| Case Report | ||
Open Vet. J.. 2021; 11(4): 728-733 Open Veterinary Journal, (2021), Vol. 11(4): 728–733 Case Report Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dogYuma Tomo, Erina Sobashima, Hinano Eto, Atsushi Yamazaki, Koji Tanegashima and Kazuya Edamura*Laboratory of Veterinary Surgery, Department of Veterinary Medicine, College of Bioresource and Sciences, Nihon University, Fujisawa, Japan *Corresponding Author: Kazuya Edamura. Laboratory of Veterinary Surgery, Department of Veterinary Medicine, College of Bioresource and Sciences, Nihon University, Fujisawa, Japan. Email: edamura.kazuya [at] nihon-u.ac.jp Submitted: 04/06/2021 Accepted: 25/11/2021 Published: 20/12/2021 © 2021 Open Veterinary Journal
AbstractBackground: In recent years, surgical site infections caused by drug-resistant pathogens have emerged as a cause of concern in small animal practice. In this report, methicillin-resistant Staphylococcus aureus (MRSA) infections associated with tibial plateau leveling osteotomy (TPLO) is reported. However, there have been no reports on the treatment of MRSA infection following TPLO in dogs. This case report describes the use of a combination of vancomycin and rifampicin to treat MRSA infection following TPLO in a dog. Case Description: A 7-year-old spayed female American cocker spaniel was referred for right hind limb lameness that did not improve with conservative treatment. The dog was diagnosed with cranial cruciate ligament rupture, for which TPLO was performed. Once the surgical wound was closed, the dog licked the skin on the surgical site, causing the injury to dehisce. MRSA was detected from the purulent discharge, and chloramphenicol was then administered based on the drug sensitivity test results. Because of the continued drainage, the implants were removed after the bone union of the osteotomy site was observed. Since this did not provide any relief to the existing condition, the antibiotic was changed to vancomycin at 132 days after TPLO surgery, and the infected location was cleaned many times through a drain tube placed into the tibia. However, the infection could not be controlled. Thus, a rifampicin and vancomycin combination was started. As a result, the purulent discharge disappeared and the fistula entirely closed on the 154th day after TPLO surgery. Conclusion: A combination of rifampicin and vancomycin may be effective for treating MRSA infection at the surgical site following TPLO surgery that does not heal despite implant removal and administration of vancomycin. Keywords: Dog, Infection, MRSA, Rifampicin, TPLO. IntroductionCranial cruciate ligament (CrCL) rupture is one of the most common causes of hind limb lameness in dogs (Canapp, 2007). Surgical interventions for CrCL rupture include intracapsular and extracapsular reconstruction techniques and corrective osteotomy (Bergh et al., 2014). In recent years, the number of surgeons preferring a tibial plateau leveling osteotomy (TPLO) has increased because of its excellent long-term outcome and a higher rate of owner satisfaction (Nanda and Hans, 2019). The complications of TPLO include surgical site infection (SSI), meniscal injury, tibial tuberosity fracture, and implant failure, which reportedly occur in 10%–34% of the cases (Bergh and Peirone, 2012). The estimated incidence of SSI following TPLO is between 2.9% and 25.9% (Hagen et al., 2020). Bacterial pathogens such as Staphylococcus pseudintermedius, coagulase-negative Staphylococci spp., and Pseudomonas aeruginosa are reportedly responsible for TPLO-related SSI (Savicky et al., 2013). In recent years, SSI caused by drug-resistant bacteria has emerged as a cause of concern in small animal practice, and episodes of methicillin-resistant Staphylococcus aureus (MRSA) infections associated with TPLO were reported (Savicky et al., 2013; Stine et al., 2018). To our knowledge, there have been no reports on the treatment of MRSA