| Short Communication | ||
Open Vet. J.. 2025; 15(6): 2915-2918 Open Veterinary Journal, (2025), Vol. 15(6): 2915-2918 Short Communication A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopyElizabeth Alvey1, Langdon Fielding1*, Dustin Dennis1, Diane Rhodes1, Emma Deane1 and Jessica Bouton11Loomis Basin Equine Medical Center, Penryn, CA *Correspondence to: Langdon Fielding. Loomis Basin Equine Medical Center, Penryn, California, USA. Email: lfielding [at] lbemc.com Submitted: 07/03/2025 Revised: 11/05/2025 Accepted: 13/05/2025 Published: 30/06/2025 © 2025 Open Veterinary Journal
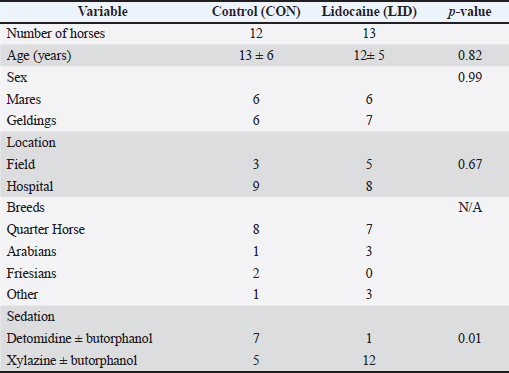
AbstractBackground: Intranasal lidocaine (LID) administration is a common treatment used to facilitate the passing of endoscopes and nasogastric tubes in horses. However, no research has supported its use in equine practice. Aim: To compare patient reactivity and endoscope passage time between intranasal LID and intranasal saline prior to gastroscopy. Methods: This blinded, randomized clinical trial included 25 horses presenting for gastroscopy. Following the administration of sedation and prior to gastroscopy, 10 ml of saline (CON) was administered intranasally to 12 horses in the control group, or 10 ml of 2% LID was administered intranasally to 13 horses in the LID group. The recorded data included signalment, location of scoping (field or hospital), sedation, grade of reactivity on a 6-point scale (0 for no reactivity up to five when the scope could not be passed), and time to passage from the nares to the cardia. Results: The time to reach the cardia in the CON group was 73 (35–183) seconds, and the time to reach the cardia in the LID group was 70 (45–210) seconds (p = 0.8). The number of horses with a reactivity grade less than or equal to 1 in the CON group was 75% (9/12) compared with 69% (9/13) in the LID group (p = 0.12). Conclusion: This small study did not identify any significant benefit from administering intranasal LID prior to endoscope passage. Keywords: Nasogastric, Endoscopy, Nasal passage. IntroductionPassing a nasogastric tube or endoscope through the nostrils is one of the most common emergency procedures in equine veterinary medicine and takes place in both hospital and ambulatory practice (Blikslager, 2020, van den Boom, 2022). Horses are often reactive despite sedation, and additional physical restraint (e.g., nose twitch) is sometimes required. In the authors’ experience, horses tend to be most reactive to the passage of the endoscope or nasogastric tube at the external nares and through the ventral meatus. Reactions may include raising the head, backing up, extending the neck, rearing, or striking. Complications associated with the procedure include epistaxis, mucosal irritation, and pharyngeal or esophageal trauma (Hardy et al., 1992; Trim et al., 1997). Lidocaine (LID) is a common local anesthetic used for many applications in equine medicine. Topical LID has been shown to reduce the discomfort of intramuscular injection in horses, reduce thermal nociception and mechanical sensation, and reduce corneal sensitivity (Regnier et al., 2018; Söbbeler and Kästner, 2018; Torcivia and McDonnell 2022). LID can also be nebulized in horses as a treatment for asthma (Minuto et al., 2022). Some practitioners use intranasal LID prior to passing a nasogastric tube or endoscope with the hope of decreasing reactivity and discomfort. Currently, no study has assessed the efficacy of intranasal LID in equine veterinary medicine. Intranasal LID has been studied in human medicine, and its application before nasogastric tube insertion has been shown to decrease discomfort (Cullen et al., 2004, Lor et al., 2018). A clinical trial showed that nebulized LID improved the comfort of human patients based on a visual analog scale (Cullen et al., 2004). It would seem logical that similar benefits would exist in horses when using intranasal LID before passing a nasogastric tube or endoscope. The objective of this study was to evaluate whether intranasal LID administered before gastroscopy has an effect on the reactivity of equine patients and improves the speed at which the endoscope can be passed easily. We hypothesized that compared with saline, intranasal LID prior to the passage of an endoscope through the nasal passage would decrease the reactivity of equine patients during the procedure. We also hypothesized that compared with saline, intranasal LID would decrease the time of endoscope travel from the nostril to the cardia. Materials and MethodsA randomized, blinded, controlled