| Case Report | ||
Open Vet. J.. 2022; 12(6): 1035-1038 Open Veterinary Journal, (2022), Vol. 12(6): 1035–1038 Case Report Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstructionFrancesco Santoro* and Johanna KaartinenDepartment of Clinical Sciences and Services, The Royal Veterinary College, Hatfield, UK Submitted: 12/09/2022 Accepted: 22/11/2022 Published: 22/12/2022 *Corresponding Author: Francesco Santoro. Department of Clinical Sciences and Services, The Royal Veterinary College, Hatfield, UK. Email: doc.tabarez [at] gmail.com © 2022 Open Veterinary Journal
AbstractBackground: Alpacas are becoming more and more diffused as pets in Europe and United Kingdom, and it is not uncommon to deal with these species in large animal referral hospitals. Unfortunately, pain assessment and treatment in llamoids remain challenging, due to their instinct of hiding signs of pain and the lack of relevant scientific literature. Case Description: This report describes the use of an ultrasound-guided brachial plexus block as part of a multimodal analgesic strategy in an alpaca undergoing surgical right shoulder luxation repair. Based on the intra-operative cardiovascular stability, the post-operative comfort level, and the minimal amount of systemic analgesics needed, it can be concluded that the block appeared effective and contributed to the peri-operative pain management. After recovery from general anesthesia, drooping of the right upper eyelid was observed and persisted for approximately 10 hours. This finding could be interpreted as a Horner’s syndrome-like clinical sign and be a minor complication of the block, as previously described in other species. Conclusion: Despite the minor complication here reported, and the difficulty in assessing intra- and post-operative nociception and pain in camelids, it can be concluded that the use of a brachial plexus block could be a valuable option when desensitization of the forelimb is required. Keywords: Alpaca, Anesthesia, Analgesia, Acute pain, Regional anesthesia. IntroductionDespite their diffusion as pets during the last decades, and the increased level of veterinary care provided, pain assessment and treatment in alpacas (and camelids in general) remain challenging. In fact, the lack of species-specific validated pain scales, the potential for side effects related to the most effective and common analgesics, the scant amount of available literature, and the legal classification of these animals as food-producing species in some countries, are all issues to be addressed when planning an analgesic protocol for this species (Smith et al., 2021). The use of local and regional anesthetic techniques in small animals, like in people, is associated with numerous advantages such as better analgesic quality, reduction of peri-operative stress response, and lower total doses of administered intra- and post-operative systemic analgesics (Richman et al., 2006; Romano et al., 2016). Several recently published case reports and series describe the successful use of loco-regional anesthesia in alpacas undergoing various surgical procedures (Stathopoulou et al., 2019; Fackler et al., 2020; Foster et al., 2020). This case report describes the performance and efficacy of an ultrasound-guided brachial plexus block in an alpaca undergoing surgical scapulo-humeral sub-luxation reduction and articular capsule repair, and the suspect of ipsilateral Horner’s syndrome post-operatively. Case DetailsA 60 kg 2-year-old male huacaya alpaca was presented to the Equine Referral Hospital of the Royal Veterinary College with 1 week history of traumatic right acromial fracture with resulting scapulo-humeral luxation, diagnosed radiographically by the referring veterinary surgeon. At the time of admission, the only relevant clinical sign was moderate right forelimb lameness, and the animal was classified as ASA II (American Society of Anesthesiologists Physical Status Classification System) based on history and clinical evaluation. Informed consent for all the procedures performed was signed by the owner during admission. Immediately following the orthopedic examination, analgesia was provided with meloxicam IV (0.5 mg/kg; Metacam 20 mg/ml, Boehringer Ingelheim, UK). A computed tomography (CT) was performed under general anesthesia to assess the trauma and plan the surgical technique. This exam confirmed the presence of complete displaced comminuted subacute fracture of the acromion and luxation of the shoulder.2 days after the CT exam, the animal underwent surgery under general anesthesia. No pre-operative starvation period was observed, as hay remained available in the barn until last minute. The pre-anesthetic clinical examination was normal. Routine pre-operative blood tests showed a packed cell volume of 26%, and routine biochemistry results all within reference intervals. After IV premedication with methadone (0.1 mg/kg; Synthadon 10 mg/ml; Animal Care, UK) and xylazine (0.6 mg/kg; Chanazine 10%, Chanelle Pharma Group, Ireland), general anesthesia was induced with a mixture of ketamine (2.5 mg/kg; Ketamidor 100 mg/ml, Chanelle Pharma Group, Ireland) and midazolam (0.2 mg/kg; Dormazolam 5 mg/ml, Dechra, UK) administered IV. Endotracheal intubation was quickly performed with a size 7 mm silicone endotracheal tube guided by a flexible stylet, the animal was transferred on the surgical table, placed on left lateral recumbency for surgical preparation, and connected to the anesthetic machine (Tafonius Junior, Vetronic Services Ltd., UK). General anesthesia was maintained with isoflurane (Isofane, Piramal Critical Care Ltd., UK) in 80% oxygen and Hartmann’s solution was infused at the rate of 5 ml/kg/hour during the entire duration of the procedure. The following vital parameters were measured by an anesthetic monitor (Carescape Monitor B450, GE Healthcare, UK) and recorded every 5 minutes on the anesthetic record: heart, pulse, and respiratory rate, electrocardiogram, invasive blood pressure (via a 20 g IV catheter placed in the right auricular artery), capnography, inspired fraction, and end tidal concentration of isoflurane and oxygen, pulse oximetry, Esophageal temperature, and spirometry.