infection following TPLO in dogs. Therefore, this case report describes the use of a combination of vancomycin and rifampicin to treat MRSA infection following TPLO, in which an excellent clinical outcome was achieved. Case DetailsA 7-year-old spayed female American cocker spaniel, weighing 11.2 kg, presented to the primary veterinary hospital with a chief complaint of acute right hind limb lameness. The dog was treated with meloxicam (0.1 mg/kg) for 3 weeks; however, the lameness did not improve. Therefore, the dog was referred to the Animal Medical Center of Nihon University. During the initial visit to our hospital, the dog presented with non-weight-bearing lameness of the right hind limb. An orthopedic examination of the right hind limb revealed positivity for both the tibial compression and cranial drawer tests. Radiography of the right hind limb showed cranial displacement of the tibia, formation of osteophytes, and fat pad sign in the stifle joint. Based on these findings, the dog was diagnosed with CrCL rupture. TPLO surgery was recommended to the owner to treat CrCL rupture, and consent was obtained from the owner. At the surgery, the dog was premedicated with atropine sulfate (0.04 mg/kg) subcutaneously and fentanyl citrate (5 μg/kg) intravenously. Subsequently, anesthesia was induced by intravenous administration of propofol (4 mg/kg). After intubation, anesthesia was maintained using isoflurane. Perioperative analgesia was provided by administering meloxicam (0.1 mg/kg) subcutaneously and fentanyl citrate (5–10 μg/kg/hour, constant rate infusion) intravenously. An intravenous dose of cefazolin (20 mg/kg) was initiated at the time of anesthesia and administered thereafter every 120 minutes during the surgery. The disinfected limb was first covered with a surgical drape, followed by an antimicrobial incise drape (Ioban; 3M, St. Paul, MN). The CrCL rupture and medial meniscus injury were identified and treated with arthroscopy. Subsequently, TPLO was performed using routine procedures. Briefly, the tibia was osteotomized using a TPLO saw blade. The proximal tibia was rotated to a position where the tibial plateau angle was 5°, and the osteotomy site was fixed using a 2.7 mm TPLO plate, 2.7 mm locking head screws, and standard cortex screws (Johnson and Johnson K.K., New Brunswick, NJ). The surgical site was thoroughly washed, closed, and shielded with an adherent dressing sheet (Opsite Flexifix; Smith & Nephew, Hertfordshire, UK). Cefalexin (20 mg/kg) was administered intravenously initially every 8 hours over the next 48 hours and then orally every 12 hours. The dog was discharged from our hospital 7 days after the TPLO surgery and wore an Elizabethan collar until the suture was removed. At 13 days after the TPLO surgery, all sutures were removed as the surgical wound had healed. At 31 days after TPLO surgery, there were no medical issues at the surgical site, and improvement from lameness was observed. At 41 days after TPLO surgery, the dog was brought to our hospital because of licking the surgical site and wound dehiscence (Fig. 1). The dog had weight-bearing lameness with purulent discharge from the wound. Blood examination revealed a marked increase in C-reactive protein level (CRP; 14 mg/dl). The results of the bacteriological culture test revealed MRSA infection. At 49 days after TPLO surgery, based on the drug sensitivity profile, oral administration of chloramphenicol (23 mg/kg) thrice daily was initiated. The infected area was also continually sterilized using 0.02% chlorhexidine gluconate solution. While the symptoms improved temporarily, they deteriorated after that, and purulent discharge was again observed on the lateral side of the cruris.
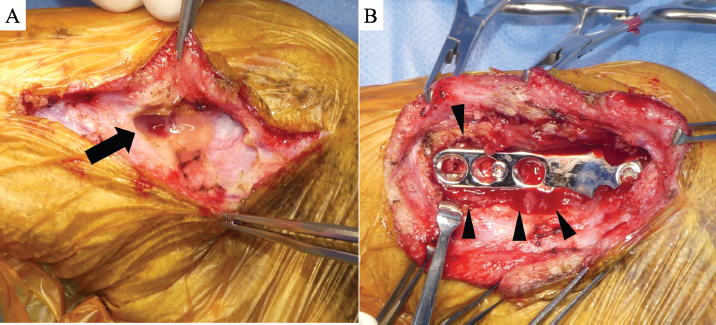
Fig. 1. Gross finding of the surgical site at 41 days after TPLO surgery. The dehiscence of the wound was observed (black arrow). (TPLO): tibial plateau leveling osteotomy.
