva Richter Salfarm Scandinavia) and an initial dose of 0.3 mg/kg subcutaneously (SC) Meloxicam 5 mg/ml (Metacam vet. Boehringer Ingelheim Animal Health Nordics A/S). Finally, the affected leg was protected with a well-padded bandage overnight. After the first 24 hours, the meloxicam dose was reduced to half the initial dose. The following day, the cat was pre-medicated by adding Dexmedetomidine (0.5 mg/ml) at a dose of 20 µg/kg IM (Dexdomitor vet, Orion Pharma Animal Health) to the already provided Methadone. General anesthesia was induced with IV Propofol (10 mg/ml) (PropoVet Multidose, Zoetis Animal Health ASA) at a dose of 1.2 mg/kg to effect, and the cat was intubated and maintained on sevoflurane in 100% oxygen. Palpation of the affected leg revealed noticeable swelling and discontinuity of the hook joint. The fracture was closed, and orthogonal radiographs revealed a dislocated talar neck fracture, with tibiotalar and subtalar luxation (Fig. 1a and 1b). Based on the nature of the fracture, it was anticipated that there would be collateral support disruption. Fracture repair was performed using a routine aseptic hanging limb, ensuring intraoperative fluoroscopy could pass around the hock joint. An initial attempt at closed reduction of the fracture fragment was made but proved difficult. Therefore, a small medial incision was made, and the fracture fragment was repositioned using pointed reduction forceps and traction. The fracture was stabilized with a unilateral biplanar trans articular external fixator [External skeletal fixator (ESF) type 1b], using small treaded Elis pins, the Kirscher–Ehmer plus system (Veterinary instrumentation, Sheffield) drilled into the tibia, tarsal and proximal metatarsals through stab incisions, as previously described techniques for pin placements (Palmer, 1999; Kraus et al., 2003), using a battery-driven drill (Colibri II, Depuy Synths). The external fixation bars were contoured to approximately 125. The craniomedial and craniolateral incisions were closed routinely with poliglecaprone 25 4–0 (monocryl, Ethicone), and the total surgical time was 70 minutes.
Fig. 1. (A and B) Mediolateral and craniocaudal digital radiography of the left hock joint. The talar neck fracture is evident, with luxation of both the tibiotalar and subtalar joints.
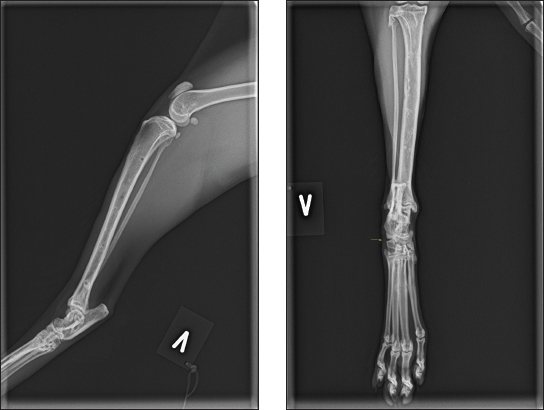
Fig. 2. (A and B) Mediolateral and craniocaudal digital radiograph of the left hock joint eight weeks post-operative. The fracture line was well visible. The lateral frame was removed at this stage. A protective bandage was applied to the external fixators to protect the cat and the environment (owner, kids, and furniture). Post-operative orthogonal radiographs were taken to confirm satisfactory reduction and pin placements. The cat was hospitalized for another 24 hours for analgesic treatment, where Methadone was gradually changed to Buprenorphine 0.3 mg/ml with a dose of 10–20 µg/kg (IM) at an interval of 8 hours (Bupaq vet. Bupaq Multidose vet. VetViva Richter, Salfarm Scandinavia AS). Additionally, the cat received a meloxicam oral mixture (suspension) of 0.5 mg/ml with a dose of 0.05 mg/kg (Metacam vet. Boehringer Ingelheim Animal Health Nordics A/S); oral meloxicam was continued at home for 7 days. Based on previous reports, we estimated a fracture healing time to be approximately 10–14 weeks (McCartney and Carmichael, 2000). Furthermore, advice was given to keep the cat in a large dog transport cage for 6 weeks. The cage should be large enough for food and water, bowels, toilet, and sleeping area, and the cat should be able to move around. The cat was allowed out for cuddles when the owner was home. After 6 weeks, the cat could be in the living room until the first scheduled re-examination at 8 weeks postoperatively. Complications arose after 