Fig. 1. Ultrasound guided brachial plexus block. Orientation of the ultrasound probe (covered by a sterile glove filled with conductive gel) and the sono-reflectant needle immediately before the execution of the block. In lateral recumbency, after trichotomy and surgical scrub of the area, the brachial plexus was localized at the level of the right axilla using a 13-6 MHz linear ultrasound transducer (SonoSite Edge, FUJIFILM Sonosite, Netherlands) (Fig. 1), and a total volume of 16 ml of ropivacaine 0.75% (2 mg/kg, Naropine, AstraZeneca, UK) was injected perineurally under ultrasound-guidance (Fig. 2). Intermittent positive pressure ventilation was provided for the whole duration of the procedure, with a set tidal volume of 0.6 l and a respiratory rate between 12 and 15 breaths per minutes, aimed at maintaining normocapnia (end-tidal CO2 between 35 and 45 mmHg). An open luxation reduction with tension suture placement was then performed. The duration of surgery was 140 minutes, and no rescue analgesic treatment was needed at any point, based on a lack of significant (more than 20% above the pre-incisional baseline) variation of heart rate and arterial blood pressure or sudden dyssynchrony between the animal and the ventilator. End-tidal isoflurane was maintained between 1.1% and 1.3%, and 35 minutes after the first incision, following a decrease of mean arterial blood pressure below 60 mmHg, a constant rate of dobutamine (0.5–1 mcg/kg/minutes; dobutamine 12.5 mg/ml, Hameln Pharma Ltd., UK) was started to restore normotension. Esophageal temperature was 36°C at the time of first incision, and 35°C immediately before recovery.
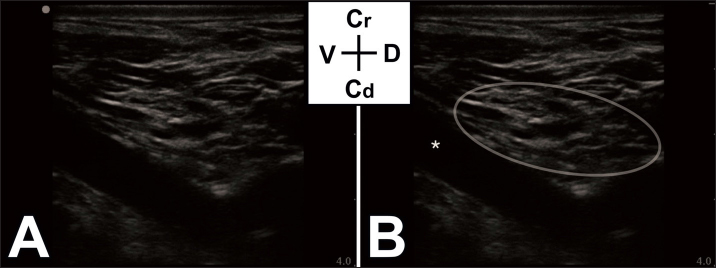
Fig. 2. (A): Ultrasound image of the brachial plexus, obtained at the level of the chosen acoustic window. (B): Same image with added landmarks. Ellipse – target area of the brachial plexus. Asterisk – carotid artery. During general anesthesia, both eyes were protected with a thick layer of ophthalmic gel (Viscotears Liquid Gel, Bausch & Lomb U.K Limited, UK) applied on the globes every hour. After placement of a Velpeau bandage, general anesthesia was discontinued, and the animal was transferred into recovery box. During this phase, the head was constantly sustained in a straight vertical position and kept slightly tilted downwards to allow drainage of the saliva. When the swallowing reflex returned and the animal was deemed able to hold its head spontaneously, the endotracheal tube was removed with its cuff partially inflated. After 20 minutes of clinical monitoring, the alpaca was moved back to the barn, where it was reunited with its companion (another alpaca of the same owner). Following extubation, right ptosis (drooping of the upper eyelid) was noticed. A brief examination of the right eye was performed by the clinician in charge, and nothing grossly abnormal was detected. Recovery from general anesthesia was smooth and rapid, pain was subjectively assessed by the hospital staff, due to the lack of validated scales in this species, and no rescue analgesia was needed during the whole hospitalization time. Meloxicam was continued at the same aforementioned dose for 10 days post-operatively. On the morning following surgery, right ptosis had fully resolved. The animal was discharged after 28 days, and the entire hospitalization period was uneventful. DiscussionBased on the intra-operative cardiovascular stability, post-operative low apparent pain level and overall comfort of the animal, the regional block, here reported for the first time in this species, seems to have provided an adequate level of intra- and post-operative analgesia. However, considering the lack of validated pain scales in camelids, the level at which the plexus was blocked, and the concurrent use of other drugs with analgesic properties, these findings should be interpreted cautiously. Pain was assessed subjectively, based on observation of behaviors such as food ingestion and overall gastro-intestinal function, interaction with its companion and the hospital staff, degree of mobility, and comfort when recumbent. This subjective assessment showed a high level of