Fig. 2. Intraoperative findings at implants removal. (A) A subcutaneous fistula tract was formed toward TPLO plate (black arrow). (B) Purulent accumulation was observed around the TPLO plate (black arrowheads). (TPLO): tibial plateau leveling osteotomy.
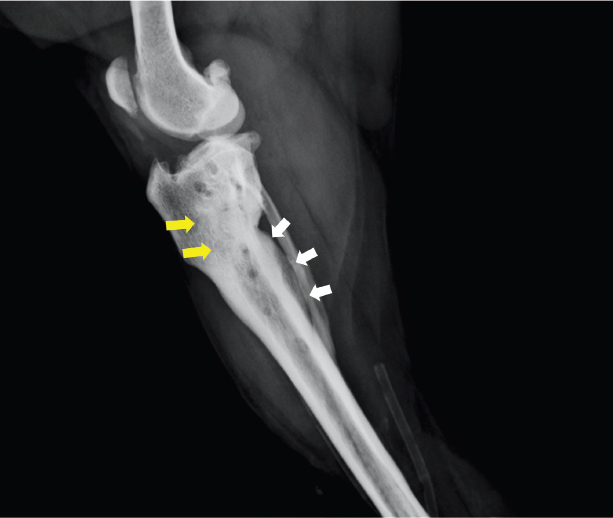
Fig. 3. Lateral view of the right hind limb on radiograph at 132 days after TPLO. An area of high radiolucency in the proximal tibia (yellow arrows) and a periosteal reaction on the caudal side of the tibia (white arrows) were observed. (TPLO): tibial plateau leveling osteotomy.
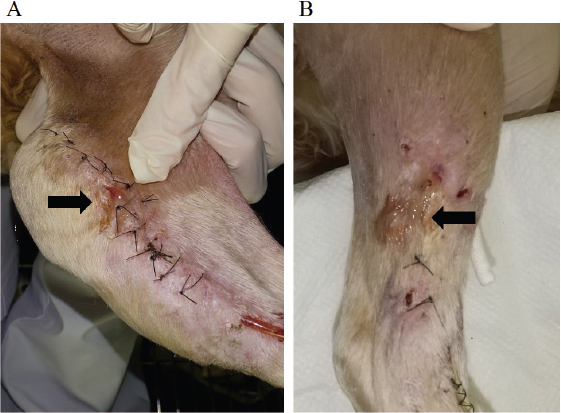
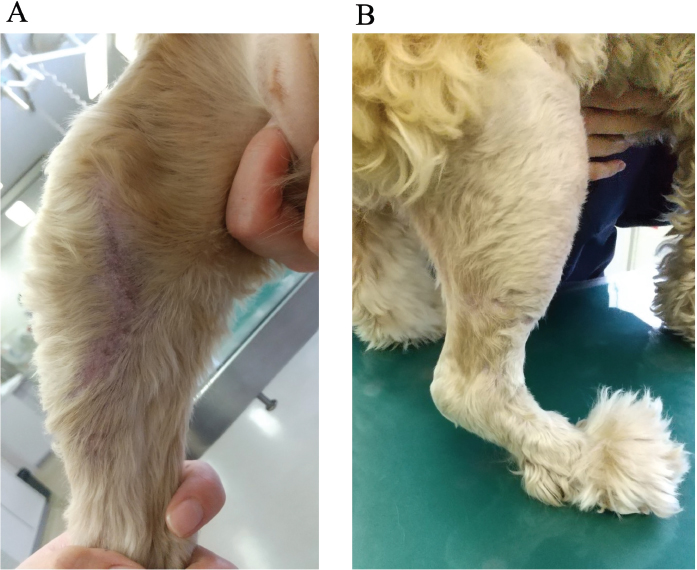
Fig. 4. Gross findings of the surgical site at 145 days after TPLO surgery. (A) Medial aspect. (B) Lateral aspect. Purulent discharge from the surgical site was observed (black arrows). (TPLO): tibial plateau leveling osteotomy. At 117 days after TPLO surgery, since the bone union of the osteotomy site was satisfactorily achieved, the implants were removed under general anesthesia. A subcutaneous fistula tract formation was noted toward the TPLO plate, surrounded by purulent accumulation (Fig. 2). After implant removal, the affected tissue was debrided and thoroughly cleaned using a pulse wound cleaning and debridement system (Pulsavac® Plus; Zimmer Biomet Holdings Inc., St. Warsaw, IN). In addition, the lateral discharge area was debrided. Intraoperatively, the purulent discharge was aseptically collected, and a second drug sensitivity test was carried out. Based on these results, oral administration of trimethoprim-sulfamethoxazole (17 mg/kg) once a daily was initiated, and chloramphenicol was withdrawn. At 132 days after TPLO surgery, the purulent discharge continued, and the surgical wound was dehisced again. Blood examination again showed a marked increase in CRP level (19 mg/dl). In addition, radiography showed an area of high radiolucency in the proximal tibia and a periosteal reaction on the caudal side of the tibia, suggestive of osteomyelitis (Fig. 3). Thus, lavage of the infected site was carried out under general anesthesia. Furthermore, because of purulent discharge, a drain tube was inserted to penetrate a third screw hole from the distal side. Postoperatively, the antibiotic was changed to an intravenous administration of vancomycin (15 mg/kg) thrice daily, based on the third drug sensitivity test result. Continuous infusion of vancomycin and lavage with saline via a drain tube was carried out for 2 weeks. However, there was no remarkable improvement in the purulent discharge (Fig. 4). Hence, oral administration of rifampicin (13 mg/kg) twice daily was attempted in combination with vancomycin at 145 days after TPLO surgery. Following this, the discharge from the infected site decreased gradually and the lameness disappeared. At 154 days after TPLO surgery, the drain tube was removed. Subsequently, vancomycin was withdrawn and rifampicin was administered for another month. No noticeable side effects were observed in blood tests or physical examinations during or after administering each antibiotic. Finally, the purulent discharge disappeared and the fistula closed completely (Fig. 5). Currently, the dog has no clinical symptoms and is progressing well.