7 days when the cat had escaped the owner, resulting in one loose pin on the craniolateral frame. The cat was anesthetized as previously, and orthogonal radiographs confirmed that the fracture was not affected. The cat was aseptically prepared and taken to the theatre, where the loos pin was replaced and the frame reconnected. A new bandage was provided before new orthogonal post-operative radiographs confirming proper pin placement. The cat was discharged the same day, and the initial post-operative plan was maintained. Eight weeks postoperatively, the cat was back for re-examination and radiographs. The owner reported that the cat moved freely around the house after 6 weeks of cage rest. The cat was anesthetized as previously, orthogonal radiographs revealed good fracture healing (Fig. 2a and 2b), and the lateral frame was removed according to standard procedures (Kraus et al., 2003). Twelve weeks postoperatively, the cat was back for re-examination and radiographs, and the owner could report that the cat was doing fine. The cat was anesthetized as previously for orthogonal radiographs, which revealed good fracture healing, and the medial frame was removed. A set of new orthogonal radiographs was taken after frame removal. Palpation of the affected talocrural joint revealed a moderately reduced range of motion (ROM) compared to the opposite joint. Measurements with a goniometer showed left extension at 160°, flexion at 67°, right extension at 167°, and flexion at 20° (Jaeger et al., 2007). Thirty-three weeks postoperatively, the cat was seen for a progress check. The cat was still not allowed outdoors. Slight lameness was evident when the cat moved freely on the floor. There was no pain or swelling in the affected area during palpation, and the ROM had improved, but it was still reduced compared to the opposite limb (left extension 163° and flexion 30°). The cat was anesthetized as previously for orthogonal radiographs (Fig. 3a and 3b). DiscussionTo the authors’ knowledge, this is the first reported “Hawkins type 3” talar neck fracture in a cat. Hawkins initially described talar neck fracture in humans based on initial fracture displacement: type I indicates a nondisplaced fracture; type II, a displaced subtalar joint (subluxated or dislocated); and type III, a dislocated tibiotalar joint (Hawkins LG, 1970), which was later modified by Canale and Kelly (1978) and Vallier et al. (2014). There is currently no classification scheme for talar fractures in small animals, probably due to their rarity. So far, cat talar neck fractures have been reported as minimally displaced or with luxation of the talar head (DeCamp et al., 2016). Reported treatment options for talar neck fractures include casts for non-displaced fractures, counter sunken pins and lag screws protected with a lateral splint or an external fixator, or solely by external fixators (Denny, 1993; McCartney and Carmichael, 2000; DeCamp et al., 2016).
Fig. 3. (A and B) Mediolateral and craniocaudal digital radiographs of the left hock joint. The fracture line is still evident. The yellow straight arrow points to the lateral calcaneoquartal joint, where a lack of bone is observed, believed to be due to a loose pin related to complications after the cat escaped the owner. Nevertheless, there was no pain or instability during palpation. This area can also be seen in Figure 2. The area appears larger in Figure 3b, likely due to slight angulation differences between the two radiographs. Considering Halsted’s principles of surgery, special attention was given to the soft tissue, particularly the vasculature and collateral support, when planning this surgery (Cushing, 1922). Due to the nature of the fracture in this cat, assessing the state of the collateral support was difficult. However, disruption was anticipated, so