clinical trial was performed with 25 horses (12 control horses and 13 LID horses) to compare intranasal LID with intranasal saline. The study took place at the Loomis Basin Equine Medical Center and included patients who presented for gastroscopy in both the hospital and field settings. The study was approved by the hospital review board, and client consent was obtained for each animal. All personnel participating in the clinical part of the study were blinded to the treatment group. The treatment group was randomly assigned using a random number generator in the order in which horses were enrolled in the study. A pharmacy staff member prepared the study medication (saline or LID) and did not participate in any clinical aspects of the study. No person who created the randomization or drew up the medication was involved in carrying out the study protocol. Prior to participation in the study, client consent was obtained for each patient. Individual horses were assigned to the control (CON) group or the treatment (LID) group. In all cases, the horses were sedated following physical examination. The sedation dose was selected based on the discretion of the senior clinician and recorded. Xylazine, detomidine hydrochloride, xylazine and butorphanol, or detomidine and butorphanol were administered intravenously for sedation. Approximately 5 minutes following sedation, 10 ml of the study solution (saline or 2% LID) was administered into one nostril (left or right) using a 12 ml syringe that was inserted as far into the nostril as the horse would tolerate. The average horse in this group would require approximately 0.4 mg/kg of intranasal LID. The endoscope was passed within 5 minutes after the intranasal infusion of solution (LID vs. saline). In most cases, two or three individuals participated in the procedure with either one person holding the horse, one person driving the endoscope, and one person passing the endoscope or with one person driving the endoscope and one person holding the horse and passing the endoscope. Reactivity was assessed based on a 6-point scale (0–5): No reaction (0), mild lifting of the head (1), additional physical restraint required (2), additional chemical restraint required (3), additional chemical and physical restraint required (4), and scope could not be performed (5). The senior clinician selected the grade following the completion of the gastroscopy procedure. Additional chemical restraint was defined as an additional dose of sedation, while additional physical restraint was defined as a nose or skin twitch. As a more objective measure of the efficacy of intranasal LID, a timer was used to record the time from the introduction of the endoscope into the nares to the time the endoscope reached the cardia. Other data recorded included complications during or following gastroscopy if the individual had undergone gastroscopy before this study and gastroscopy findings. Data were assessed for normality using the Kolmogorov–Smirnov test. Normally distributed variables were reported as mean ± SD, and non-normally distributed variables were reported as median (range). To assess the efficacy of randomization, signalment variables were compared before treatment using the t-test (normally distributed) or Mann–Whitney test (not normally distributed). Categorical variables were compared using Fisher’s exact test. To determine treatment effects, the two groups were compared using a Mann–Whitney test for continuous variables and Fisher’s exact test for categorical variables. Due to the sedation differences following randomization, a post hoc analysis of the subgroup of horses that received xylazine was performed. This subgroup of xylazine horses used a more evenly distributed sedation protocol. A commercially available software was used for the analysis (GraphPad Prism version 8.2.1 for Windows, GraphPad Software, La Jolla, CA) and p < 0.05 was considered statistically significant. Results and DiscussionThe pretreatment characteristics of the horses are shown in Table 1. There were no significant differences between the two study groups in terms of sex or setting (field vs. hospital). However, a larger number of horses (seven horses) in the CON group received detomidine compared with the LID group (one horse) as part of the sedation protocol. The mean age of the horses in the study was 12 (4–27) years, and 12 mares and 13 geldings were included in the study. Table 1. Pretreatment characteristics of the CON (intranasal saline) and LID (intranasal lidocaine) groups.