Fig. 5. Gross findings of the surgical site at 178 days after TPLO surgery. (A) Medial aspect. (B) Lateral aspect. Purulent discharge disappeared and the fistula was completely closed. (TPLO): tibial plateau leveling osteotomy. DiscussionThe causes of bacterial infection following TPLO surgery include direct contamination during surgery, pre-existing infection before surgery, and hematogenous infection from distant sources, such as dental disease and endocarditis (Savicky et al., 2013). In the case presented here, the onset of symptoms occurred more than 40 days following TPLO surgery, with no identifiable source of infection. Therefore, it was suspected that the direct cause of wound dehiscence might not be an intraoperative infection but rather an external infection caused by licking the surgical site. The number of reports on antimicrobial-resistant bacterial infections following orthopedic implant placement in dogs have increased (Stine et al., 2018). MRSA and methicillin-resistant S. pseudintermedius were documented as the most common multidrug-resistant pathogens that are responsible for infections associated with TPLO implants (Savicky et al., 2013; Hagen et al., 2020). In this case, MRSA was detected at the site of the infection. MRSA forms biofilms and is resistant to many antibacterial agents (Otto, 2013). The presence of the implant at the site of infection is also a factor that makes infection control difficult (Patel, 2005). Therefore, in the current case, the implants were removed after the osteotomy site achieved bone union. It was suspected that biofilm formation around the TPLO plate and screws was responsible for the deterioration of symptoms in the dog. Vancomycin is reportedly the most effective antimicrobial agent against MRSA infection in dogs (DeStefano et al., 2019). However, in the present case, the purulent discharge did not completely disappear, despite the continuous intravenous administration of vancomycin. This could have been due to mutations in the MRSA during the treatment, leading to resistance to this antibiotic. Recently, the efficacy of rifampicin in combination with other antibiotics was investigated to treat MRSA infections that are difficult to treat with a single antibiotic (Davis et al., 2015). Rifampicin is especially considered active in treating staphylococcal infections and eradicating pathogens located in difficult to reach target areas, such as within phagocytic cells (Guo et al., 2020). To our knowledge, there have been no reports on the efficacy of rifampicin in the treatment of MRSA infection following TPLO. In this case, rifampicin was administered along with vancomycin and was highly effective in suppressing SSI