a type 1b external fixator was chosen, as loss of collateral stability in the tarsocrural joint in cats has been successfully treated with external fixators (Kulendra et al., 2011; Jaeger et al., 2005). Although the initial plan was a closed reduction, this was converted to a minimally invasive approach. In humans, Hawkins type 3 fracture is typically treated with open surgery and internal fixations (Buza and Leucht, 2018). In this instance, the decision was made to reject the lag screw due to concerns that motion between the talus and calcaneus could potentially lead to either a fractured screw or loosening (McCartney and Carmichael, 2000). One previous case series of five cats with talar neck fractures did not encounter any complications, utilizing only an external fixator in four of the cats (McCartney and Carmichael, 2000). In this case, complications were encountered; the pin, which came loose after the cat escaped the owner, was replaced and is not believed to have interfered with the outcome. Furthermore, the reduced ROM could result from the prolonged immobilization of the joint. Prolonged immobilization of joints is considered detrimental and predisposes to joint stiffness (Jurvelin et al., 1986; 1989; Haapala et al., 1999). Preliminary studies using hinged transarticular external fixators have shown promising results to hinder this process (Jaeger et al., 2005). As a result of various injuries and potential intra-articular damage from the initial injury, combined with prolonged joint immobilization, might be the combined cause of reduced ROM and potentially lead to arthritis (Fournier et al., 2012; Haverkort et al., 2015). Nonetheless, based on the last radiographs, there is no indication of the development of arthritis, meaning that joint mobility could improve as time progresses and the cat is outdoors. Avascular necrosis and post-traumatic arthritis are common complications of Hawkins type 3 talar neck fractures in humans (Fournier et al., 2012; Vallier et al., 2014; Haverkort et al., 2015; John A Buza and Leucht, 2018). In cats, the main blood supply to the talus comes from branches of the dorsal pedal artery, with an array of intraosseous and extraosseous anastomoses (Barnes, 1993). Previously, it was believed that humans shared a similar blood supply; however, recent studies have revealed that most of the blood supply in humans derives from the posterior tibial artery. This discovery might explain some inconsistencies in human treatment outcomes (Miller et al., 2011). In this case, as in previous published cases, the fracture cause was of unknown origin. However, all were closed fractures (McCartney and Carmichael, 2000), meaning that we can only speculate on the mechanism of the injury. In humans, it is considered that hyperdorsal flexion of the foot on the leg causes talar neck impingement against the anterior distal tibia, causing the fracture. If the force continuous, the talar body dislocates posterior medial and rotates around the medial collateral ligament (Peterson et al., 1976; Kapoor and Patra, 2011). Whether this mechanism applies to cats is unknown, yet it is a plausible theory based on pre-operative radiographs. ConclusionThis case adds to previous cases in cats with talar neck fractures, demonstrating that ESF provides fracture stability, preserves soft tissue, and is simple and well-tolerated. Additionally, the option for disabling the fixation and when the fracture has healed, there are no concerns for future implant issues. AcknowledgmentAniCura Jeløy Dyresykehus for the support. Conflict of interestThe author declares that there is no conflict of interest. Authors’ contributionJon Andre Berg was the single author of the case. FundingThis case report was privately funded. Data availabilityAll data supporting the findings