post-operative comfort and lack of pain-associated behaviors. Horner’s syndrome results from a dysfunction of the efferent sympathetic nervous system to the eye anywhere along its three-neuron pathway, from the hypothalamus and midbrain to the globe. The main clinical signs include enophthalmos, ptosis, miosis, and protrusion of the nictitating membrane. In large animals, further clinical signs include: facial/neck sweating (in horses), hyperthermia of the facial area, anhidrosis of the planum nasolabial (in cattle), and hyperthermia of the ear (in ruminants) (de Lahunta et al., 2020). Horner syndrome (partial or complete) has been reported as a potential consequence of brachial plexus block in people and dogs, as a result of a dorsal spread of local anesthetic and blockade of structures such as the thoracc sympathetic trunk, the cervicothoracic and middle cervical ganglia, and the vagosympathetic trunk (Stasiowski et al., 2018; Zwueste and Grahn, 2019). To the best of our knowledge, the presence of all the typical clinical signs of Horner’s syndrome has never been reported in alpacas. Interestingly, similarly to the case described here, in one clinical report in which severe otitis media and interna were diagnosed, ipsilateral ptosis was the only clinical sign potentially attributable to a lesion of the nerves involved in this syndrome (Galvan et al., 2013). An important limitation in this report is the absence of a complete ophthalmic examination performed by a board-certified specialist, although other macroscopic abnormalities were not detected by the clinicians in charge.The hypotheses of the post-operative Horner’s syndrome could also correlate with the clinical efficacy of this block despite the distal approach used. In fact, in order to provide complete somatic desensitization, a regional blockade should aim for nerve structures proximal to the surgical area. In this case, the sono-anatomy of the brachial plexus was evaluated beforehand, and the injection site was chosen based on the best obtained image (with most of the target nerves adjacent and within the same fascial plane), although this being at the same level, or even slightly distal to the scapulo-humeral joint. A possible explanation for both the clinical efficacy of the technique and the neurological deficit observed post-operatively is the high total injected volume of undiluted local anesthetic, which may have migrated more proximally (dorsally) by following and surrounding the nerves involved in the plexus. Horner’s syndrome can be considered a minor complication, as it does not result in any short- or long-term organ damage or impairment and it resolves within hours (Zwueste and Grahn, 2019). Nevertheless, a reduction of the injectate volume and/or a more distal approach to the brachial plexus could result in a lower incidence of this undesired neurological deficit. For the regional block described here, ropivacaine was the local anesthetic of choice, in virtue of a lower toxicity and only slightly shorter duration of action when compared to bupivacaine (Feldman et al., 1989; Simpson et al., 2005). However, it is important to consider how data about pharmacodynamics and toxic dose of local anesthetics are currently lacking for this species. ConclusionUltrasound-guided brachial plexus block with axillary approach may be an effective adjunctive intra- and post-operative analgesic treatment in alpacas undergoing shoulder surgery. Ipsilateral Horner’s syndrome (partial or complete) should be considered as a possible complication of the described block, in case of dorsal spread of the local anesthetic. AcknowledgmentsThe authors received no financial support for the research, authorship, and/or publication of this article. Conflict of interestThe authors declare that they have no conflict of interest. Author contributionsF.S. and J.K. were involved in execution of the block, clinical case management, and manuscript writing/editing. Referencesde Lahunta, A., Glass, E. and Kent, M. 2020. De Lahunta’s veterinary neuroanatomy and clinical neurology, 5th ed. Amsterdam, The Netherlands: Elsevier. Fackler, B.M., Portela, D.A., Romano, M. and Gatson, B.J. 2020. Use of distal radial, ulnar, median and musculocutaneous (RUMM) nerve blocks in a Huacaya alpaca undergoing radial fracture repair. Vet. Anesth. Analg. 