The time to reach the cardia in the CON group was 73 (35–183) seconds, and the time to reach the cardia in the LID group was 70 (45–210) seconds (p = 0.8). The number of horses with a reactivity grade less than or equal to 1 in the CON group was 75% (9/12) compared with 69% (9/13) in the LID group (p = 0.12). Only one horse in the LID group required additional sedation with additional physical restraint, whereas no horses in the CON group required additional sedation or restraint. Both the CON and LID groups had three horses that had a reactivity of grade 2 (required additional physical restraint). In the subgroup post hoc analysis of horses receiving xylazine, five horses received intranasal saline, and the time to reach the cardia was 76 seconds (70–183) as compared to 12 horses that received intranasal LID and the time to reach the cardia was 70 seconds (45–210) (p = 0.17). This study showed no difference between the LID and CON groups regarding the speed of endoscope passage during gastroscopy and level of reactivity. Despite blinding and randomization, more horses in the CON group received detomidine for sedation. Although further research is needed, these findings do not support the use of intranasal LID prior to the passing of the endoscope. For reactivity, the majority of individuals were grade 1 (mild lifting of the head) during the procedure. Overall, few horses required additional sedation or physical restraint. This highlights the importance of appropriate sedation administered prior to intubation and endoscopy, and it could have minimized the effect of the local anesthetic. While previous studies have shown LID to be an effective local anesthetic, the use of intranasal LID for this procedure may not be useful (Regnier et al., 2018, Söbbeler and Kästner, 2018, Torcivia and McDonnell, 2022). A study on human medicine showed that nebulized LID administered before nasogastric intubation decreased discomfort in patients (Cullen et al., 2004). However, the lengths of the equine and human nasal cavities are different, and effectively decreasing sensitization of the nasal cavity may prove more difficult in equine patients due to anatomical differences. Using different concentrations of LID might have also yielded different results (Torcivia and McDonnell, 2022). The reactivity scale chosen for this study was simple and easy to use, with an objective categorization of reactions. This allowed for clarity for clinicians utilizing the grading scale more clearly. Because many horses were given a grade 1 reactivity, further studies could investigate a larger point scale to differentiate between individuals within grade 1 reactivity. The individuals scoping the horses in this study were quite experienced, and many of them had scoped hundreds of horses. It is possible that the results of this study would have been different with less experienced veterinarians or technicians. LID administration might be more important when the individual passing the scope is less efficient. A power calculation was used to estimate the sample size required to find statistically significant differences based on the data from this study. Given the time to reach the cardia in the control group of 83 ± 40 seconds, power of 80%, and an alpha of 0.05, a total of 56 horses would need to be enrolled in the study to detect a 30-second improvement in the passage of the gastroscope to the cardia. The much smaller difference observed in the current study suggests that a large-scale study is needed to find a significant difference if one exists. Another limitation of this study was the lack of standardization of sedation. Each dose and medication selection was dependent on the senior clinicians who participated in the study. Different drugs and doses were used prior to the intranasal infusion of the solution, which could have affected the results. The grade/level of sedation was not recorded following the administration of sedation, and the level of sedation was therefore variable between individuals. Randomization was not effective in this study for sedation given that the saline group had a much larger number of horses sedated with detomidine. However, the subgroup analysis of the xylazine group was also not able to demonstrate a significant difference between the groups, suggesting that the results are robust and may not have been heavily influenced by the choice of sedation. The second limitation of this study was the variation in the number of personnel passing and conducting the gastroscopy. The individual technique could have affected the reactivity of the individual to the endoscope, and individual skill/technique could have affected the speed from external nares to the cardia. ConclusionThis study did not reveal any