of this study are available within the manuscript. ReferencesBarnes, J. 1993. Cardiovascular System, In: Hudson, L. and Hamilton, W. Eds., Atlas of Feline Anatomy for Veterinarians. Saunders, St. Louis, USA, pp: 103–105. Buza, J.A. and Leucht, P. 2018. Fractures of the talus: current concepts and new developments. Foot Ankle Surg. 24, 282–290. Canale, S.T. and Kelly, F.B.Jr. 1978. Fractures of the neck of the talus. Long-term evaluation of seventy-one cases. J. Bone Joint Surg. 60, 146–156. Carmichael, S. and Marshall, William.G. 2018. Tarsus ans Metatarsus, In: Veterinary Surgery Small Animals. Eds., Johnston, Spencer.A., Tobias and Karen.M. St. Louis, MO: Elsevier, pp: 1193–1209. Cook, J.L., Evans, R., Conzemius, M.G., Lascelles, B.D.X., McIlwraith, C.W., Pozzi, A., Clegg, P., Innes, J., Schulz, K., Houlton, J., Fortier, L., Cross, A.R., Hayashi, K., Kapatkin, A., Brown, D.C. and Stewart, A. 2010. Proposed definitions and criteria for reporting time frame, outcome, and complications for clinical orthopedic studies in veterinary medicine. Vet. Surg. 39, 905–908. Cushing, H. 1922. William Stewart Halsted, 1852-1922. Proceedings of the American Academy of Arts and Sciences, Washington, D.C., USA, 58, 599–604. DeCamp, Charles.E., Johnston, Spencer.A., Dejardin, Lóíc.M. and Schaefer, Susan.L. 2016. Fractures and other orthopaedic injuries of the Tarsus, Metatarsus and Phalanges, In: Brinker, Piermattei and Flo’s Handbook of Small Animal Orthopaedics and Fracture Repair. Ed., DeCamp, C.E Elsevier, St. Louis pp: 730–731. , Denny, H.R. 1993. The hind limb, in: A Guide to Canine and Feline Ortopaedic Surgery. Oxford, UK: Blackwell Scientific Publications, pp: 284–393. Fournier, A., Barba, N., Steiger, V., Lourdais, A., Frin, J.M., Williams, T., Falaise, V., Pineau, V., Salle de Chou, E., Noailles, T., Carvalhana, G., Ruhlmann, F. and Huten, D. 2012. Total talar fracture—Long-term results of internal fixation of talar fractures. A multicentric study of 114 cases. Orthop. Traumatol. Surg. Res. 98(4 Suppl), S48–55. Haapala, J., Arokoski, J.P.A., Hyttinen, M.M., Lammi, M., Tammi, M., Kovanen, V., Helminen, H.J. and Kiviranta, I. 1999. Remobilisation does not fully restore immobilisation induced articular cartilage atrophy. Clin. Orthop. Relat. Res. 362, 218–229. Haverkort, J.J.M., Leenen, L.P.H. and Wessem, K.J.P. van 2015. Diagnosis and treatment of talar dislocation fractures illustrated by 3 case reports and review of literature. Int. J. Surg. Case Rep. 16, 106–111. Hawkins, L.G. 1970. Fractures of the neck of the talus. J Bone Joint Surg Am 52, 991–1002. Jaeger, G., Marcellin-Little, D., DePuy, V. and Lascelles, B. 2007. Validity of goniometric joint measurements in cats. Am. J. Vet. Res. 68, 822–826. Jaeger, G.H., Wosar, M.A., Marcellin-Little, D.J. and Lascelles, B.D.X. 2005. Use of hinged transarticular external fixation for adjunctive joint stabilisation in dogs and cats: 14 cases (1999-2003). J. Am. Vet. Med. Assoc. 227, 586–591. Jurvelin, J., Kiviranta, I., Säämänen, A. -M, Tammi, M. and Helminen, H.J. 1989. Partial restoration of immobilisation-induced softening of canine articular cartilage after remobilisation of the knee (stifle) joint. J. Orthop. Res. 7, 352–358. Jurvelin, J., Kiviranta, I., Tammi, M. and Helminen, J.H. 1986. Softening of canine articular cartilage after immobilisation of the knee joint. Clin. Orthop. Relat. Res. 207, 246–252. Kapoor, S.K. and Patra, S.R. 2011. Talar neck fracture associated with talonavicular dislocation and fracture of posteromedial process of Talus. J. Foot Ankle Surg. 50, 758–761. Kraus, K.H., Toombs, J.P. and Ness, M.G. 2003. External fixation in small animal practice, 1st ed. J. Feline Med. Surg. Oxford, UK: Blackwell Science Ltd. Kulendra, E., Grierson, J., Okushima, S., Cariou, M. and House, A. 2011. Evaluation of the transarticular external skeletal fixator for the treatment of tarsocrural instability in 32 cats. Vet. Comp. Orthop. Traumatol. 