5, 734–736. Feldman, H.S., Arthur, R. and Covino, B.G. 1989. Comparative systemic toxicity of convulsant and supraconvulsant doses of intravenous ropivacaine, bupivacaine, and lidocaine in the conscious dog. Anesth. Analg. 69, 794–801. Foster, A., McSloy, A. and Monticelli, P. 2020. Ultrasound-guided psoas compartment and sciatic nerve blocks for pain management of hind limb procedures in the alpaca (Vicugna pacos). Open. Vet. J. 10, 120–127. Galvan, N., Middleton, J.R., Cook, C., Britt, L.G. and Kuroki, K. 2013. Otitis interna, media, and externa with destruction of the left tympanic bulla and subluxation and septic arthritis of the left temporomandibular joint in an alpaca (Vicugna pacos). Can. Vet. J. 54, 283–285. Richman, J.M., Liu, S.S., Courpas, G., Wong, R., Rowlingson, A.J., McGready, J., Cohen, S.R. and Wu, C.L. 2006. Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth. Analg. 102, 248–257. Romano, M., Portela, D.A., Breghi, G. and Otero, P.E. 2016. Stress-related biomarkers in dogs administered regional anaesthesia or fentanyl for analgesia during stifle surgery. Vet. Anaesth. Analg. 43, 44–54. Simpson, D., Curran, M.P., Oldfield, V. and Keating, G.M. 2005. Ropivacaine: a review of its use in regional anaesthesia and acute pain management. Drugs 65, 2675–2717. Smith, J.S., Schleining, J. and Plummer, P. 2021. Pain management in small ruminants and Camelids analgesic agents. Vet. Clin. Food. Anim. 37, 1–16. Stasiowski, M., Zuber, M., Marciniak, R., Kolny, M., Chabierska, E., Jalowiecki, P., Pluta, A. and Missir, A. 2018. Risk factors for the development of Horner’s syndrome following interscalene brachial plexus block using ropivacaine for shoulder arthroscopy: a randomised trial. Anaesthesiol. Intensive. Ther. 50, 215–220. Stathopoulou, T., Seymour, C., McSloy, A., Adams, J. and Viscasillas, J. 2019. Pain management of a mandibular fracture in an alpaca via epidural catheter placement in the mandibular foramen. Vet. Rec. 7, e000863. Zwueste, D.M. and Grahn, B.H. 2019. A review of Horner’s syndrome in small animals. Can. Vet. J. 60, 81–88. | ||
| How to Cite this Article |
| Pubmed Style Santoro F, Kaartinen J. Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.. Open Vet. J.. 2022; 12(6): 1035-1038. doi:10.5455/OVJ.2022.v12.i6.32 Web Style Santoro F, Kaartinen J. Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.. https://www.openveterinaryjournal.com/?mno=112612 [Access: November 22, 2025]. doi:10.5455/OVJ.2022.v12.i6.32 AMA (American Medical Association) Style Santoro F, Kaartinen J. Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.. Open Vet. J.. 2022; 12(6): 1035-1038. doi:10.5455/OVJ.2022.v12.i6.32 Vancouver/ICMJE Style Santoro F, Kaartinen J. Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.. Open Vet. J.. (2022), [cited November 22, 2025]; 12(6): 1035-1038. doi:10.5455/OVJ.2022.v12.i6.32 Harvard Style Santoro, F. & Kaartinen, . J. (2022) Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.. Open Vet. J., 12 (6), 1035-1038. doi:10.5455/OVJ.2022.v12.i6.32 Turabian Style Santoro, Francesco, and Johanna Kaartinen. 2022. Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.. Open Veterinary Journal, 12 (6), 1035-1038. doi:10.5455/OVJ.2022.v12.i6.32 Chicago Style Santoro, Francesco, and Johanna Kaartinen. "Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.." Open Veterinary Journal 12 (2022), 1035-1038. doi:10.5455/OVJ.2022.v12.i6.32 MLA (The Modern Language Association) Style Santoro, Francesco, and Johanna Kaartinen. "Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.." Open Veterinary Journal 12.6 (2022), 1035-1038. Print. doi:10.5455/OVJ.2022.v12.i6.32 APA (American Psychological Association) Style Santoro, F. & Kaartinen, . J. (2022) Ultrasound-guided brachial plexus block and suspected Horner’s syndrome in an alpaca (Vicugna pacos) undergoing traumatic scapulo-humeral luxation reduction and articular capsule reconstruction.. Open Veterinary Journal, 12 (6), 1035-1038. doi:10.5455/OVJ.2022.v12.i6.32 |