significant benefit of intranasal LID use prior to endoscope passage. Further studies with more patients are needed to identify a statistically significant benefit of LID administration if one exists. The sedation protocol and personnel may be more important than the local anesthetic. AcknowledgmentsNone. FundingNo funding sources. Authors’ contributionsAll authors were involved in study design and data collection. Dr. Alvey and Dr. Fielding performed the data analysis and manuscript preparation. All authors were involved in manuscript revision and approval. Conflict of interestThe authors declare no conflicts of interest. Data availabilityAll data are available in the manuscript as follows. ReferencesBlikslager, A. 2020. How to manage a horse with colic in the field. In the proceedings of the American Association of Equine Practitioners. Washington, DC pp: 115–118. Cullen, L., Taylor, D., Taylor, S. and Chu, K. 2004. Nebulized lidocaine decreases the discomfort of nasogastric tube insertion: a randomized, doubleblind trial. Ann. Emerg. Med. 44, 131–137. Hardy, J., Stewart, R.H., Beard, W.L. and Yvorchuk-St-Jean, K. 1992. Complications of nasogastric intubation in horses: nine cases (1987-1989). J. Am. Vet. Med. Assoc. 201, 483–486. Lor, Y.C., Shih, P.C., Chen, H.H., Liu, S.J., Chao, H.C., Hwang, L.C., Hsu, Y.F. and Yeh, T.L. 2018. The application of lidocaine to alleviate the discomfort of nasogastric tube insertion: a systematic review and meta-analysis. Medicine (Baltimore) 97, e9746. Minuto, J., Bedenice, D., Ceresia, M., Zaghloul, I., Böhlke, M. and Mazan, M.R. 2022. Clinical effects and pharmacokinetics of nebulized lidocaine in healthy horses. Front. Vet. Sci. 15(9), 984108. Regnier, A., Berton, I., Concordet, D. and Douet, J.Y. 2018. Effect of topical application of 2% lidocaine gel on corneal sensitivity of clinically normal equine eyes. Vet. Anaesth. Analg. 45, 158–164. Söbbeler, F.J. and Kästner, S.B. 2018. Effects of transdermal lidocaine or lidocaine with prilocaine or tetracaine on mechanical superficial sensation and nociceptive thermal thresholds in horses. Vet.Anaesth. Analg. 45, 227–233. Torcivia, C. and McDonnell, S. 2022. Efficacy of lidocaine topical solution in reducing discomfort reaction of horses to intramuscular vaccination. Animals 12, 1659. Trim, C.M., Eaton, S.A. and Parks, A.H. 1997. Severe nasal hemorrhage in an anesthetized horse. J. Am. Vet. Med. Assoc. 210, 1324–1327. van den Boom, R. 2022. Equine gastric ulcer syndrome in adult horses. Vet. J. 283, 105830. | ||
| How to Cite this Article |
| Pubmed Style Alvey E, Fielding L, Dennis D, Rhodes D, Deane E, Bouton J. A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy. Open Vet. J.. 2025; 15(6): 2915-2918. doi:10.5455/OVJ.2025.v15.i6.62 Web Style Alvey E, Fielding L, Dennis D, Rhodes D, Deane E, Bouton J. A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy. https://www.openveterinaryjournal.com/?mno=246194 [Access: January 25, 2026]. doi:10.5455/OVJ.2025.v15.i6.62 AMA (American Medical Association) Style Alvey E, Fielding L, Dennis D, Rhodes D, Deane E, Bouton J. A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy. Open Vet. J.. 2025; 15(6): 2915-2918. doi:10.5455/OVJ.2025.v15.i6.62 Vancouver/ICMJE Style Alvey E, Fielding L, Dennis D, Rhodes D, Deane E, Bouton J. A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy. Open Vet. J.. (2025), [cited January 25, 2026]; 15(6): 2915-2918. doi:10.5455/OVJ.2025.v15.i6.62 Harvard Style Alvey, E., Fielding, . L., Dennis, . D., Rhodes, . D., Deane, . E. & Bouton, . J. (2025) A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy. Open Vet. J., 15 (6), 2915-2918. doi:10.5455/OVJ.2025.v15.i6.62 Turabian Style Alvey, Elizabeth, Langdon Fielding, Dustin Dennis, Diane Rhodes, Emma Deane, and Jessica Bouton. 2025. A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy. Open Veterinary Journal, 15 (6), 2915-2918. doi:10.5455/OVJ.2025.v15.i6.62 Chicago Style Alvey, Elizabeth, Langdon Fielding, Dustin Dennis, Diane Rhodes, Emma Deane, and Jessica Bouton. "A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy." Open Veterinary Journal 15 (2025), 2915-2918. doi:10.5455/OVJ.2025.v15.i6.62 MLA (The Modern Language Association) Style Alvey, Elizabeth, Langdon Fielding, Dustin Dennis, Diane Rhodes, Emma Deane, and Jessica Bouton. "A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy." Open Veterinary Journal 15.6 (2025), 2915-2918. Print. doi:10.5455/OVJ.2025.v15.i6.62 APA (American Psychological Association) Style Alvey, E., Fielding, . L., Dennis, . D., Rhodes, . D., Deane, . E. & Bouton, . J. (2025) A randomized clinical trial comparing intranasal lidocaine and saline prior to gastroscopy. Open Veterinary Journal, 15 (6), 2915-2918. doi:10.5455/OVJ.2025.v15.i6.62 |