24, 320–325. Lahunta, H.E. and A. de, Howard E. Evans, Lahunta, A. de 2013. Miller’s Anatomy of the Dog, 4th ed. St. Louis, MO: Elsever, Saunders. Lee, C., Brodke, D., Perdue, P.W. and Patel, T. 2020. Talus fractures: evaluation and treatment. J. Am. Acad. Orthop. Surg. 28, e878–e887. McCartney, W.T. and Carmichael, S. 2000. Talar neck fractures in five cats. J. Small Anim. Pract. 41, 204–206. Miller, A.N., Prasarn, M.L., Dyke, J.P., Helfet, D.L. and Lorich, D.G. 2011. Quantitative assessment of the vascularity of the Talus with gadolinium-enhanced magnetic resonance imaging. J. Bone Joint Surg. 93, 1116–1121. Palmer, R.H. 1999. Biological osteosynthesis. Vet. Clin. North Am. Small Anim. Pract. 29, 1171–1185. Peterson, L., Romanus, B. and Dahlberg, E. 1976. Fracture of the collum tali—an experimental study. J. Biomech. 9, 277–279. Piermattei, D., Flo, G. and DeCamp, C. 2006. Handbook of Small Animal Orthopedics and Fracture Repair, 4th ed. Saunders, Philadelphia, PA: Vallier, H.A., Reichard, S.G., Boyd, A.J. and Moore, T.A. 2014. A new look at the Hawkins classification for Talar neck fractures: which features of injury and treatment are predictive of osteonecrosis? J. Bone Joint Surg. 96, 192–197. Vollmerhausl, B., Roos, H., Matis, U., Blümp, U. and Fischer, H. 2002a. Zur klinisch-angewandten und funktionellen Anatomie des Sprunggelenks der Hauskatze. Teil 1: Tarsalskelett. Teil 1: Tarsalskelett. Tierärztl. Prax. 30, 131–137. Vollmerhausl, B., Roos, H., Matis, U., Blümp, U. and Fischer, H. 2002b. Zur klinisch-angewandten und funktionellen Anatomie des Sprunggelenks der Hauskatze. Teil 2: Gelenke, Bänder, Muskeln des Tarsus. Tierärztl. Prax. 30, 202–210. von Knoch, F., Reckord, U., von Knoch, M. and Sommer, C. 2007. Fracture of the lateral process of the talus in snowboarders. J. Bone Joint Surg. 89, 772–777. Young, R.P., Scott, S.H. and Loeb, G.E. 1993. The distal hindlimb musculature of the cat: multiaxis moment arms at the ankle joint. Exp. Brain Res. 96, 141–151. | ||
| How to Cite this Article |
| Pubmed Style Jon Andre Berg. A rare case of “Hawkins type 3” talar neck fracture in a cat. Open Vet. J.. 2024; 14(8): 2110-2115. doi:10.5455/OVJ.2024.v14.i8.41 Web Style Jon Andre Berg. A rare case of “Hawkins type 3” talar neck fracture in a cat. https://www.openveterinaryjournal.com/?mno=206595 [Access: October 22, 2025]. doi:10.5455/OVJ.2024.v14.i8.41 AMA (American Medical Association) Style Jon Andre Berg. A rare case of “Hawkins type 3” talar neck fracture in a cat. Open Vet. J.. 2024; 14(8): 2110-2115. doi:10.5455/OVJ.2024.v14.i8.41 Vancouver/ICMJE Style Jon Andre Berg. A rare case of “Hawkins type 3” talar neck fracture in a cat. Open Vet. J.. (2024), [cited October 22, 2025]; 14(8): 2110-2115. doi:10.5455/OVJ.2024.v14.i8.41 Harvard Style Jon Andre Berg (2024) A rare case of “Hawkins type 3” talar neck fracture in a cat. Open Vet. J., 14 (8), 2110-2115. doi:10.5455/OVJ.2024.v14.i8.41 Turabian Style Jon Andre Berg. 2024. A rare case of “Hawkins type 3” talar neck fracture in a cat. Open Veterinary Journal, 14 (8), 2110-2115. doi:10.5455/OVJ.2024.v14.i8.41 Chicago Style Jon Andre Berg. "A rare case of “Hawkins type 3” talar neck fracture in a cat." Open Veterinary Journal 14 (2024), 2110-2115. doi:10.5455/OVJ.2024.v14.i8.41 MLA (The Modern Language Association) Style Jon Andre Berg. "A rare case of “Hawkins type 3” talar neck fracture in a cat." Open Veterinary Journal 14.8 (2024), 2110-2115. Print. doi:10.5455/OVJ.2024.v14.i8.41 APA (American Psychological Association) Style Jon Andre Berg (2024) A rare case of “Hawkins type 3” talar neck fracture in a cat. Open Veterinary Journal, 14 (8), 2110-2115. doi:10.5455/OVJ.2024.v14.i8.41 |