following TPLO. Rifampicin is recommended for use in combination with other systemic antimicrobial agents, as it is prone to the development of bacterial resistance (Papich, 2012). Therefore, combining rifampicin with vancomycin can be an effective option for refractory SSI caused by MRSA after orthopedic surgery, especially when the patient’s symptoms do not improve with the administration of vancomycin alone. This is a valuable case report on the treatment of MRSA infection after TPLO surgery without amputation. However, since only one case has been evaluated, additional investigation in more dogs is required to determine if rifampicin is also effective against MRSA infection after TPLO surgery in males and other breeds. In addition, further studies are needed on the administration method, effective combinations, and dosage of rifampicin for refractory MRSA infection in dogs. The treatment of deep SSI caused by MRSA following TPLO surgery is challenging. If the response to removing the implant and administration of vancomycin alone is poor, a combination of rifampicin and vancomycin may be an effective treatment for MRSA infection. Conflicts of interestThe authors declare that there is no conflict of interest. Authors’ contributionsAll authors conceived and carried out the procedures; drafted and revised the manuscript; and approved the final version of the manuscript. ReferencesBergh, M.S. and Peirone, B. 2012. Complications of tibial plateau leveling osteotomy in dogs. Vet. Comp. Orthop. Traumatol. 25, 349–358. Bergh, M.S., Sullivan, C., Ferrell, C.L., Troy, J. and Budsberg, S.C. 2014. Systematic review of surgical treatments for cranial cruciate ligament disease in dogs. J. Am. Anim. Hosp. Assoc. 50, 315–321. Canapp Jr, S.O. 2007. The canine stifle. Clin. Tech. Small Anim. Pract. 22, 195–205. Davis, J.S., Van Hal, S. and Tong, S.Y.C. 2015. Combination antibiotic treatment of serious methicillin-resistant Staphylococcus aureus infections. Semin. Respir. Crit. Care Med. 36, 3–16. DeStefano, I.M., Wayne, A.S., Rozanski, E.A. and Babyak, J.M. 2019. Parenterally administered vancomycin in 29 dogs and 7 cats (2003-2017). J. Vet. Intern. Med. 33, 200–207. Guo, P., Xue, H.Y., Buttaro, B.A., Tran, N.T. and Wong, H.L. 2020. Enhanced eradication of intracellular and biofilm-residing methicillin-resistant Staphylococcus aureus (MRSA) reservoirs with hybrid nanoparticles delivering rifampicin. Int. J. Pharm. 589, 119784. Hagen, C.R.M., Singh, A., Weese, J.S., Marshall, Q., Linden, A.Z. and Gibson, T.W.G. 2020. Contributing factors to surgical site infection after tibial plateau leveling osteotomy: a follow-up retrospective study. Vet. Surg. 49, 930–939. Nanda, A. and Hans, E.C. 2019. Tibial plateau leveling osteotomy for cranial cruciate ligament rupture in canines: patient selection and reported outcomes. Vet. Med. (Auckl). 10, 249–255. Otto, M. 2013. Staphylococcal infections: mechanisms of biofilm maturation and detachment as critical determinants of pathogenicity. Annu. Rev. Med. 64, 175–188. Papich, M.G. 2012. Selection of antibiotics for meticillin-resistant Staphylococcus pseudintermedius: time to revisit some old drugs? Vet. Dermatol. 23, 352–360. Patel, R. 2005. Biofilms and antimicrobial resistance. Clin. Orthop. Relat. Res. 437, 41–47. Savicky, R., Beale, B., Murtaugh, R., Swiderski-Hazlett, J. and Unis, M. 2013. Outcome following removal of TPLO implants with surgical site infection. Vet. Comp. Orthop. Traumatol. 26, 260–265. Stine, S.L., Odum, S.M. and Mertens, W.D. 2018. Protocol changes to reduce implant-associated infection rate after tibial plateau leveling osteotomy: 703 dogs, 811 TPLO (2006-2014). Vet. Surg. 47, 481–489. | ||
| How to Cite this Article |
| Pubmed Style Tomo Y, Sobashima E, Eto H, Yamazaki A, Tanegashima K, Edamura K. Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog. Open Vet. J.. 2021; 11(4): 728-733. doi:10.5455/OVJ.2021.v11.i4.25 Web Style Tomo Y, Sobashima E, Eto H, Yamazaki A, Tanegashima K, Edamura K. Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog. https://www.openveterinaryjournal.com/?mno=85525 [Access: January 25, 2026]. doi:10.5455/OVJ.2021.v11.i4.25 AMA (American Medical Association) Style Tomo Y, Sobashima E, Eto H, Yamazaki A, Tanegashima K, Edamura K. Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog. Open Vet. J.. 2021; 11(4): 728-733. doi:10.5455/OVJ.2021.v11.i4.25 Vancouver/ICMJE Style Tomo Y, Sobashima E, Eto H, Yamazaki A, Tanegashima K, Edamura K. Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog. Open Vet. J.. (2021), [cited January 25, 2026]; 11(4): 728-733. doi:10.5455/OVJ.2021.v11.i4.25 Harvard Style Tomo, Y., Sobashima, . E., Eto, . H., Yamazaki, . A., Tanegashima, . K. & Edamura, . K. (2021) Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog. Open Vet. J., 11 (4), 728-733. doi:10.5455/OVJ.2021.v11.i4.25 Turabian Style Tomo, Yuma, Erina Sobashima, Hinano Eto, Atsushi Yamazaki, Koji Tanegashima, and Kazuya Edamura. 2021. Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog. Open Veterinary Journal, 11 (4), 728-733. doi:10.5455/OVJ.2021.v11.i4.25 Chicago Style Tomo, Yuma, Erina Sobashima, Hinano Eto, Atsushi Yamazaki, Koji Tanegashima, and Kazuya Edamura. "Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog." Open Veterinary Journal 11 (2021), 728-733. doi:10.5455/OVJ.2021.v11.i4.25 MLA (The Modern Language Association) Style Tomo, Yuma, Erina Sobashima, Hinano Eto, Atsushi Yamazaki, Koji Tanegashima, and Kazuya Edamura. "Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog." Open Veterinary Journal 11.4 (2021), 728-733. Print. doi:10.5455/OVJ.2021.v11.i4.25 APA (American Psychological Association) Style Tomo, Y., Sobashima, . E., Eto, . H., Yamazaki, . A., Tanegashima, . K. & Edamura, . K. (2021) Treatment of methicillin-resistant Staphylococcus aureus infection following tibial plateau leveling osteotomy in a dog. Open Veterinary Journal, 11 (4), 728-733. doi:10.5455/OVJ.2021.v11.i4.25 |